- Department of Neurosurgery, Prasat Neurological Institute, Bangkok, Thailand.
- Department of Neuroradiology, Prasat Neurological Institute, Bangkok, Thailand.
- Department of Radiology, Bumrungrad International Hospital, Bangkok, Thailand.
Correspondence Address:
Prasert Iampreechakul, Department of Neurosurgery, Prasat Neurological Institute, Bangkok, Thailand.
DOI:10.25259/SNI_1162_2021
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Prasert Iampreechakul1, Korrapakc Wangtanaphat1, Sunisa Hangsapruek2, Yodkhwan Wattanasen2, Punjama Lertbutsayanukul2, Somkiet Siriwimonmas3. Transfemoral transvenous embolization through the vein of Trolard and superficial middle cerebral vein for cavernous sinus dural arteriovenous fistula with isolated cortical vein drainage: A case report and literature review. 29-Jan-2022;13:34
How to cite this URL: Prasert Iampreechakul1, Korrapakc Wangtanaphat1, Sunisa Hangsapruek2, Yodkhwan Wattanasen2, Punjama Lertbutsayanukul2, Somkiet Siriwimonmas3. Transfemoral transvenous embolization through the vein of Trolard and superficial middle cerebral vein for cavernous sinus dural arteriovenous fistula with isolated cortical vein drainage: A case report and literature review. 29-Jan-2022;13:34. Available from: https://surgicalneurologyint.com/surgicalint-articles/transfemoral-transvenous-embolization-through-the-vein-of-trolard-and-superficial-middle-cerebral-vein-for-cavernous-sinus-dural-arteriovenous-fistula-with-isolated-cortical-vein-drainage-a-case-repo/
Abstract
Background: Endovascular treatment may be challenging for cavernous sinus dural arteriovenous fistulas (CSDAVFs) with prominent leptomeningeal drainage without other accessible routes. We report a case of CSDAVF with isolated cortical venous successfully drainage treated by percutaneous transvenous embolization through the vein of Trolard and superficial middle cerebral vein (SMCV). We also review the literature of CSDAVFs treated by transvenous embolization through SMCV with or without combined surgical approach.
Case Description: A 46-year-old woman presented with ocular symptoms and delayed treatment was encountered due to the COVID-19 pandemic. Cerebral angiography showed a CSDAVF (Barrow type D, Borden II, and Cognard II a + b) with isolated cortical vein drainage. Percutaneous transvenous access to the fistula through the inferior petrosal sinus was attempted but failed. Transvenous embolization through the vein of Trolard and SMCV was further attempted, and satisfactory occlusion of the fistula was achieved with detachable coils. This access route was chosen because of the occlusion of other access routes and can obliterate the need for more invasive approach, that is, combined surgical and endovascular approach. Cerebral angiography obtained 6 months following the procedure, confirmed complete angiographic obliteration of the fistula. The patient made an uneventful recovery.
Conclusion: To avoid invasive combined surgical and endovascular approach, transvenous embolization through the vein of Trolard and SMCV may be another accessible option for treating CSDAVF with isolated cortical venous drainage.
Keywords: Cavernous sinus dural arteriovenous fistula, Indirect carotid-cavernous fistula, Superficial middle cerebral vein, The vein of Trolard, Transvenous embolization
INTRODUCTION
Cavernous sinus dural arteriovenous fistulas (CSDAVFs) are abnormal communications between dural arteries and the cavernous sinus (CS). Feeding vessels may arise from dural branches of the cavernous segment of the internal carotid artery, that is, the meningohypophyseal trunk and/or inferolateral trunk, and/or the external carotid artery, that is, the middle meningeal artery, accessory meningeal artery, artery of foramen rotundum, and/ or ascending pharyngeal artery. CSDAVFs commonly appear in middle-aged female and symptoms of the patients usually relate to venous drainage patterns of the CS.[
Due to the risk of embolic complications associated with transarterial embolization of CSDAVFs, transvenous approach through the inferior petrosal sinus (IPS) using coils and/or liquid embolic materials was preferred method.[
We present a challenging case of transvenous embolization through the vein of Trolard and SMCV for CSDAVF with isolated cortical venous drainage by a femoral venous approach. We also review the literature of patients treated by transvenous embolization for CSDAVFs through SMCV.
