- Department of Neurosurgery, Loma Linda University Medical Center, Loma Linda, California, United States.
- Department of Neurosurgery, School of Medicine, Loma Linda University School of Medicine, Loma Linda, California, United States.
* Both of these authors contributed equally.
Correspondence Address:
Emmanuel Omosor, School of Medicine, Loma Linda University School of Medicine, 11175 Campus Street, Loma Linda-92350, California, United States.
DOI:10.25259/SNI_496_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Taylor Anne Wilson1, Ramachandran Pillai Promod Kumar1, Emmanuel Omosor2. Thoracic ventral spinal cord herniation with progressive myelopathy – A case report and review of the literature. 03-Aug-2021;12:382
How to cite this URL: Taylor Anne Wilson1, Ramachandran Pillai Promod Kumar1, Emmanuel Omosor2. Thoracic ventral spinal cord herniation with progressive myelopathy – A case report and review of the literature. 03-Aug-2021;12:382. Available from: https://surgicalneurologyint.com/surgicalint-articles/11022/
Abstract
Background: Idiopathic spinal cord herniation (ISCH) is a rare, underrecognized, and often misdiagnosed entity of unclear pathogenesis that typically presents as a slowly progressive thoracic myelopathy. There are less than 200 such cases reported in the literature. ISCH diagnosis and treatment are often delayed contributing to greater fixed neurological deficits, often leading to costly, unnecessary imaging studies, and inappropriate surgery.
Case Description: Here, a 48-year-old female presented with trauma-induced ISCH characterized by gradually worsening lower extremity myelopathy.
Conclusion: Idiopathic spinal cord herniation (ISCH) is rare, often underdiagnosed posttraumatic myelopathy that, when accurately diagnosed and treated, can result in good outcomes.
Keywords: Cerebral palsy, Myelopathy, Spinal cord herniation
