- Department of Neurosurgery, Iran University of Medical Sciences, Tehran, Iran.
DOI:10.25259/SNI_548_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Alireza Tabibkhooei, Alireza Sadeghipour, Arash Fattahi. Thoracolumbar pilomyxoid astrocytoma concomitant with spinal scoliosis: A case report and literature review. 06-Dec-2019;10:235
How to cite this URL: Alireza Tabibkhooei, Alireza Sadeghipour, Arash Fattahi. Thoracolumbar pilomyxoid astrocytoma concomitant with spinal scoliosis: A case report and literature review. 06-Dec-2019;10:235. Available from: http://surgicalneurologyint.com/surgicalint-articles/9788/
Abstract
Background: Pilomyxoid astrocytoma (PMA) is a variant of pilocytic astrocytomas but exhibits more aggressive behavior. Further, it is more prevalent in the hypothalamic/chiasmatic regions and is only rarely encountered in the thoracic spine.
Case Description: A 9-year-old male presented with severe spastic paraparesis (motor/sensory) attributed to a thoracic cord PMA and scoliosis. The magnetic resonance (MR) showed an intraaxial ill-defined expansile lesion with heterogeneous enhancement extending from the cervicothoracic junction to conus medullaris. A multilevel decompressive laminectomy was performed with restricted tumor debulking; an expansile duraplasty was also effected. Two years later, the patient has moderately improved and has not shown any symptom progression.
Conclusion: We recommend the early performance of a thoracic MR in children with idiopathic scoliosis presenting with the onset of a significant spastic paraparesis.