CASE DESCRIPTION
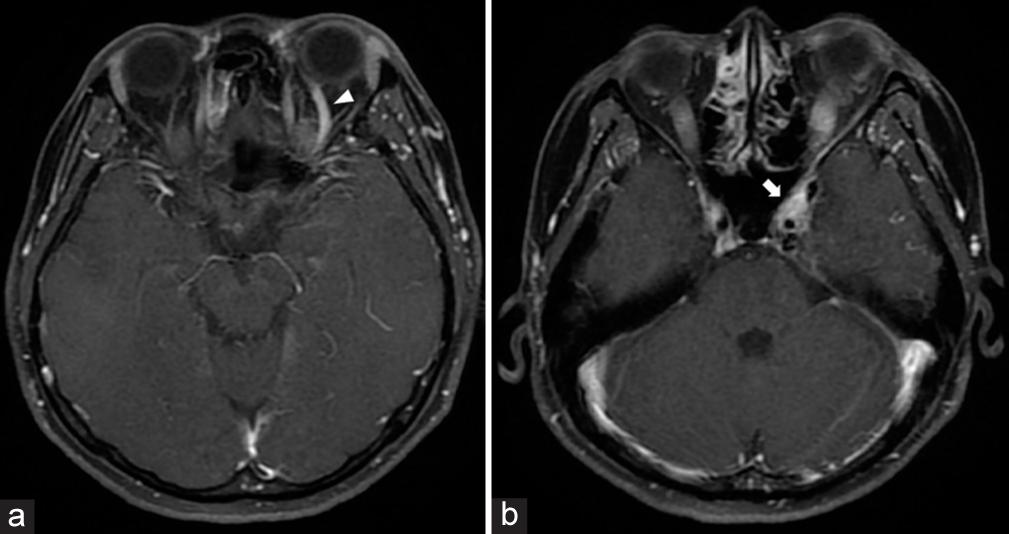
A 46-year-old woman experienced left red eye, proptosis, and diplopia for 2 weeks. She went to a local hospital and was found to have a left sixth cranial nerve paresis. Cranial magnetic resonance imaging revealed the dilatation of the left superior ophthalmic vein (SOV) and enlarged left CS [
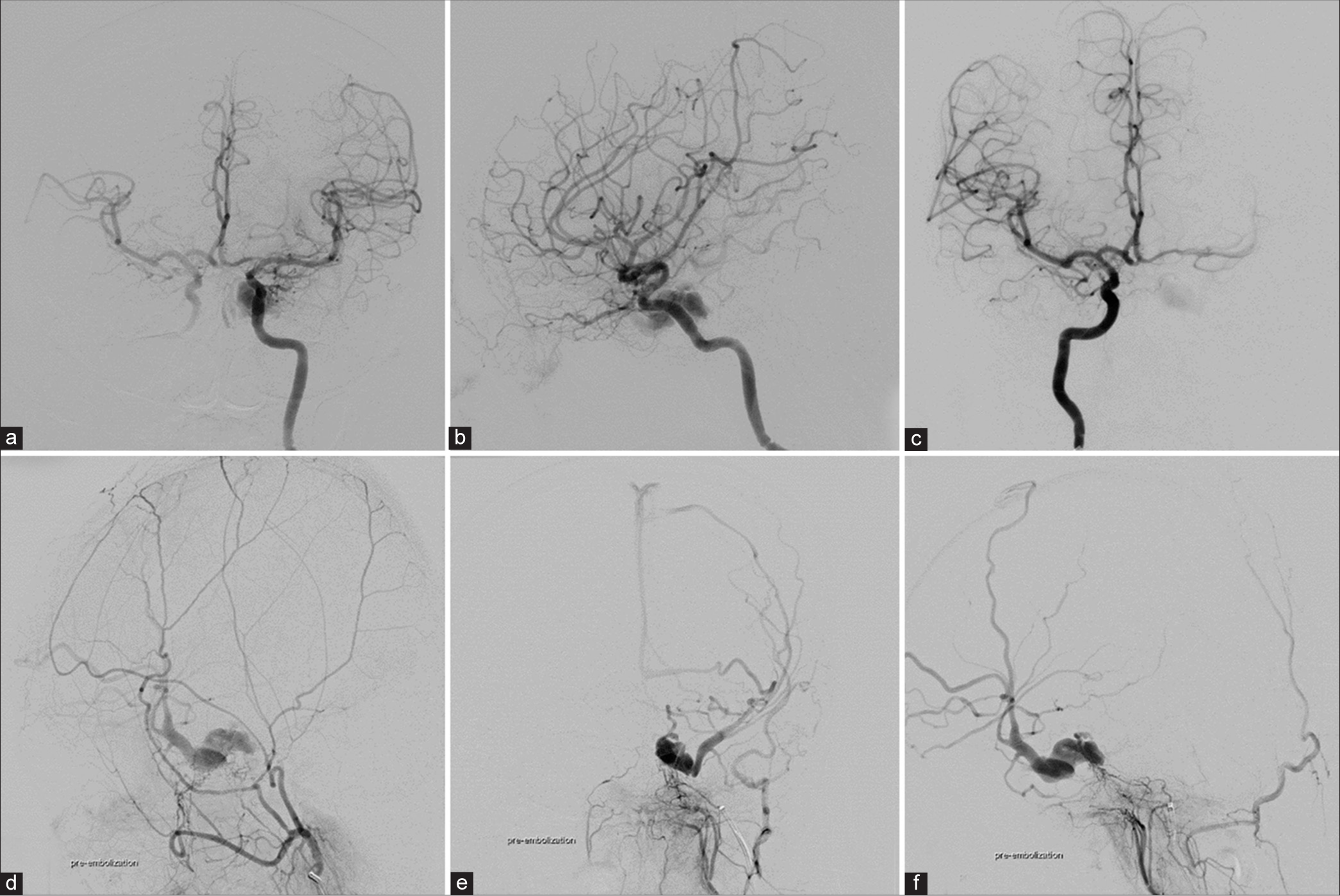
Figure 2:
(a) Anteroposterior (AP) and (b) lateral views of the left internal carotid artery (ICA) angiography show the left cavernous sinus dural arteriovenous fistula supplied from the left meningohypophyseal trunk (MHT). (c) AP view of the right ICA injection demonstrates the clival branch from the right MHT supplying the fistula. (d) Lateral view of the external carotid artery injection reveals the same fistula fed by the artery of the foramen rotundum and