Thrombosed orbital varix of the inferior ophthalmic vein: A rare cause of acute unilateral proptosis
- Department of Neurological Surgery, University of Miami Health System, Miami, United States
- Department of Radiology, University of Miami Health System, Miami, United States
- Department of Ophthalmology, University of Miami, Bascom Palmer Eye Institute, Miami, United States.
Correspondence Address:
Ahmed Abdelsalam, Department of Neurological Surgery, University of Miami Health System, Miami, United States.
DOI:10.25259/SNI_236_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahmed Abdelsalam1, Ian A. Ramsay1, Uche Ehiemua1, John W. Thompson1, Hayes B. Fountain1, Tiffany Eatz1, Eva M. Wu1, Rita G. Bhatia2, Byron L. Lam3, David T. Tse3, Robert M. Starke1. Thrombosed orbital varix of the inferior ophthalmic vein: A rare cause of acute unilateral proptosis. 02-Jun-2023;14:186
How to cite this URL: Ahmed Abdelsalam1, Ian A. Ramsay1, Uche Ehiemua1, John W. Thompson1, Hayes B. Fountain1, Tiffany Eatz1, Eva M. Wu1, Rita G. Bhatia2, Byron L. Lam3, David T. Tse3, Robert M. Starke1. Thrombosed orbital varix of the inferior ophthalmic vein: A rare cause of acute unilateral proptosis. 02-Jun-2023;14:186. Available from: https://surgicalneurologyint.com/surgicalint-articles/12350/
Abstract
Background: Orbital varices are rare, accounting for only 0–1.3% of orbital masses. They can be found incidentally or cause mild to serious sequelae, including hemorrhage and optic nerve compression.
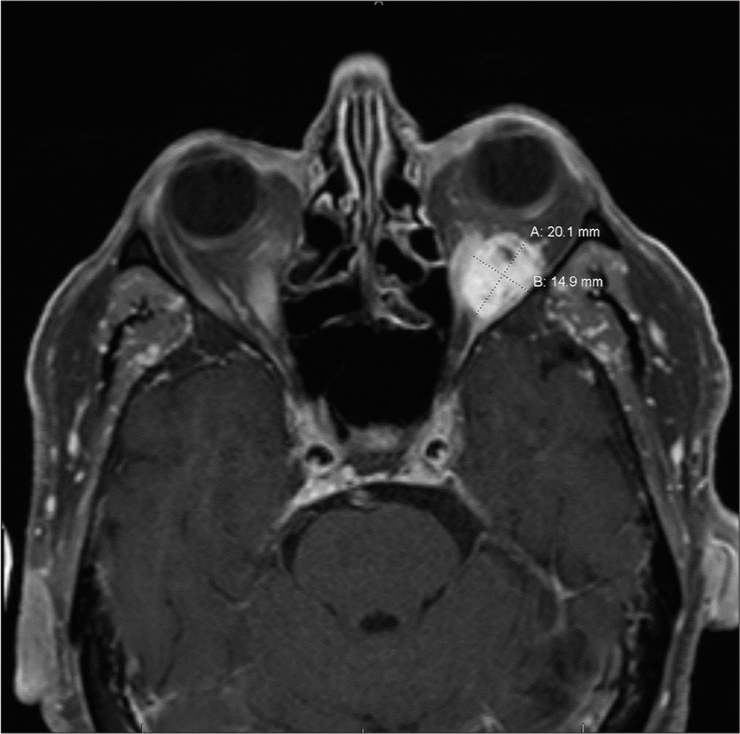
Case Description: We report a case of a 74-year-old male with progressively painful unilateral proptosis. Imaging revealed the presence of an orbital mass compatible with a thrombosed orbital varix of the inferior ophthalmic vein in the left inferior intraconal space. The patient was medically managed. On a follow-up outpatient clinic visit, he demonstrated remarkable clinical recovery and denied experiencing any symptoms. Follow-up computed tomography scan showed a stable mass with decreased proptosis in the left orbit consistent with the previously diagnosed orbital varix. One-year follow-up orbital magnetic resonance imaging without contrast showed slight increase in the intraconal mass.
Conclusion: An orbital varix may present with mild to severe symptoms and management, depending on case severity, ranges from medical treatment to escalated surgical innervation. Our case is one of few progressive unilateral proptosis caused by a thrombosed varix of the inferior ophthalmic vein described in the literature. We encourage further investigation into the causes and epidemiology of orbital varices.