INTRODUCTION
Idiopathic spinal cord herniation (ISCH), also called ventral spinal cord herniation (VSCH), is a rare and often underdiagnosed cause of slowly progressive thoracic myelopathy. It involves anterior or anterolateral displacement of spinal cord tissue through a small, ventral dural defect most typically arising in the upper/mid thoracic spine between the T2-T8 levels.[
CASE DESCRIPTION
A 48-year-old female presented 3 years after being thrown against a wall with a sequela of traumatic brain injury (TBI) with cerebral palsy, worsening myelopathy, and gait ataxia. She initially utilized a walker for ambulation, but progressed to wheelchair bound by the time of presentation [
Diagnostic studies
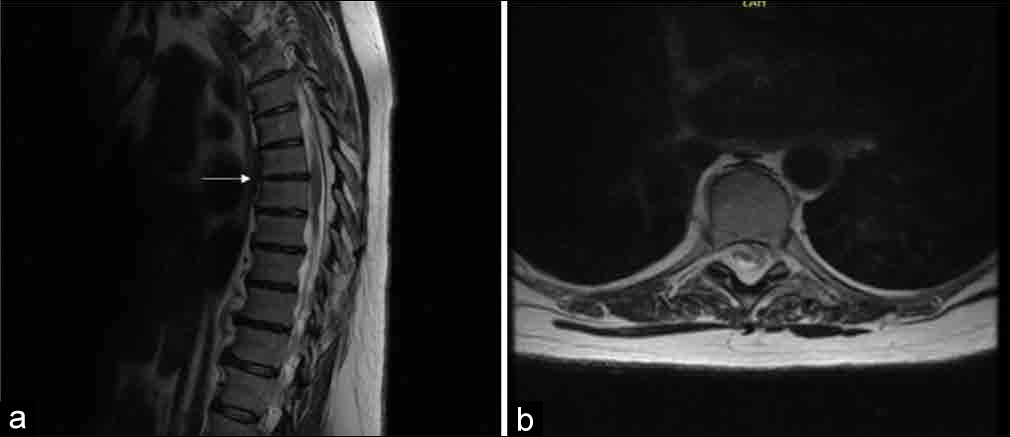
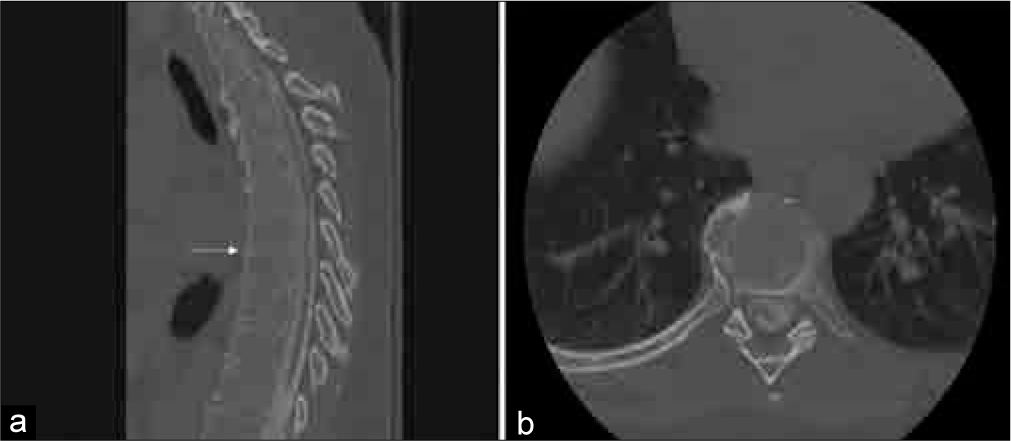
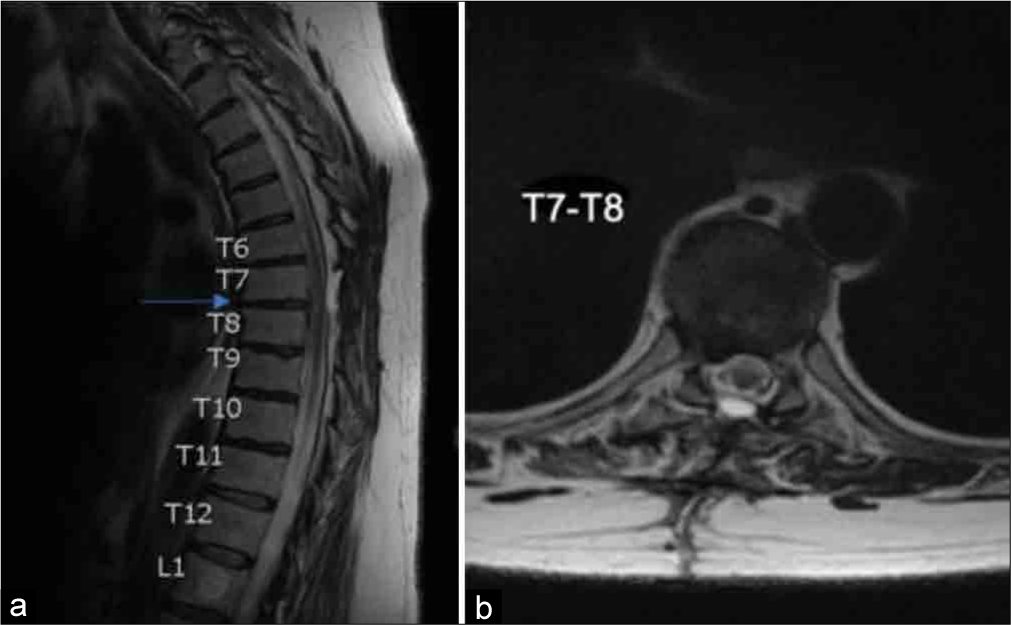
She underwent MRI studies of the brain and spine, plus EMG and NCV of the lower extremities. The thoracic MRI showed a ventral thecal sac irregularity with accompanying distortion of the ventral cord, consistent with “tethering;” cervical and lumbar studies were unremarkable [
Surgery
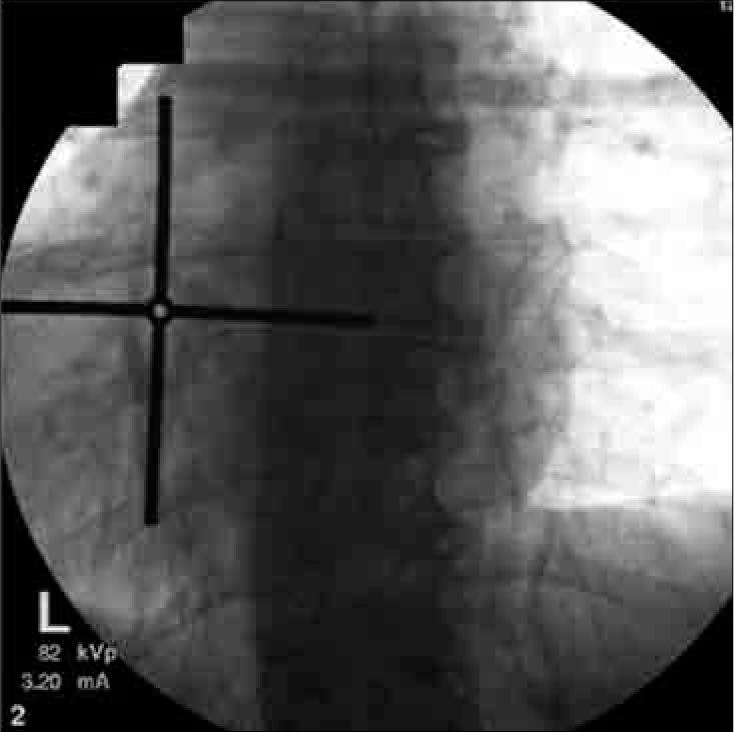
We performed a T7-T8 laminectomy and unilateral facetectomy with removal of the right T7 pedicle and transverse process, exposing the T7-8 nerve roots [
Follow-up
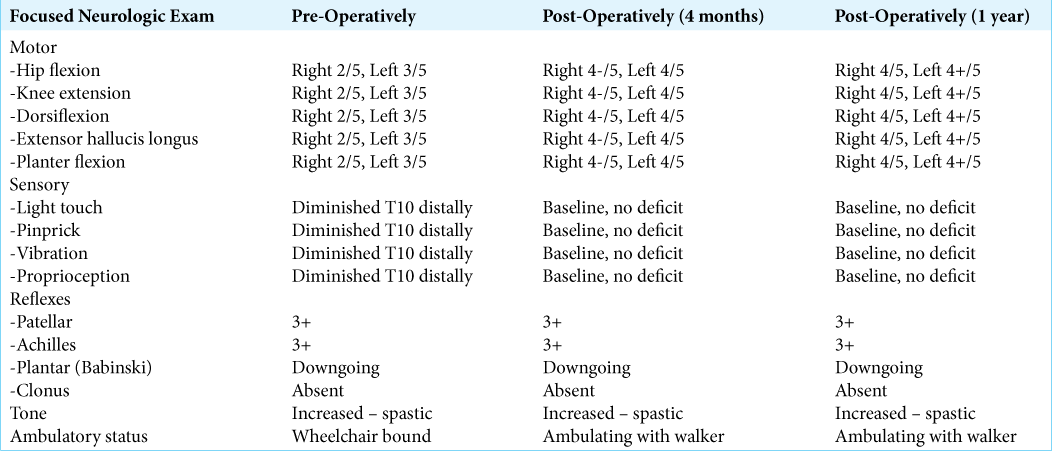
Postoperatively, the patient went to rehab and within 2 months, she was ambulating with assistance using a walker. Her strength continued to improve at her 4-month and 1-year neurosurgical follow-up visits [
DISCUSSION
ISCH is a rare cause of progressive thoracic myelopathy. Females are affected nearly twice as frequently as males.[
Patients are typically in their fifties (range 12–80 years of age).[
Etiology
