- Department of Neurosurgery, Drexel University College of Medicine, Philadelphia, Pennsylvania, United States.
- Department of Neurosurgery, Global Neurosciences Institute, Philadelphia, Pennsylvania, United States.
- Department of Neurosurgery, St. Christopher’s Hospital for Children, Philadelphia, Pennsylvania, United States.
DOI:10.25259/SNI_207_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hunter J. King1, Rohin Ramchandani1, Christina Maxwell1,2, Atom Sarkar1,2,3, Tina Loven1,2,3. To cut or not to cut? A case report on pediatric intervertebral disc calcification. 28-Jun-2021;12:307
How to cite this URL: Hunter J. King1, Rohin Ramchandani1, Christina Maxwell1,2, Atom Sarkar1,2,3, Tina Loven1,2,3. To cut or not to cut? A case report on pediatric intervertebral disc calcification. 28-Jun-2021;12:307. Available from: https://surgicalneurologyint.com/surgicalint-articles/10929/
Abstract
Background: Intervertebral disc calcification (IVDC) is a rare cause of acute spinal pain in pediatric patients. The most common symptom is back or neck pain, but muscle spasm, muscle weakness, and sensory loss also occur. Many patients have an alarming presentation and radiological findings concerning for spinal cord compression.
Case Description: A 10-year-old female presented with 2 weeks of worsening back pain and restricted neck flexion with no history of preceding trauma. Magnetic resonance imaging (MRI) showed T4/5 and T5/6 vertebral disc calcification and posterior herniation causing thoracic spinal cord compression. Despite concerning imaging findings, we decided to manage this patient conservatively with nonsteroidal anti-inflammatory drugs, leading to the improvement of symptoms within 9 days, and resolution of all pain within 1 month after hospital discharge. At 6 months follow-up, MRI showed complete resolution of calcification within the spinal canal.
Conclusion: This case report emphasizes IVDC as an important differential diagnosis of pediatric disc disease that does not require surgical intervention. X-ray imaging with PA and lateral views is an adequate screening for these patients. Majority of cases resolve within 6 months with conservative therapy.
Keywords: Disc calcification, Intervertebral, Nontraumatic, Pediatric, Spinal pain
INTRODUCTION
Intervertebral disc calcification (IVDC) in pediatric patients is a rare occurrence with approximately 300 documented cases in the medical literature.[
Diagnosis of IVDC relies on successful radiologic studies, with X-ray as an adequate initial screening.[
We present a case involving a 10-year-old female patient that exhibits IVDC and posterior disc herniation into the spinal canal with no prior trauma or other underlying etiology.
CASE DESCRIPTION
A 10-year-old unvaccinated healthy female with a history of sickle cell trait and enuresis presented to the emergency department complaining of progressive midline back pain for 2 weeks and restricted neck flexion for several days. Pain was exacerbated by movement and no preceding trauma was reported. Conservative treatment consisting of heat and cold packs, massage, acetaminophen, and ibuprofen was unable to adequately provide relief. The patient also demonstrated lower extremity paresthesia and inability to ambulate on examination, but full motor strength.
