- Division of Neurosurgery, Department of Clinical Neurosciences, Addenbrooke’s Hospital and University of Cambridge, Cambridge, United Kingdom,
- Department of General and Special Surgery, Faculty of Medicine, The Hashemite University, Zarqa, Jordan,
- Department of Neurosurgery, St George’s University Hospital NHS Foundation Trust, London, United Kingdom.
Correspondence Address:
Hugo Layard Horsfall
Department of Neurosurgery, St George’s University Hospital NHS Foundation Trust, London, United Kingdom.
DOI:10.25259/SNI_671_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hugo Layard Horsfall1, Aref-Ali Gharooni1, Alaa Al-Mousa2, Anan Shtaya3, Erlick Pereira3. Traumatic atlantoaxial rotatory subluxation in adults – A case report and literature review. 06-Nov-2020;11:376
How to cite this URL: Hugo Layard Horsfall1, Aref-Ali Gharooni1, Alaa Al-Mousa2, Anan Shtaya3, Erlick Pereira3. Traumatic atlantoaxial rotatory subluxation in adults – A case report and literature review. 06-Nov-2020;11:376. Available from: https://surgicalneurologyint.com/surgicalint-articles/10373/
Abstract
Background: Traumatic atlantoaxial rotatory subluxation (AARS) is extremely rare in adult versus pediatric populations. Patients usually present with post-traumatic neck pain and torticollis. Surgical management aims at reducing the deformity and stabilizing the spine utilizing external orthotics, and/or internal reduction/fixation.
Methods: A 65-year-old female fell downstairs at home. She complained of neck pain with right-sided tenderness and torticollis. The radiographic studies and CT scan demonstrated AARS. This led to an emergent open reduction with internal fixation at the C1-C2 level.
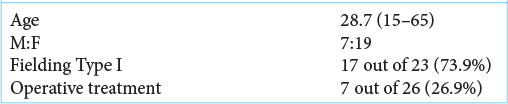
Results: We identified 25 similar cases of AARS in the English literature. Patients averaged 28.7 years of age and mostly sustained motor vehicle accidents largely treated with traction/orthotics; only six patients required surgical open reduction/internal fixation.
Conclusion: In this case, the patient’s C1-C2 deformity required open reduction/internal fixation rather than bracing alone.
Keywords: Atlantoaxial, Atlantoaxial dislocations, Atlantoaxial rotatory subluxation, Cervical spine, Rotatory, Subluxation, Trauma