accessory meningeal artery. (e) AP and (f) lateral views of the left ascending pharyngeal artery injection illustrate the arterial feeders supplying the fistula with retrograde venous drainage into the left sphenoparietal sinus, superficial middle cerebral vein, the basal vein of Rosenthal, and multiple frontal and parietal cortical veins.
Under general anesthesia, transvenous embolization through the occluded left IPS was attempted but failed to reach the CS. We decided to try to access the left vein of Trolard. With heparinization, distal access guiding catheter (Fargo MAX, Balt Extrusion, Montmorency, France) was introduced into the left sigmoid sinus. Under fluoroscopic road map, Prowler Plus (Codman Neurovascular, Raynham, MA, USA) microcatheter, length 150 cm, was used over the Agility Steerable guidewire (0.016 soft, Codman Neurovascular, Raynham, MA, USA) but this microcatheter was too short to navigate into the CS. Therefore, the microcatheter was changed to Prowler Select Plus (Codman Neurovascular, Raynham, MA, USA), length 170 cm, over the same guidewire. This system was successfully navigated into the affected CS [
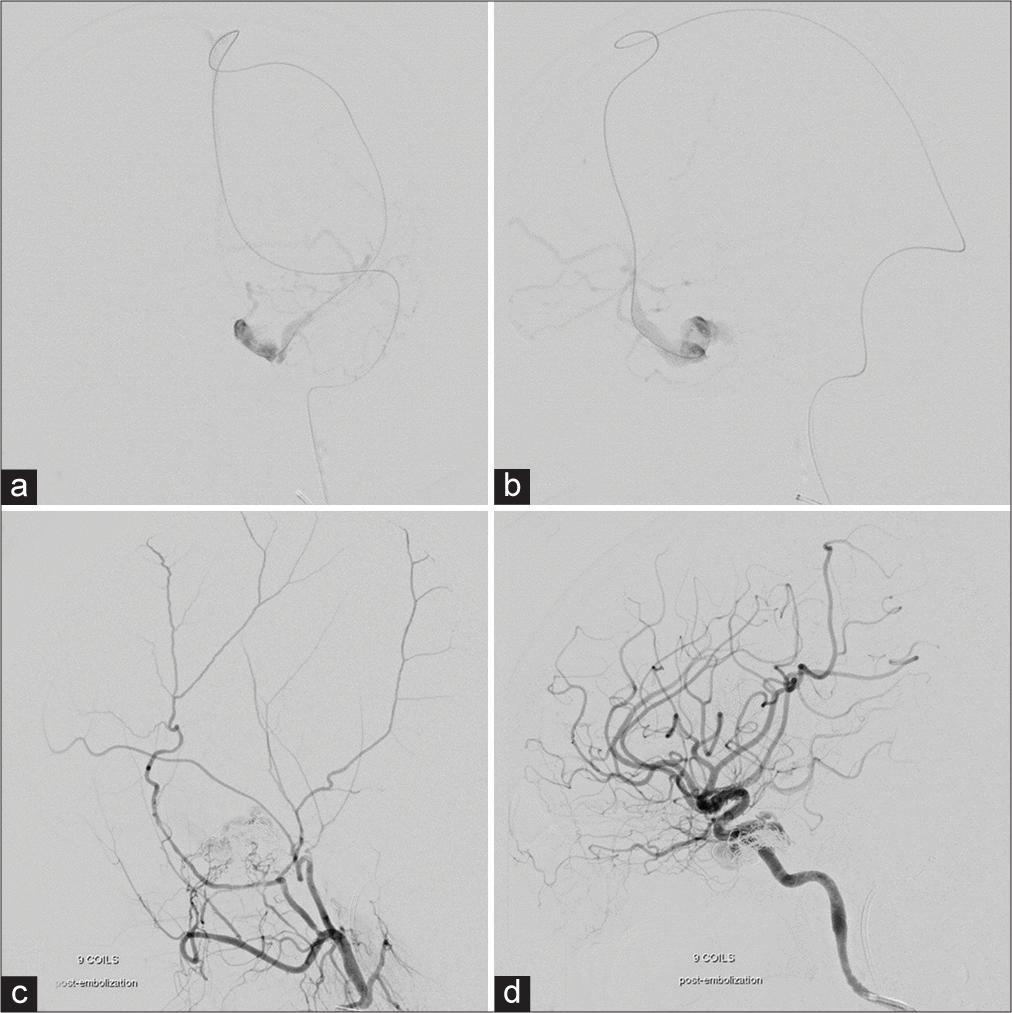
Figure 3:
(a) Anteroposterior and (b) lateral views of venography revealed the affected cavernous sinus after successful navigation of the tip of the microcatheter into the cavernous sinus through the left vein of Trolard and superficial middle cerebral vein. Lateral views of the (c) external and (d) internal carotid arteries injections following the embolization with coils demonstrate significant reduction of the shunt flow.
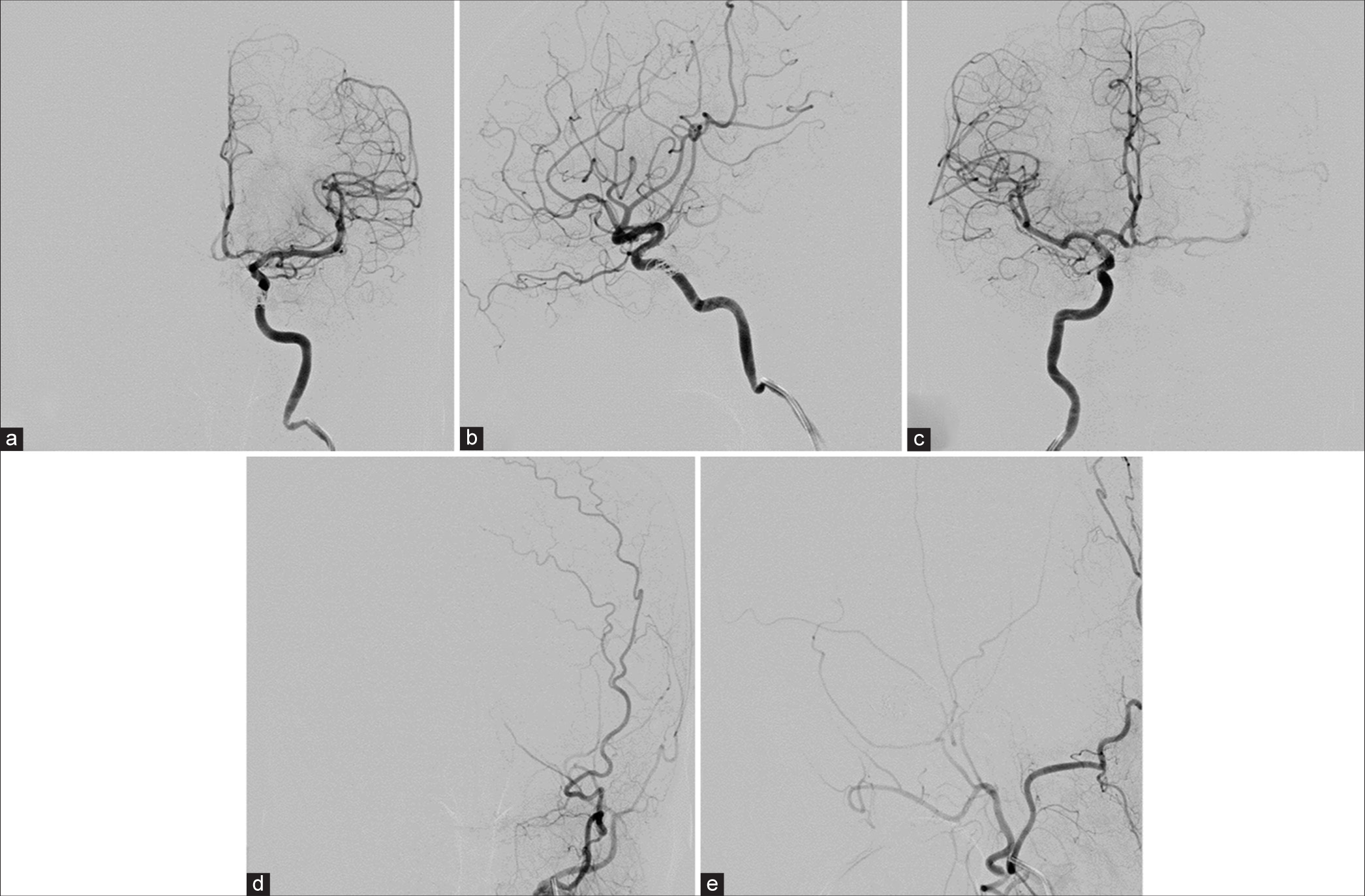
Figure 4:
Cerebral angiography obtained 6 months after embolization. (a) Anteroposterior (AP) and (b) lateral views of the left internal carotid artery (ICA), (c) AP view of the right ICA, and (d) AP and (e) lateral views of the left external carotid artery confirm complete obliteration of the cavernous sinus arteriovenous fistula.
DISCUSSION
The access route for transvenous embolization of CSDAVFs depends on the patency of the accessible drainage pathways of the CS.[
In our case, percutaneous transvenous access to the fistula through IPS was attempted but failed. Without other accessible routes, we decided to access the fistula through the superficial cerebral vein which its diameter was quite large enough to advance the microcatheter. However, we considered more invasive transcranial transcortical venous approach in case of unsuccessful attempt of percutaneous transvenous access through the cortical vein.