Several hypotheses exist regarding the pathogenesis of ISC. In 1974, Wortzman et al. described a patient with a gradually worsening spastic paraplegia due to a congenital myelocele.[
Variable neurological presentation
Characteristically, ISCH leads to gradual onset of lower extremity myelopathy and spastic paresis; however, 60–75% of patients present with Brown-Sequard syndrome, while others develop asymmetric/symmetric lower extremity spastic paresis. Other symptoms/signs include 70% incidence of neck/upper back pain and 10% frequency of bladder dysfunction.[
Diagnostic MR or Myelo-CT studies
Thin cut thoracic spine MRI is the gold standard for diagnosing ISCH. These studies typically show a C-shaped ventral kink or displacement of the thoracic cord adjacent to the dural defect.[
Outcomes with early surgery
Earlier operative intervention has better prognoses/ outcomes.[
Operative intervention requires direct repair of the dural defect, reduction of the cord into the canal, and detethering adhesions.[
Dural closure methods
Dural repair techniques for ISCH include primary repair versus duraplasty. Primary repair is often considered more secure; however, it may contribute to thecal sac stenosis and greater postoperative neurological deficits due to pressure around the cord. Conversely, duraplasty minimizes the risk of inadvertent spinal cord manipulation and the related postoperative neurological dysfunction, but introduces a foreign material into the patient.[
CONCLUSION
ISCH is rare, often underdiagnosed posttraumatic myelopathy that, when accurately diagnosed and treated, can result in good outcomes.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Batzdorf U, Holly LT. Idiopathic thoracic spinal cord herniation: Report of 10 patients and description of surgical approach. J Spinal Disord Tech. 2012. 25: 157-62
2. Carter BJ, Griffith BD, Schultz LR, Abdulhak MM, Newman DS, Jain R. Idiopathic spinal cord herniation: An imaging diagnosis with a significant delay. Spine J. 2015. 15: 1943-8