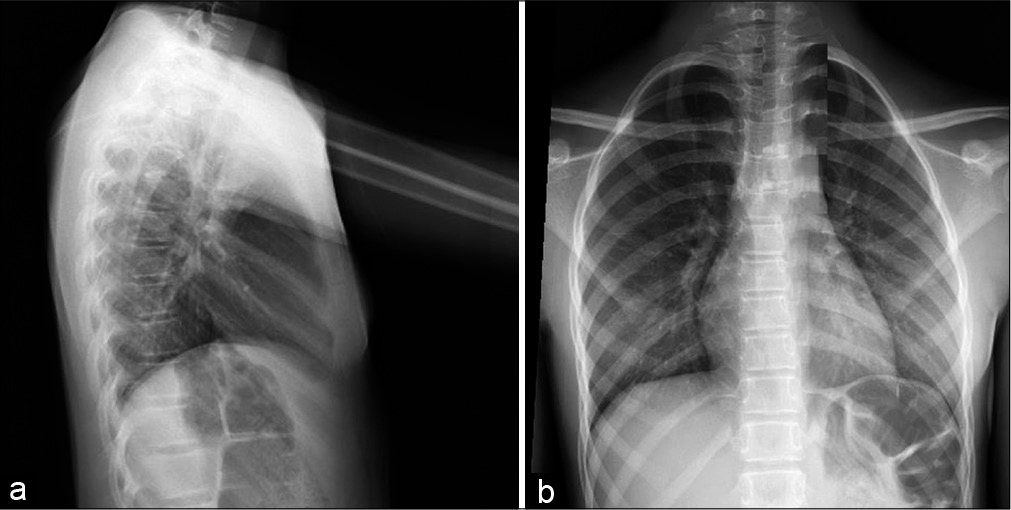
Emergency department course was remarkable for tachycardia and tachypnea. Initial physical examination demonstrated restricted neck flexion without tenderness or swelling. Her back was tender to palpation over the left lower paraspinal muscles with slight decreased range of motion. Initial laboratories were significant for a mildly elevated ESR of 17 mm/h and CRP of 5.23 mg/L. Initial X-rays showed disc calcification without any fractures [
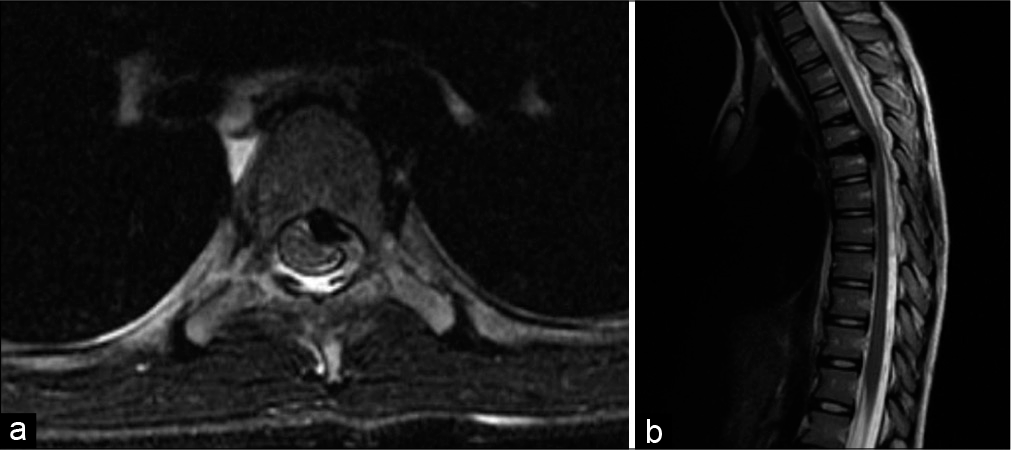
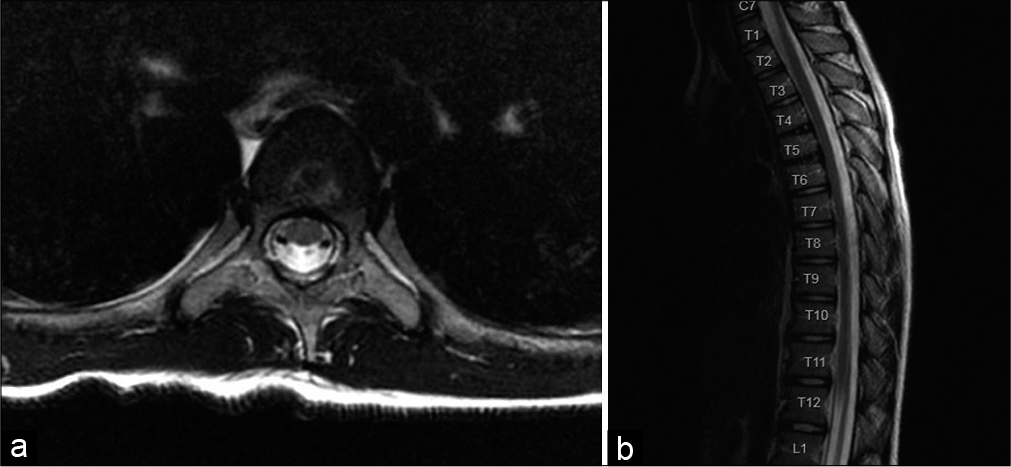
Hospital course continued with ketorolac and acetaminophen overnight which reduced her pain. Repeat physical examination was notable for positive Brudzinski and Kernig sign, abnormal gait, and nuchal rigidity with total neck extension worrisome for possible meningitis. Neurological examination was otherwise normal and nonfocal. Empiric treatment with ceftriaxone and vancomycin was started. Lumbar puncture was deferred for magnetic resonance imaging (MRI) due to concerns of a possible epidural abscess or space-occupying lesion. MRI of brain, cervical, and thoracic spine