The vein of Trolard, superior anastomotic vein, is the largest superficial vein crossing the cortical surface of the frontal and parietal lobes between the superior sagittal sinus and SMCV.[
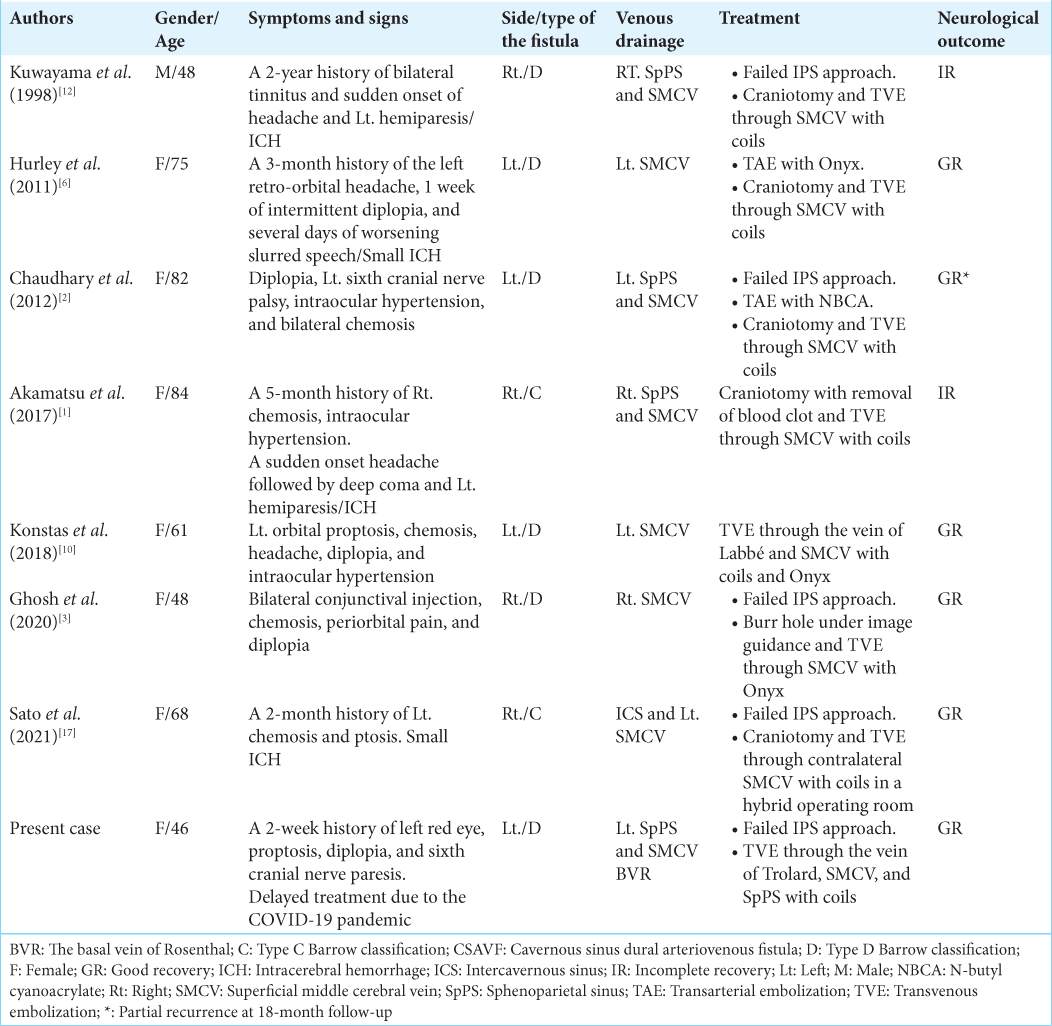
We reviewed the published studies in English language with sufficient information about CSDAVFs treated with transvenous embolization through SMCV [
The technological advances in microcatheter design, embolic materials, and fluoroscopic imaging equipment permit access to the CS through multiple routes, making endovascular treatment becoming the preferred treatment modality for CSDAVFs. The endovascular approach should be adjusted to individual case based on the angioarchitecture or angiographic features of the fistula.[
The aggravation of preexisting cranial nerve symptoms or new cranial nerve dysfunction may cause by the overpacking of embolic materials in the CS.[
CONCLUSION
To avoid invasive combined surgical and endovascular approach, transvenous embolization through the vein of Trolard and SMCV may be another accessible option for treating CSDAVF with isolated cortical venous drainage.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akamatsu Y, Sato K, Endo H, Matsumoto Y, Tominaga T. Single-session hematoma removal and transcranial coil embolization for a cavernous sinus dural arteriovenous fistula: A technical case report. World Neurosurg. 2017. 104: 1046.e7-12
2. Chaudhary N, Lownie SP, Bussière M, Pelz DM, Nicolle D. Transcortical venous approach for direct embolization of a cavernous sinus dural arteriovenous fistula: Technical case report. Neurosurgery. 2012. 70: 343-8
3. Ghosh R, Al Saiegh F, Mahtabfar A, Mouchtouris N, Khanna O, Sweid A. Burr hole-assisted direct transsylvian venous catheterization for carotid-cavernous fistula embolization: A case report. Oper Neurosurg (Hagerstown). 2020. 19: E196-200
4. Guo H, Yin Q, Liu P, Guan N, Huo X, Li Y. Focus on the target: Angiographic features of the fistulous point and prognosis of transvenous embolization of cavernous sinus dural arteriovenous fistula. Interv Neuroradiol. 2018. 24: 197-205
5. Halbach VV, Higashida RT, Hieshima GB, Hardin CW, Pribram H. Transvenous embolization of dural fistulas involving the cavernous sinus. AJNR Am J Neuroradiol. 1989. 10: 377-83
6. Hurley MC, Rahme RJ, Fishman AJ, Batjer HH, Bendok BR. Combined surgical and endovascular access of the superficial middle cerebral vein to occlude a high-grade cavernous dural arteriovenous fistula: Case report. Neurosurgery. 2011. 69: E475-81