3. Darbar A, Krishnamurthy S, Holsapple JW, Hodge CJ. Ventral thoracic spinal cord herniation: Frequently misdiagnosed entity. Spine (Phila Pa 1976). 2006. 31: E600-5
4. Delgado-López PD, Gil-Polo C, Martín-Velasco V, Martín-Alonso J, Galacho-Harriero AM, Araus-Galdós E. Spinal cord herniation repair with microstaples: Case report. J Neurosurg Spine. 2017. 26: 384-7
5. Ghali MGZ, Srinivasan VM, Rao VY, Omeis I. Idiopathic thoracic spinal cord herniation. J Clin Neurosci. 2018. 51: 1-5
6. Goetti R, Wille D, Kretzschmar U, Klein A, Scheer I. Idiopathic spinal cord herniation: First reported case in a child. JAMA Neurol. 2013. 70: 125-6
7. Kasliwal MK, O’toole JE, Deutsch H. Unilateral paramedian transpedicular approach for repair of anterior transdural spinal cord herniation: Report of a case and literature review. Asian Spine J. 2012. 6: 55-9
8. Marshman LA, Hardwidge C, Ford-Dunn SC, Olney JS. Idiopathic spinal cord herniation: Case report and review of the literature. Neurosurgery. 1999. 44: 1129-33
9. Payer M, Zumsteg D, de Tribolet N, Wetzel S. Surgical management of thoracic idiopathic spinal cord herniation. Technical case report and review. Acta Neurochir (Wien). 2016. 158: 1579-82
10. Saito A, Takahashi T, Sato S, Kumabe T, Tominaga T. Modified surgical technique for the treatment of idiopathic spinal cord herniation. Minim Invasive Neurosurg. 2006. 49: 120-3
11. Uhl E, Holtmannspötter M, Tonn JC. Improvement of Brown-Sequard syndrome after surgical repair of an idiopathic thoracic spinal cord herniation. J Neurol. 2008. 255: 125-6
12. Wortzman G, Tasker RR, Rewcastle NB, Richardson JC, Pearson FG. Spontaneous incarcerated herniation of the spinal cord into a vertebral body: A unique cause of paraplegia. Case report. J Neurosurg. 1974. 41: 631-5