Keywords: Ophthalmic vein, Orbit, Proptosis, Thrombosis, Varix, Orbital, Thrombosed
INTRODUCTION
An orbital varix is a rare pathology that has abnormally distensible, thin-walled veins. It can be primary due to congenital venous malformation or secondary due to orbital venous outflow obstruction.[
Orbital varices may be found in the intraconal space, a conical area posterior to the eyeball which includes arteries, nerves, and central orbital fat. The anterior boundary includes Tenon’s capsule of the posterior half of the eye; the posterior border is the orbital apex tendinous ring, and the peripheral boundary includes the four recti muscles with intermuscular septa and extraconal space. The intraconal space itself can be further separated into the central, medial, and lateral orbital spaces based on location in relation to the optic nerve. Due to the extremely innervated and vascular compact area of the intraconal space, it may be described as a rather limited and challenging surgical area.
We present a rare case of unilateral progressive proptosis caused by a secondary orbital varix due to thrombosis of the inferior ophthalmic vein.
CASE PRESENTATION
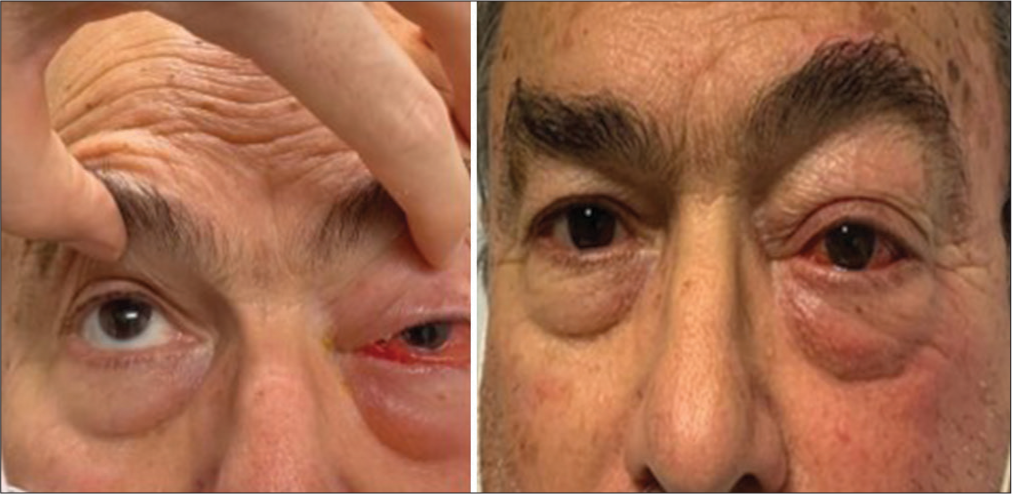
A 74-year-old male was admitted to the emergency department with a 3-day history of progressive painful proptosis of the left eye. His medical history included hypertension and hyperlipidemia with no history of trauma. Clinical examination revealed a left proptotic orbit with chemosis and scleral injection [
Imaging
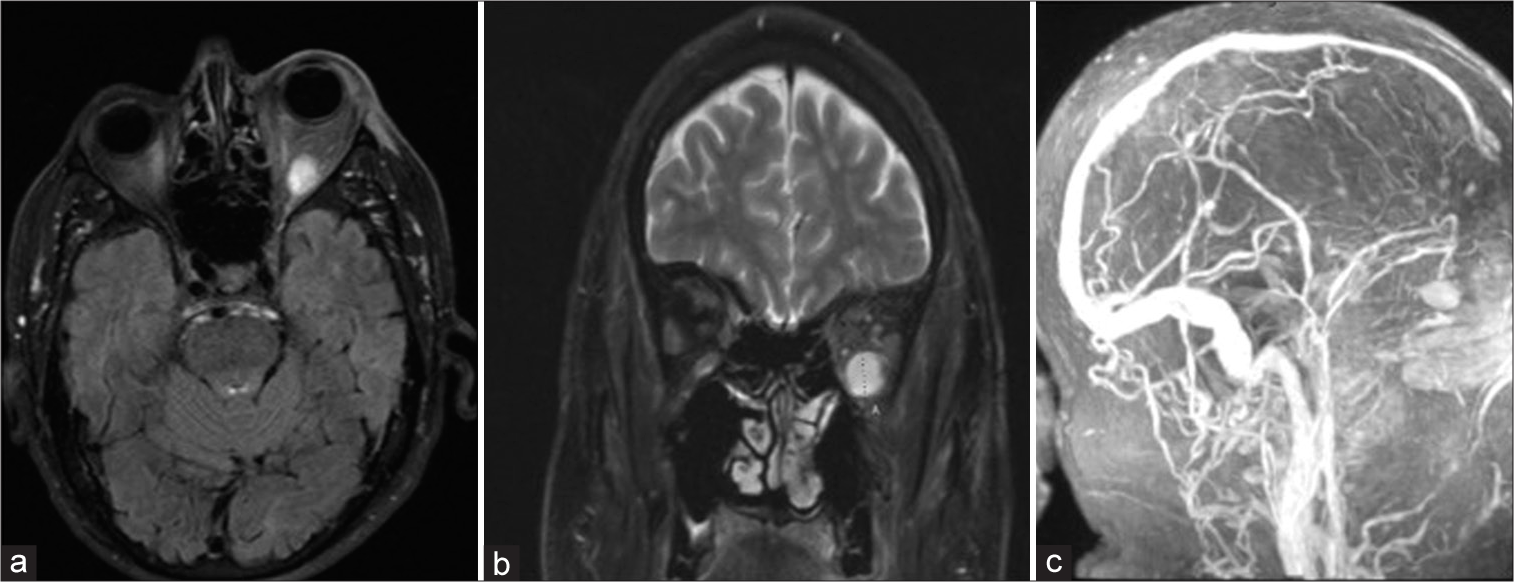
Computed tomography (CT) scan showed an ovoid mass in the lateral intraconal space with surrounding infiltration and increased vascularity. CT angiogram revealed a well-circumscribed heterogeneously enhancing mass within the inferior intraconal space of the left orbit (measuring 1.8 × 1.7 cm round) with periorbital soft-tissue swelling, suggesting inflammation [
Differential diagnosis
At this point, potential considerations included orbital cavernous malformation, metastatic tumor causing venous outflow stenosis, arteriovenous malformation, dural arteriovenous fistula, and thrombosed venous varix due to orbital cellulitis.
