- Departement of Neurosurgery, AL-Ramadi Teaching Hospital, Al-Anbar, Iraq,
- Departement of Neurosurgery, College of Dentistry, Al-Anbar University, Al-Anbar, Iraq,
- Departement of Neurosurgery, College of Medicine, University of Baghdad, Iraq,
- Departement of Neurosurgery, College of Medicine, University of Mustansiriyah, Baghdad, Iraq,
- Department of Neurosurgery, University of Cincinnati, Cincinnati, Ohio, United States.
Correspondence Address:
Mustafa Ismail, Department of Neurosurgery, College of Medicine, University of Baghdad, Baghdad, Iraq.
DOI:10.25259/SNI_695_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hisham Maddah Al-Alousi1, Kamal T. Al-Kubaisi2, Mustafa Ismail3, Teeba A. Al-Ageely3, Aanab O. Abdulameer3, Sajjad A. Aluaibi4, Rania H. Al-Taie4, Samer S. Hoz5. Transbasal penetrating traumatic brain injury caused by a rifle rod: A case report. 25-Nov-2022;13:555
How to cite this URL: Hisham Maddah Al-Alousi1, Kamal T. Al-Kubaisi2, Mustafa Ismail3, Teeba A. Al-Ageely3, Aanab O. Abdulameer3, Sajjad A. Aluaibi4, Rania H. Al-Taie4, Samer S. Hoz5. Transbasal penetrating traumatic brain injury caused by a rifle rod: A case report. 25-Nov-2022;13:555. Available from: https://surgicalneurologyint.com/surgicalint-articles/12020/
Abstract
Background: Penetrating traumatic brain injury (TBI) caused by a low-velocity object is a rare entity with a potential range of critical complications.
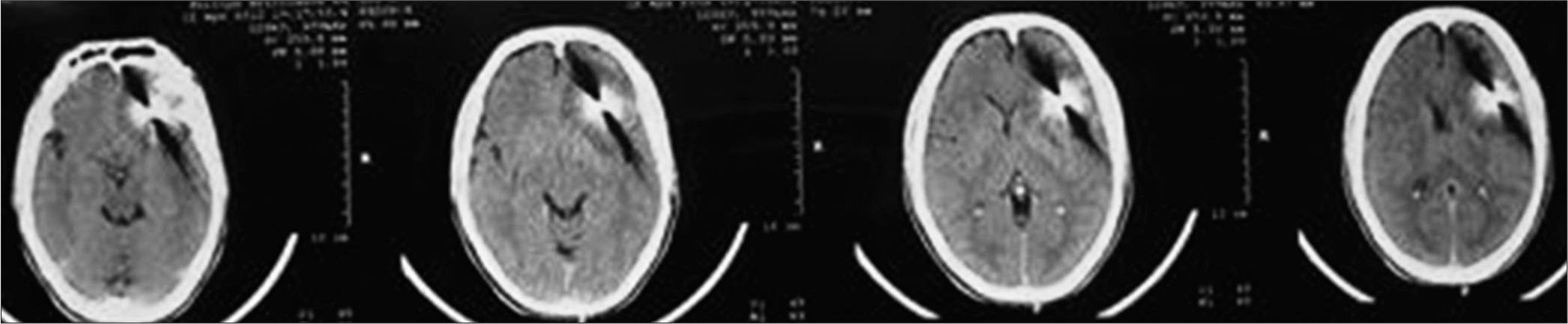
Case Description: We report a unique case of a 30-year-old male presenting with penetrating TBI caused by a rifle’s cleaning rod. The rod passes through the left nostril to reach the frontal lobe after transgressing the sella turcica. A cranial computed tomography scan shows the extension of brain damage and the trajectory of the rod with no evidence of an associated vascular injury. Surgical removal of the rifle rod was performed using a transnasal approach by a multidisciplinary with the postoperative course went uneventfully.
Conclusion: Transbasal penetrating TBI through the nose is an extremely rare entity. This type of head injury carries its own peculiarities that deviate from the classic treatment algorithms.
Keywords: Skull base, Penetrating head injury, Rifle rod, Traumatic brain injury
INTRODUCTION
Penetrating traumatic brain injury (TBI) through the nose is a rare entity with various potential culprits.[
CASE DESCRIPTION
A 30-year-old male was admitted to the surgical department of Al-Anbar Hospital in Iraq due to a complaint of behavioral changes a few days after firing his rifle. The patient had no history of bleeding, loss of consciousness (Glasgow Coma Scale [GCS] of 15), weakness, or headache. Moreover, there was no clear entry wound. On physical examination, he was vitally stable and conscious but disoriented. Neurological examination was unremarkable in that there was no loss of sensory, motor, or cerebellar function; besides, he had normal reflexes.