7. Iampreechakul P, Tirakotai W, Tanpun A, Wattanasen Y, Lertbusayanukul P, Siriwimonmas S. Spontaneous resolution of direct carotid-cavernous fistulas: Case series and literature review. Interv Neuroradiol. 2019. 25: 71-89
8. Iampreechakul P, Wangtanaphat K, Lertbutsayanukul P, Wattanasen Y, Siriwimonmas S. Spontaneous closure of a cavernous sinus dural arteriovenous fistula with spinal perimedullary drainage (Cognard V) during attempted transvenous embolization. Asian J Neurosurg. 2019. 14: 1268-74
9. Jia ZY, Song YS, Sheen JJ, Kim JG, Lee DH, Suh DC. Cannulation of occluded inferior petrosal sinuses for the transvenous embolization of cavernous sinus dural arteriovenous fistulas: Usefulness of a frontier-wire probing technique. AJNR Am J Neuroradiol. 2018. 39: 2301-6
10. Konstas AA, Song A, Song J, Thanos A, Ross IB. Embolization of a cavernous carotid fistula through the vein of Labbé: A new alternative transvenous access route. J Neurointerv Surg. 2018. 10: e11
11. Korkmazer B, Kocak B, Tureci E, Islak C, Kocer N, Kizilkilic O. Endovascular treatment of carotid cavernous sinus fistula: A systematic review. World J Radiol. 2013. 5: 143-55
12. Kuwayama N, Endo S, Kitabayashi M, Nishijima M, Takaku A. Surgical transvenous embolization of a cortically draining carotid cavernous fistula via a vein of the sylvian fissure. AJNR Am J Neuroradiol. 1998. 19: 1329-32
13. Matsumoto A, Okauchi M, Shindo A, Kawanishi M, Tamiya T. Cavernous sinus dural arteriovenous fistula treated by facial vein direct puncture: Case report and review of the literature. Interv Neuroradiol. 2017. 23: 301-6
14. Meyers PM, Halbach VV, Dowd CF, Lempert TE, Malek AM, Phatouros CC. Dural carotid cavernous fistula: Definitive endovascular management and long-term follow-up. Am J Ophthalmol. 2002. 134: 85-92
15. Newton TH, Hoyt WF. Dural arteriovenous shunts in the region of the cavernous sinus. Neuroradiology. 1970. 1: 71-81
16. Rhoton AL. The cerebral veins. Neurosurgery. 2002. 51: S159-205
17. Sato S, Kokubo Y, Kawanami K, Itagaki H, Yamada Y, Matsumoto Y. Hybrid surgical and endovascular approach via the contralateral superficial middle cerebral vein to occlude cavernous sinus dural arteriovenous fistula in a hybrid operating room: A case report. NMC Case Rep J. 2021. 8: 137-42
18. Shimizu Y. Superficial middle temporal vein as a pivotal route to embolize dural carotid-cavernous fistulas. J Clin Neurosci. 2021. 84: 106-10
19. White JB, Layton KF, Evans AJ, Tong FC, Jensen ME, Kallmes DF. Transorbital puncture for the treatment of cavernous sinus dural arteriovenous fistulas. AJNR Am J Neuroradiol. 2007. 28: 1415-7