was performed under general anesthesia, showing disc calcification with herniation causing spinal cord compression of T4-T6. The discs were involved at T4/5 and T5/6, with a flattened T5 vertebrae posteriorly, and hypointense signal indicative of calcification [
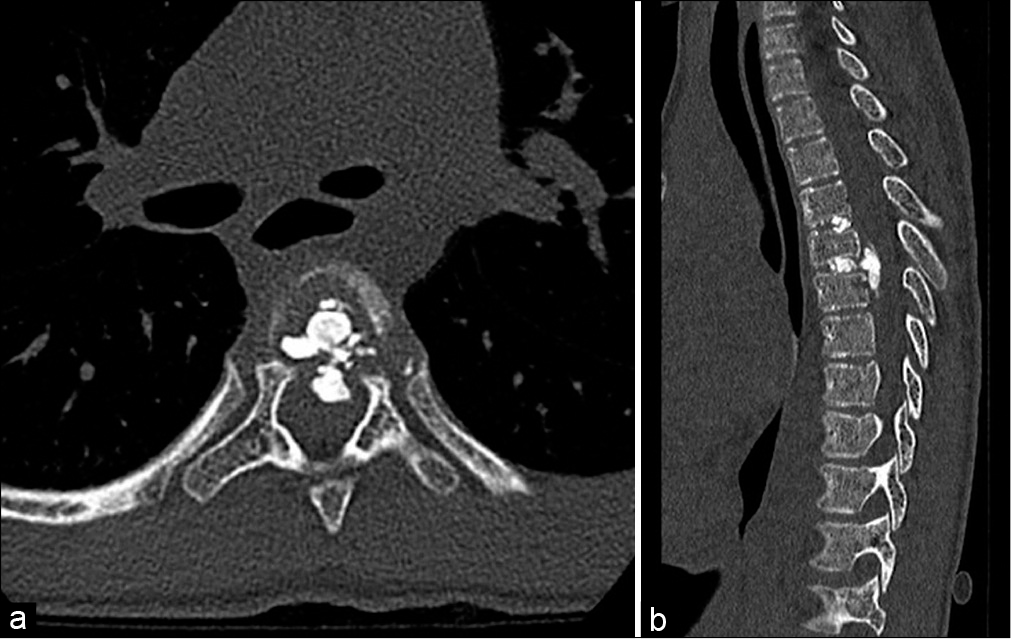
Neurosurgery was consulted and recommended computed tomography (CT) of the thoracic spine [
Diagnosis was made as pediatric IVDC based on a combination of imaging findings and patient history. Antibiotics were discontinued and medical management with ibuprofen and diazepam taper was recommended instead of surgery. Endocrinology workup for metabolic bone disease was unremarkable. The patient was discharged and advised for neurosurgical follow-up in 1 month.
The patient reported to the clinic 9 days after hospital discharge with marked improvement of symptoms. She reported moderate back pain, but denied any difficulty ambulating, bowel or bladder incontinence, or paresthesia.
No neurological deficits were observed on physical examination. Diazepam taper, acetaminophen, and ibuprofen were given to additionally alleviate her pain.