Management
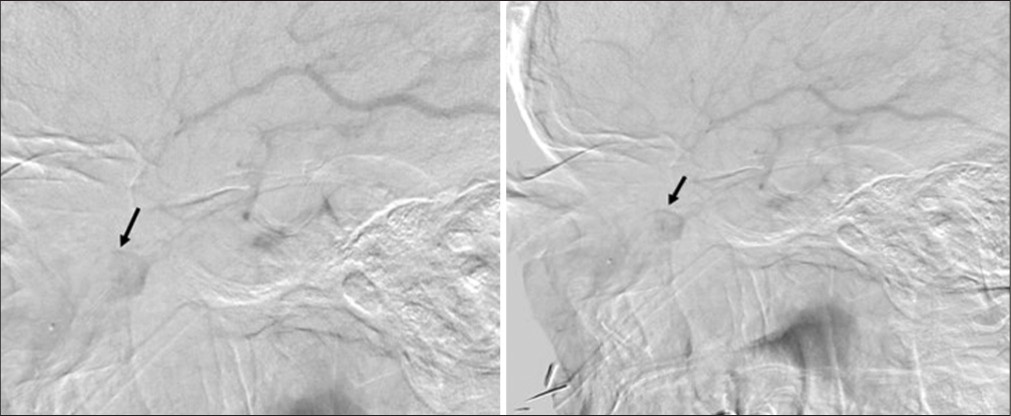
A neurosurgical consult was requested by the ophthalmology team. To further delineate the nature of the lesion, a diagnostic cerebral angiogram was performed, which revealed an intraconal venous varix [
Patient status and follow-up
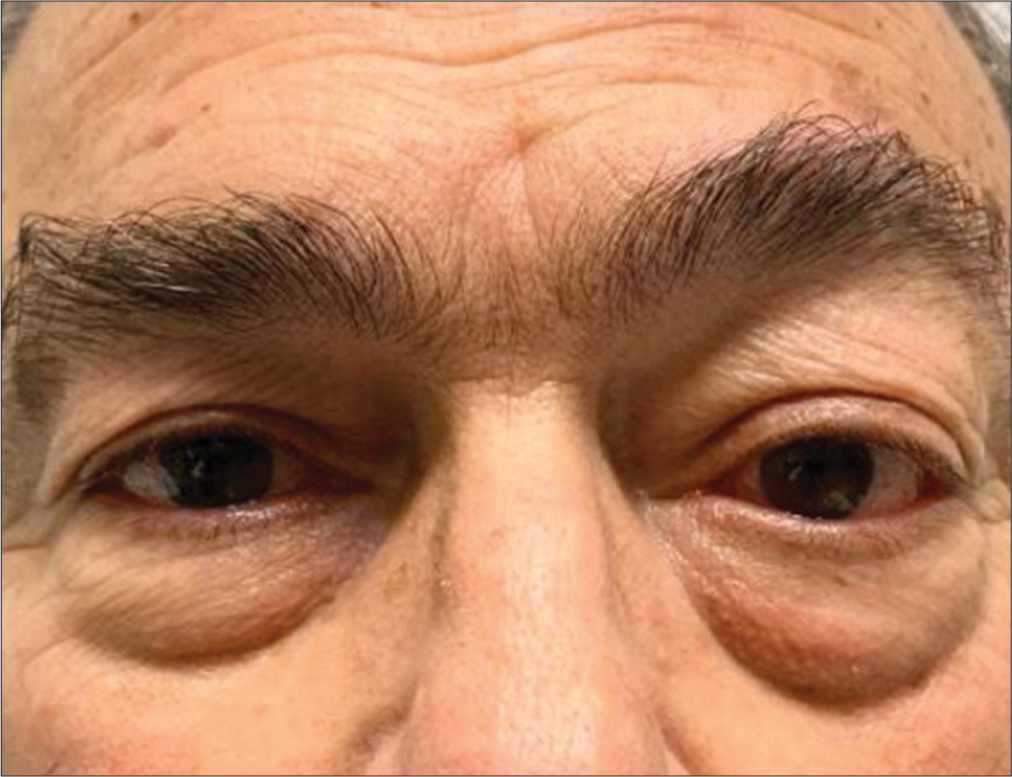
The patient was seen in the clinic 2 weeks after discharge. His symptoms had significantly improved, and he denied any eye redness, diplopia, or pain. On examination, there was no chemosis or scleral injection, but there was a significantly improved mild, painless proptosis [
DISCUSSION
Orbital varices are rare vascular malformations that account for only 0–1.3% of all histologically identified orbital masses.[
Orbital varix can be diagnosed clinically through observation of worsening proptosis proceeding the Valsalva maneuver. However, confirmation with imaging is required, especially if hemorrhage or thrombosis are suspected, and is instrumental in excluding differential diagnoses (i.e., – soft-tissue neoplasm or arteriovenous fistula). CT scan with contrast is the preferred imaging modality, on which a varix appears as a smooth or heterogeneous enhancing soft-tissue mass.[
Given the potential significant complications of an orbital varix, such as hemorrhage, blindness, and challenging surgical exposure associated with surgical excision, conservative management with observation is typically recommended.[
CONCLUSION
An orbital varix may present with mild to severe symptoms with potentially fatal sequalae if not promptly and adequately treated. Management, depending on case severity, ranges from medical treatment to escalated surgical innervation. Our case is one of few progressive unilateral proptosis caused by a thrombosed varix of the inferior ophthalmic vein described in the literature. We encourage further investigation into the causes and epidemiology of orbital varices.
Authors’ contributions