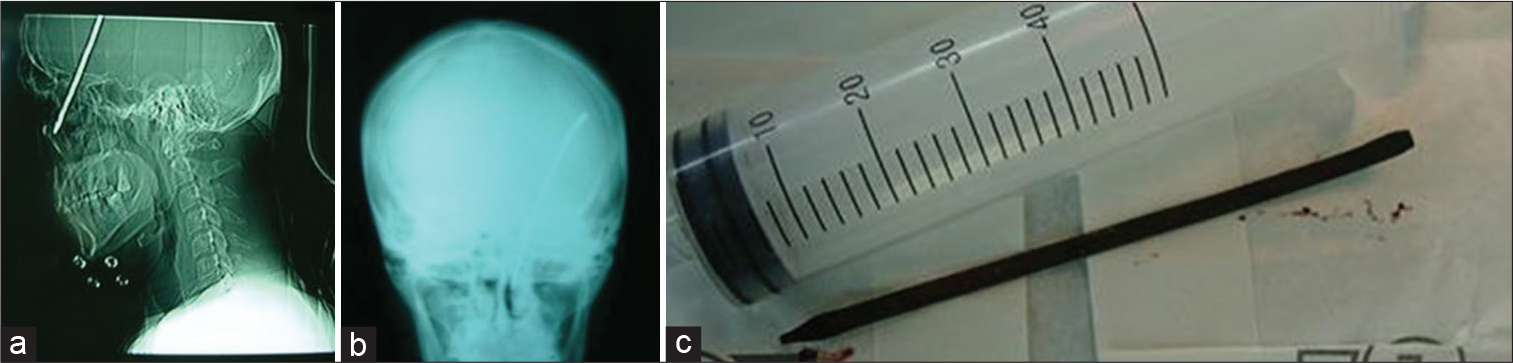
Imaging assessment was initially performed using a plain X-ray, which demonstrated the presence of an intracranial foreign body [
The patient was admitted to the neurosurgery ward. The extraction was done through the same site through a transnasal approach with the assistance of a maxillofacial surgeon and otolaryngologists. The closure was performed through layers using a septal flap and fat. Postoperative imaging showed no ICH with a GCS of 15. Further management included prophylactic antibiotics and antiepileptic medications throughout the follow-up period, which was uneventful.
DISCUSSION
Although transnasal TBI represents one of the most severe traumatic brain injuries,[
In this patient, the rifle cleaning rod accidentally sprang out and penetrated his left nostril during his gun maintenance. Additional examples of unintentional firearm accidents could result from poor weapon handling, inadequate weapon safety measures, and incidental child handling of a firearm.[
However, in first aid response, foreign bodies should be left in situ until proper diagnostic tools are available. The foreign bodies might prevent significant bleeding by acting as a tamponade.[
The uneventful history of the patient and the absence of wound entry made the diagnosis more difficult. However, the behavioral changes and social history of firearm acquisition led to a more focused differential diagnosis. Radiological imaging was ordered for the confirmation of diagnosis. Notably, a CT scan can localize different intracranial lesions, estimate the depth of injury, and reveal ossific fractures and the extent of parenchymal damage; therefore, it is considered the gold standard diagnostic tool for evaluating penetrating TBIs.[
The management of the patient started in the emergency room with advanced trauma care according to ATLS guidelines. The patient was then taken to the operating room and started broad-spectrum antibiotic coverage with the third generation of cephalosporins and metronidazole. Craniotomy has the advantages of early visualization with the protection of neurovascular structures, controlled object removal, accessible debridement of the devitalized brain tissue, associated hematoma emptying, and adequate dural reparation. The optimum approach would be a combined transnasal and transcranial approach according to the vascular injury extension. Thus, if there was an injury to the anterior cerebral artery, the combined approach would be transnasal and transfrontal.
In contrast, if the middle cerebral artery is injured, the pterional approach combined with the transnasal approach would be effective. To avoid infection complications and further tissue damage, urgent surgery was performed with the transnasal approach without a vascular study. To overcome this obstacle, surgical step modification was planned after collaborating with the attending neurosurgeon, maxillofacial surgeon, and otolaryngologist. These modifications include drilling 0.5 cm bone on the periphery of the metallic nail, followed by the intact frontobasal dura opening at the rod’s periphery for proper visualization of the surgical field. A careful extraction was performed with the aid of a pressure monitor for rapid detection of any vascular impairment of the internal carotid artery and circle of Willis. The nail was successfully extracted with no intraoperative bleeding. Hemostasis and field washing were done. After that, the frontobasal dura was repaired layer by layer, followed by an autogenous bone graft.