Keywords: Magnetic resonance imaging, Pilomyxoid astrocytoma, Radiotherapy, Scoliosis, Spinal cord, Thoracic
BACKGROUND
Intramedullary pilomyxoid astrocytoma (PMA) is a variant of pilocytic astrocytoma (PA).[
CASE PRESENTATION
A 9-year-old male with spinal scoliosis recently diagnosed/brace (e.g., 1 month’s duration) presented with a severe motor/sensory spastic paraparesis. The holospinal magnetic resonance (MR) revealed an intraaxial/intramedullary ill-defined expansile lesion with heterogeneous enhancement extending from the cervicothoracic junction to conus medullaris [
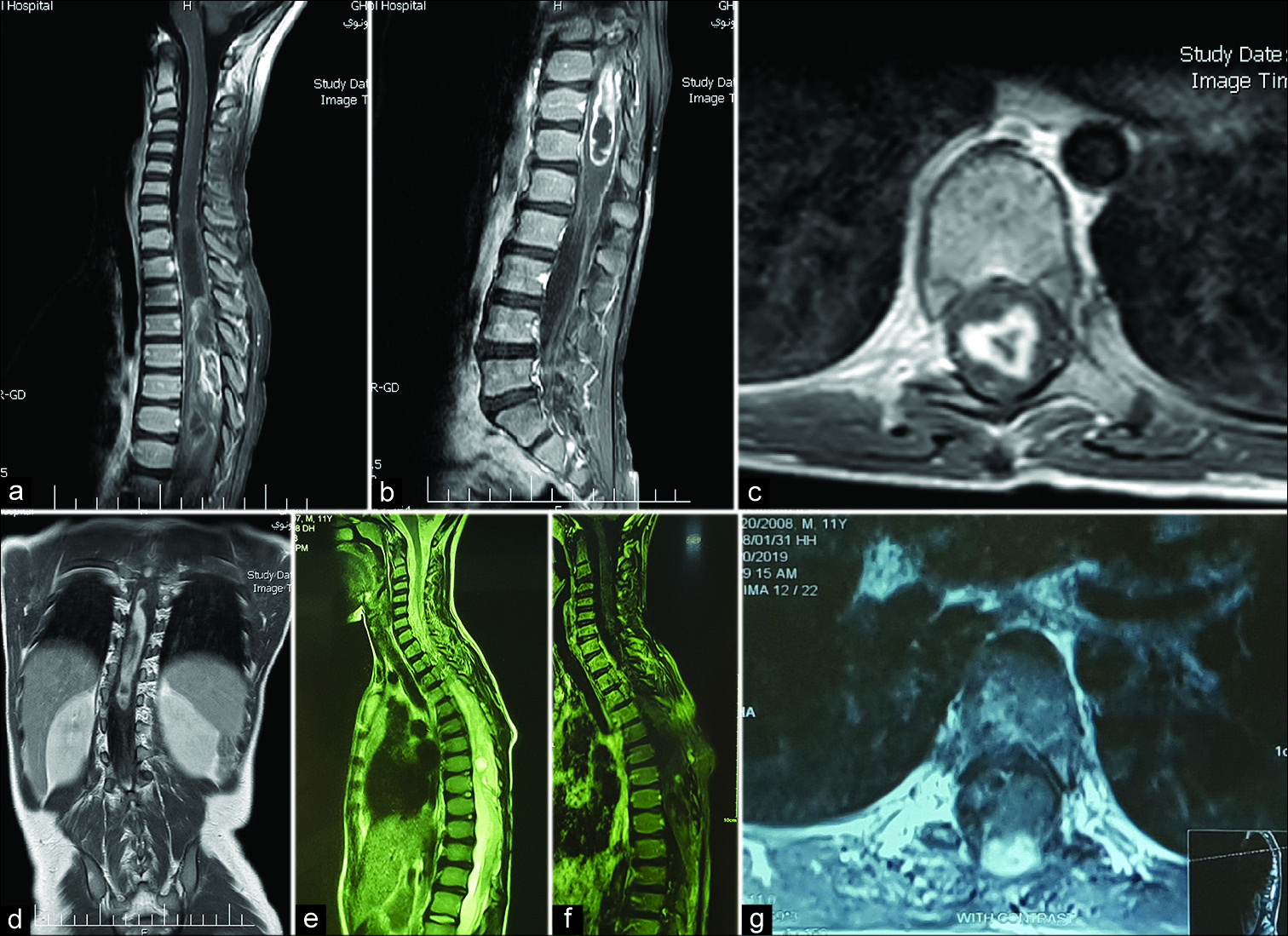
Figure 1:
Preoperative magnetic resonance imaging (MRI) with gadolinium showed an expansile intramedullary tumor of thoracic cord and conus medullaris with irregular heterogeneous enhancement and some cystic changes on sagittal (a and b) and axial (c) views in a 9-year-old patient with severe thoracolumbar scoliosis (d). After surgical treatment, 2 years follow-up MRI reveals an evidence of minimal cord herniation toward laminectomy sites and intramedullary cystic changes (sagittal T2 sequence), (e) with minimal enhancement on sagittal (f) and axial (g) views.
He underwent a T5-T11 laminectomy with tumor debulking (e.g., poor plane between tumor/cord) followed by expansile duraplasty. Postoperatively, he exhibited significant improvement of the paraparesis. As the histopathological exam showed a PMA, adjuvant therapy included spinal radiation [
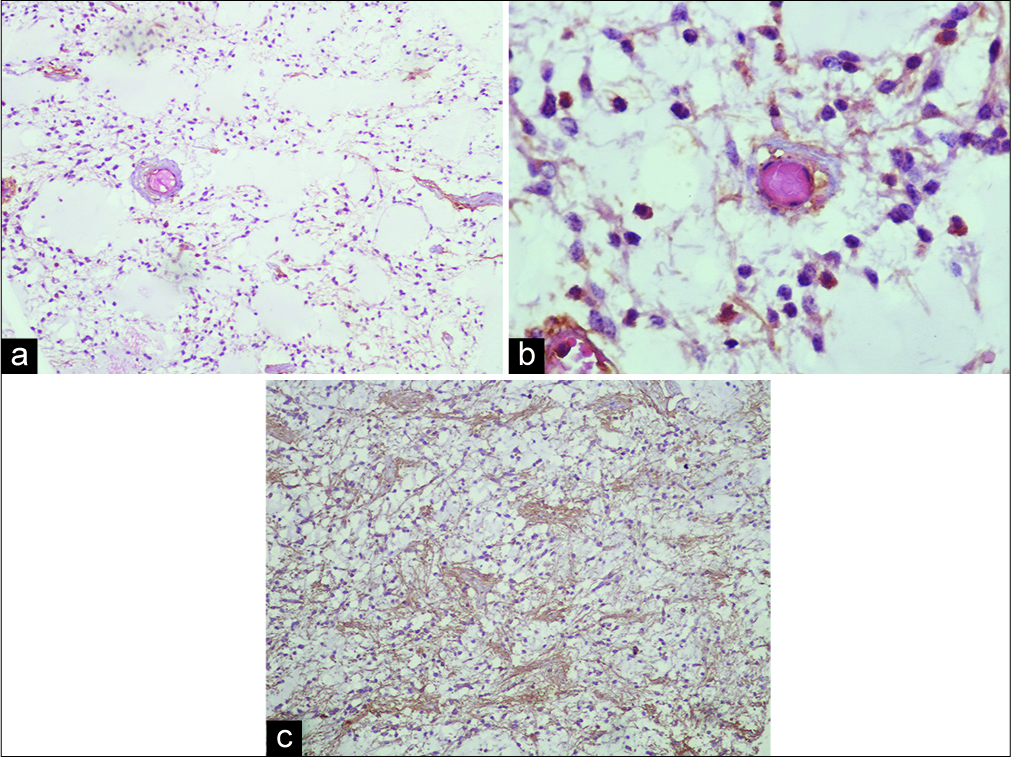
Figure 2:
This shows histopathology of resected tumor. We could see hypocellular glial tumor, in which monomorphic piloid tumor cells are dispersed in a myxoid matrix (Hematoxylin and Eosin stain, ×100) (a). Furthermore, tendency of piloid perivascular cells to form a rosette-like structure without any Rosenthal fiber could be seen (Hematoxylin and Eosin stain, ×400, b). (c) Reveals a strong immunoreactivity of the tumor cells for glial fibrillary acidic protein (GFAP immunostaining, ×100, c).
DISCUSSION
PMA is the more aggressive type of astrocytoma that usually seen in child <4-year-old age and in hypothalamic/chiasmatic region.[
On imaging, we have no any distinct criteria for differentiation of PA from PMA.[
Usually, in cases of intramedullary astrocytoma, we recommend only debulking the center of tumor (e.g., not beyond the ill-defined border between tumor/normal tissue), and then performing an expansile duraplasty, if indicated.
The addition of adjuvant radiation therapy is controversial. Many clinicians recommend safe surgical resection of the tumor followed by both radiotherapy and chemotherapy to improve survival.[
CONCLUSION
We present the rare case of a 9-year-old with a PMA of the thoracic cord and scoliosis who was effectively treated with a T5-T11 laminectomy, tumor debulking, duraplasty, and later adjuvant radiation therapy.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
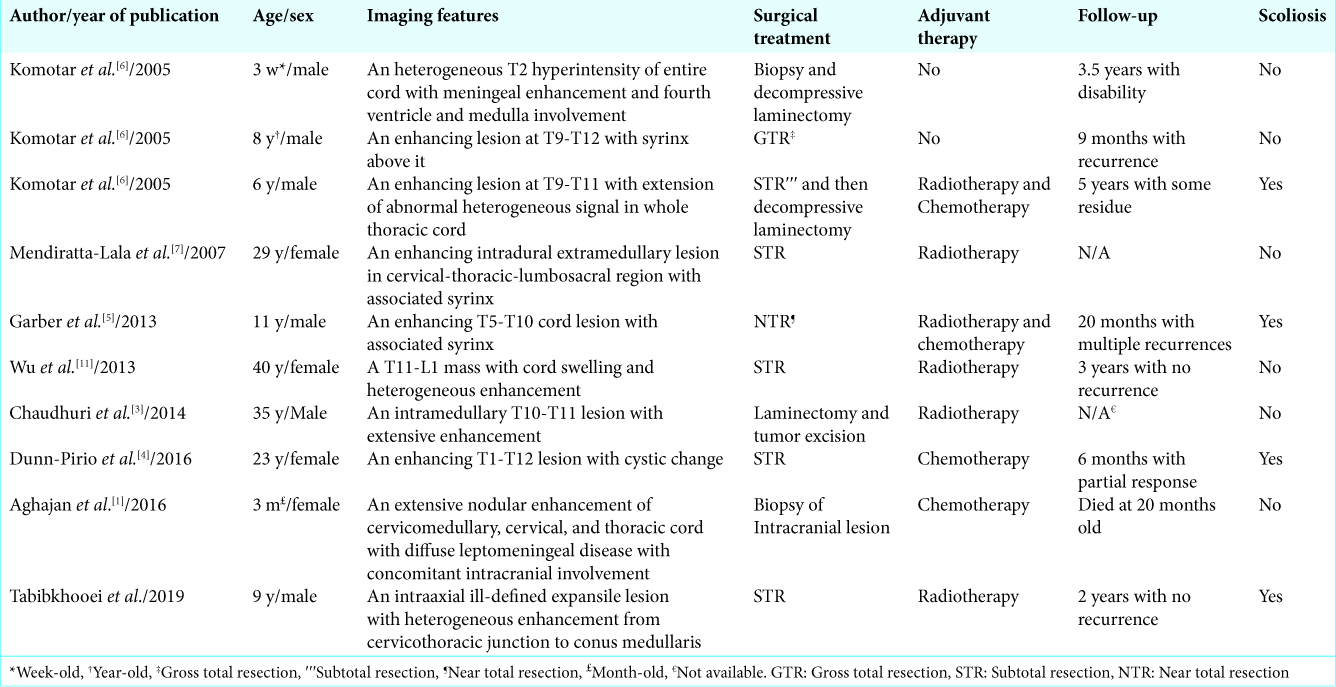
References
1. Aghajan Y, Levy ML, Newbury RO, Crawford JR. Disseminated pilomyxoid astrocytoma in infancy with novel MUTYH mutation. BMJ Case Rep. 2016. 2016: bcr2016217764-