Concept and Design: Ahmed Abdelsalam, Robert M. Starke, Rita G. Bhatia, John W. Thompson. Data acquisition: Ahmed Abdelsalam, David T. Tse, Byron L. Lam, John W. Thompson. Data analysis and interpretation: Tiffany Eatz, Uche Ehiemua, Eva M. Wu , Ian A. Ramsay. Literature Search: Tiffany Eatz, Uche Ehiemua, Eva M. Wu, Ian A. Ramsay. Drafting the first manuscript: Ahmed Abdelsalam. Revision of the manuscript for important intellectual content: Robert M. Starke, Tiffany Eatz, John W. Thompson, David T. Tse, Byron L. Lam, Rita G. Bhatia, Approval of final manuscript version for submission: All authors.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
Acknowledgments
Disclosures: The authors report no conflict of interest. RMS research is supported by the NREF, Joe Niekro Foundation, Brain Aneurysm Foundation, Bee Foundation, and by National Institute of Health (R01NS111119-01A1) and (UL1TR002736, KL2TR002737) through the Miami Clinical and Translational Science Institute, from the National Center for Advancing Translational Sciences and the National Institute on Minority Health and Health Disparities. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH. RMS has an unrestricted research grant from Medtronic and has consulting and teaching agreements with Penumbra, Abbott, Medtronic, Balt, InNeuroCo, Cerenovus, Naglreiter and Optimize Vascular.
References
1. Arun J, Peter AD. Simultaneous bilateral thrombosed orbital varices: A case report. Ophthalmic Plast Reconstr Surg. 2019. 35: e129-30
2. Issiaka M, Jamaleddine H, El Belhadji M, Iro S, Slimani F. Orbital varix: A rare case of unilateral exophthalmos, case report. Ann Med Surg (Lond). 2021. 66: 102346
3. Karcioglu ZA, editors. Orbital Tumors: Diagnosis and Treatment. Berlin: Springer; 2015. p.
4. Lloyd GA, Wright JE, Morgan G. Venous malformations in the orbit. Br J Ophthalmol. 1971. 55: 505-16
5. Rubin PA, Remulla HD. Orbital venous anomalies demonstrated by spiral computed tomography. Ophthalmology. 1997. 104: 1463-70
6. Vadlamudi V, Gemmete JJ, Chaudhary N, Pandey AS, Kahana A. Transvenous sclerotherapy of a large symptomatic orbital venous varix using a microcatheter balloon and bleomycin. BMJ Case Rep. 2015. 2015: bcr2015011777
7. Wade RG, Maddock TB, Ananth S. Orbital varix thrombosis: A rare cause of unilateral proptosis. BMJ Case Rep. 2013. 2013: bcr2012007935