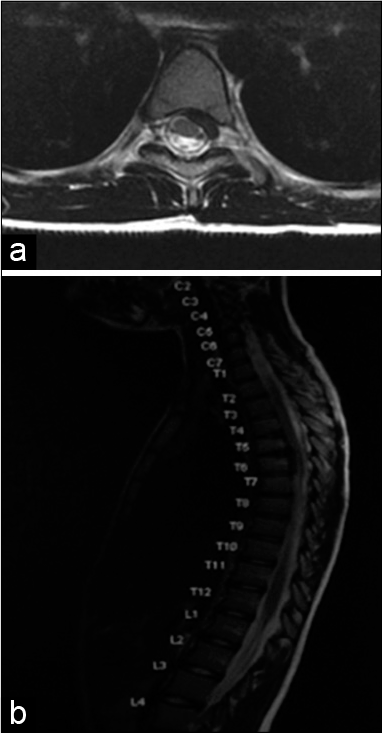
One month repeat, MRI showed significant improvement of disc herniation and stenosis [
Six months repeat, MRI imaging showed complete resolution of epidural calcification and stenosis. The T4/5 and T5/6 discs still displayed some calcification, but herniation had completely resolved [
DISCUSSION
IVDC in pediatrics is a rare condition with only around 300 reported cases in the literature.[
IVDC has higher prevalence in males compared to females (3:2 ratio), with estimated peak incidence of 6–10 years of age.[
The exact etiology of IVDC is unknown, but is suggested to be multifactorial involving genetics, trauma, metabolic abnormalities, infectious, or inflammatory causes.[
It is important to note that pediatric IVDC has a different pathophysiology from adult patients. Adults experience disc calcification secondary to trauma, hyperparathyroidism, hemochromatosis, hypervitaminosis D, ochronosis, homocystinuria, and alkaptonuria.[
Radiology plays a key role in diagnosing cases of IVDC in pediatrics.[
IVDC in pediatrics is suggested to be self-limiting and therefore responds best to medical treatment with analgesics and anti-inflammatory medications. Muscle relaxants, cervical collars, and bed rest are also helpful.[
In a literature review of 50 pediatrics cases with IVDC, only eight received surgical decompression due to cord and nerve root impingement. Only one patient of the 50 had residual symptoms at 6 months follow-up.[
CONCLUSION
IVDC is a benign self-limiting condition that should be suspected in pediatrics who present with back or neck pain, and imaging suspicious of cervical or thoracic disc calcification. There is generally no preceding trauma or infectious etiology. Proper diagnosis can avoid extensive testing and surgeries. X-ray imaging with PA and lateral views is an adequate screening for these patients, and is recommended to avoid extensive workup and unnecessary therapies. The majority of cases resolve within 6 months with conservative therapies and these patients should not be operated on.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Barrett MO, Anderson JT, Rao B, Vaslow D, Hoernschemeyer DG. Multilevel pediatric cervicothoracic intervertebral disc calcifications. Am J Orthop (Belle Mead NJ). 2008. 37: E126-8
2. Dushnicky MJ, Okura H, Shroff M, Laxer RM, Kulkarni AV. Pediatric idiopathic intervertebral disc calcification: Single-center series and review of the literature. J Pediatr. 2019. 206: 212-6
3. Garg M, Kumar S, Satija B, Gupta R. Pediatric intervertebral disc calcification: A no touch lesion. J Craniovertebr Junction Spine. 2012. 3: 23-5
4. Gerlach R, Zimmermann M, Kellermann S, Lietz R, Raabe A, Seifert V. Intervertebral disc calcification in childhood-a case report and review of the literature. Acta Neurochir (Wien). 2001. 143: 89-93
5. Lam SK, Niedzwecki CM, Daniels B, Mayer RR, Vakharia MM, Jea A. Acute spinal cord injury associated with multilevel pediatric idiopathic intervertebral disc calcification: Case report. J Neurosurg Pediatr. 2016. 17: 182-6
6. Mizukawa K, Kobayashi T, Yamada N, Hirota T. Intervertebral disc calcification with ossification of the posterior longitudinal ligament. Pediatr Int. 2017. 59: 622-4
7. O’Dell MC, Flores M, Murray JV. Pediatric idiopathic intervertebral disc calcification. Pediatr Neurol. 2016. 61: 115-6
8. Tsutsumi S, Yasumoto Y, Ito M. Idiopathic intervertebral disk calcification in childhood: A case report and review of literature. Childs Nerv Syst. 2011. 27: 1045-51