The postoperative course was uneventful; after 2 days of close observation, his GCS was 15. However, the patient was scheduled for a follow-up every 6 months for a thorough neurological assessment.
Severe complications of intracranial foreign bodies include abscess formation, cerebrospinal fluid fistulas, posttraumatic seizure foci, ICH, vascular injuries, and infection.[
In summary, managing cases of penetrating TBI caused by unusual low-velocity penetrating tools do not follow a typical plan. Therefore, treatment should be individualized according to the severity of the injury and the specific type of insult.
CONCLUSION
Penetrating brain injury caused by unusual tools has characteristics that are different from high-velocity penetrating TBI. In this study, removing the rifle cleaning rod was challenging and required a multidisciplinary team, including neurosurgeons, otolaryngologists, and maxillofacial surgeons, to plan the treatment and accomplish a good outcome.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Aarabi B, Alden TD, Chestnut RM, Downs JH, Ecklund JM, Eisenberg HM. Antibiotic prophylaxis. J Trauma. 2001. 51: S34-40
2. Aarabi B, Tofighi B, Kufera JA, Hadley J, Ahn ES, Cooper C. Predictors of outcome in civilian gunshot wounds to the head. J Neurosurg. 2014. 120: 1138-46
3. Aarabi B. Causes of infections in penetrating head wounds in the Iran-Iraq War. Neurosurgery. 1989. 25: 923-6
4. Blennow K, Brody DL, Kochanek PM, Levin H, McKee A, Ribbers GM. Traumatic brain injuries. Nat Rev Dis Primers. 2016. 2: 16084
5. Bursick DM, Selker RG. Intracranial pencil injuries. Surg Neurol. 1981. 16: 427-31
6. Gennarelli TA, Champion HR, Sacco WJ, Copes WS, Alves WM. Mortality of patients with head injury and extracranial injury treated in trauma centers. J Trauma. 1989. 29: 1193-201
7. Gökçek C, Erdem Y, Köktekir E, Karatay M, Bayar MA, Edebali N. Intracranial foreign body. Turk Neurosurg. 2007. 17: 121-4
8. Joseph B, Aziz H, Pandit V, Kulvatunyou N, O’Keeffe T, Wynne J. Improving survival rates after civilian gunshot wounds to the brain. J Am Coll Surg. 2014. 218: 58-65
9. Kaufman HH. Care and variations in the care of patients with gunshot wounds to the brain. Neurosurg Clin N Am. 1995. 6: 727-39
10. Offiah C, Twigg S. Imaging assessment of penetrating craniocerebral and spinal trauma. Clin Radiol. 2009. 64: 1146-57
11. Rinaldi A, Gazzeri R, Conti L, Schiavone M. Cranio-orbital missile wound and bullet migration: Case report. J Neurosurg Sci. 2000. 44: 107-12
12. Rosenfeld JV, Bell RS, Armonda R. Current concepts in penetrating and blast injury to the central nervous system. World J Surg. 2015. 39: 1352-62
13. Shuker ST. The immediate lifesaving management of maxillofacial, life-threatening haemorrhages due to IED and/ or shrapnel injuries: When hazard is in hesitation, not in the action. J Craniomaxillofac Surg. 2012. 40: 534-40
14. Ursic C, Curtis K. Thoracic and neck trauma. Part four. Int Emerg Nurs. 2010. 18: 177-80
15. Van Wyck DW, Grant GA, Laskowitz DT. Penetrating traumatic brain injury: A review of current evaluation and management concepts. J Neurol Neurophysiol. 2015. 6: 336-43
16. Wani AA, Ramzan AU, Shoib Y, Malik NK, Nizami FA, Dhar A. Stray bullet: An accidental killer during riot control. Surg Neurol Int. 2011. 2: 122
17. Yamamoto I, Yamada S, Sato O. Unusual craniocerebral penetrating injury by a chopstick. Surg Neurol. 1985. 23: 396-8
18. Zyck S, Toshkezi G, Krishnamurthy S, Carter DA, Siddiqui A, Hazama A, Jayarao M. Treatment of penetrating nonmissile traumatic brain injury. Case series and review of the literature. World Neurosurg. 2016. 91: 297-307