2. Bouaziz MC, Daghfous MS, Ladeb MF. Childhood scoliosis revealing spinal cord tumors. Eur Orthop Surg Traumatol. 2006. 16: 318-21
3. Chaudhuri T, Jadava K. Pilomyxoid astrocytoma of the thoracic spinal cord in an adult: A case report and review of literature. Clin Cancer Invest J. 2014. 3: 329-
4. Dunn-Pirio AM, Howell E, McLendon RE, Peters KB. Single-agent carboplatin for a rare case of pilomyxoid astrocytoma of the spinal cord in an adult with neurofibromatosis Type 1. Case Rep Oncol. 2016. 9: 568-73
5. Garber ST, Bollo RJ, Riva-Cambrin JK. Pediatric spinal pilomyxoid astrocytoma. J Neurosurg Pediatr. 2013. 12: 511-6
6. Komotar RJ, Carson BS, Rao C, Chaffee S, Goldthwaite PT, Tihan T. Pilomyxoid astrocytoma of the spinal cord: Report of three cases. Neurosurgery. 2005. 56: 191-
7. Mendiratta-Lala M, Kader Ellika S, Gutierrez JA, Patel SC, Jain R. Spinal cord pilomyxoid astrocytoma: An unusual tumor. J Neuroimaging. 2007. 17: 371-4
8. Samartzis D, Gillis CC, Shih P, O’Toole JE, Fessler RG. Intramedullary spinal cord tumors: Part I-epidemiology, pathophysiology, and diagnosis. Global Spine J. 2015. 5: 425-35
9. Tihan T, Fisher PG, Kepner JL, Godfraind C, McComb RD, Goldthwaite PT. Pediatric astrocytomas with monomorphous pilomyxoid features and a less favorable outcome. J Neuropathol Exp Neurol. 1999. 58: 1061-8
10. Tobin MK, Geraghty JR, Engelhard HH, Linninger AA, Mehta AI. Intramedullary spinal cord tumors: A review of current and future treatment strategies. Neurosurg Focus. 2015. 39: E14-
11. Wu L, Yang T, Yang C, Xu Y. Primary pilomyxoid astrocytoma of the thoracolumbar spinal cord in an adult. Neurol India. 2013. 61: 677-9