INTRODUCTION
Atlantoaxial dislocations are a heterogeneous group of C1-C2 rotatory subluxations involving the inferior atlanto and superior axial facet articulations.[
Definitive management of such traumatic unilateral atlantoaxial rotatory subluxation (AARS) varies due to the unique biomechanics of these injuries; they often require an individualized approach.[
CASE REPORT
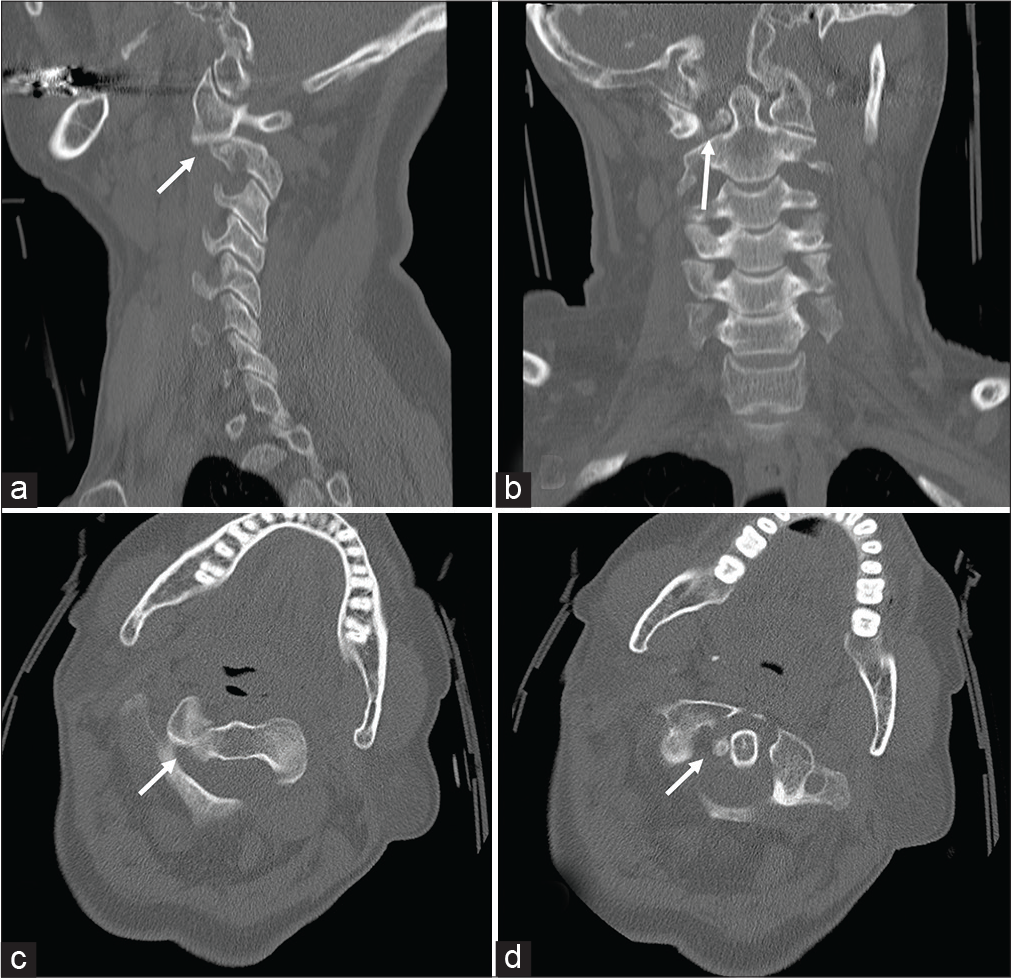
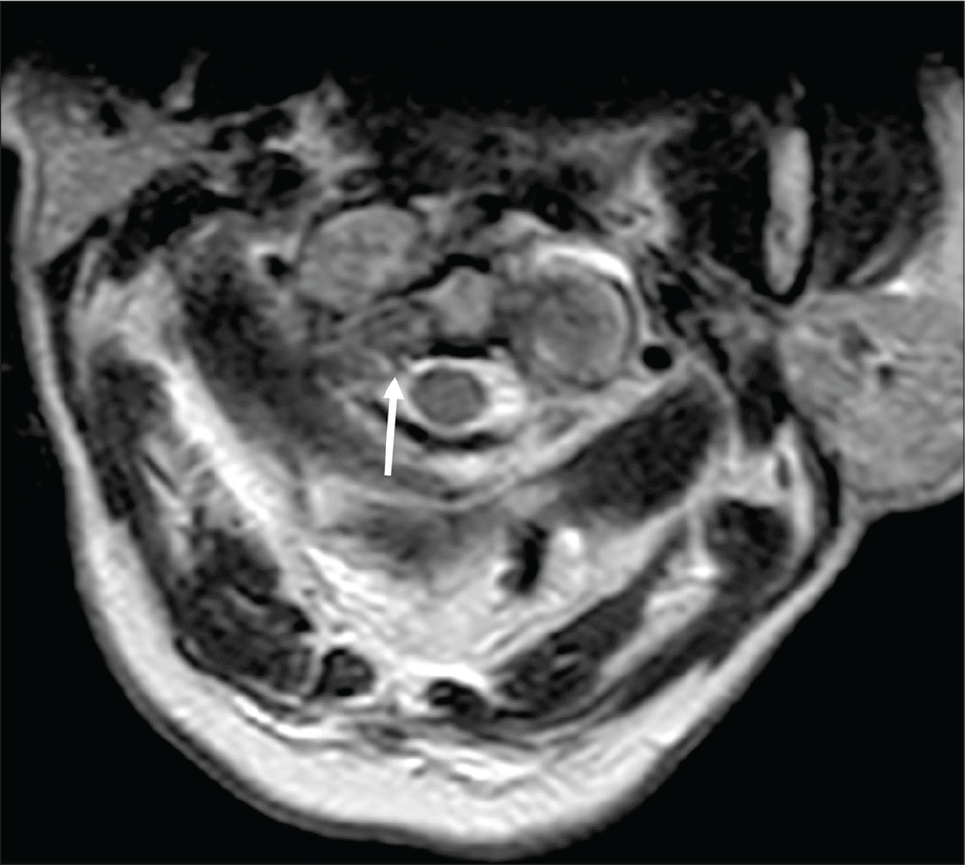
A 65-year-old female sustained a fall from ten steps at her home. She presented with stiffness/ neck pain and reduced range of movement. On examination, she had cervical (C5-C7) and thoracic (T7-L2) spine tenderness and torticollis toward the right. The neurological examination was normal. When plain films demonstrated a T11 fracture, she was placed in a TLSO. In addition, the CT showed a unilateral atlantoaxial rotatory subluxation with a locked right C1 facet and a right-sided intracanalicular bony fragment adjacent to the odontoid process [
Surgery
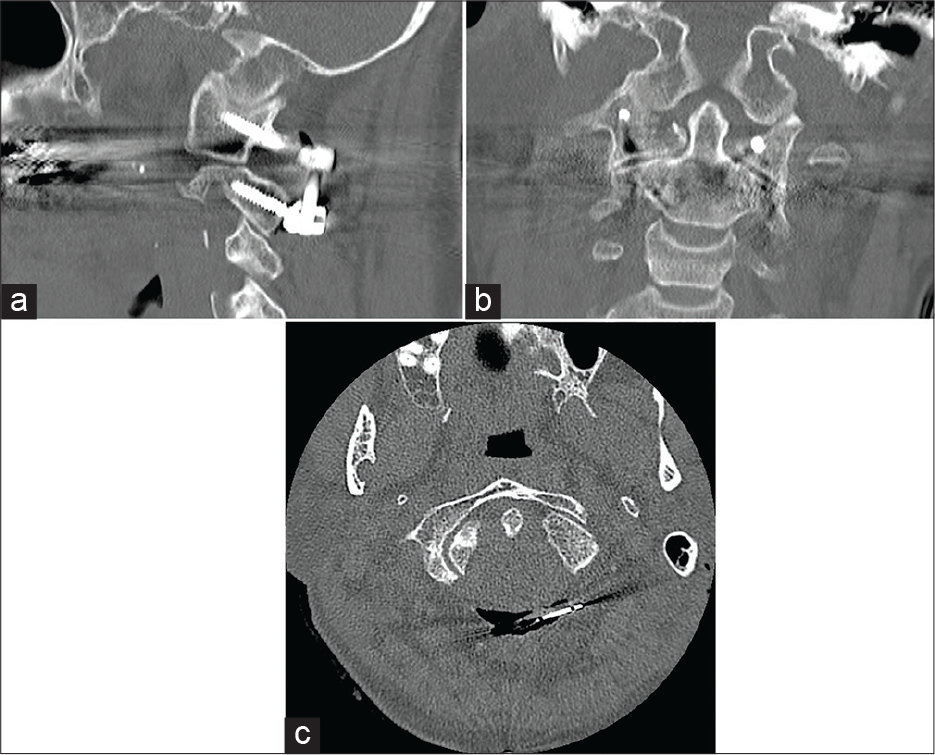
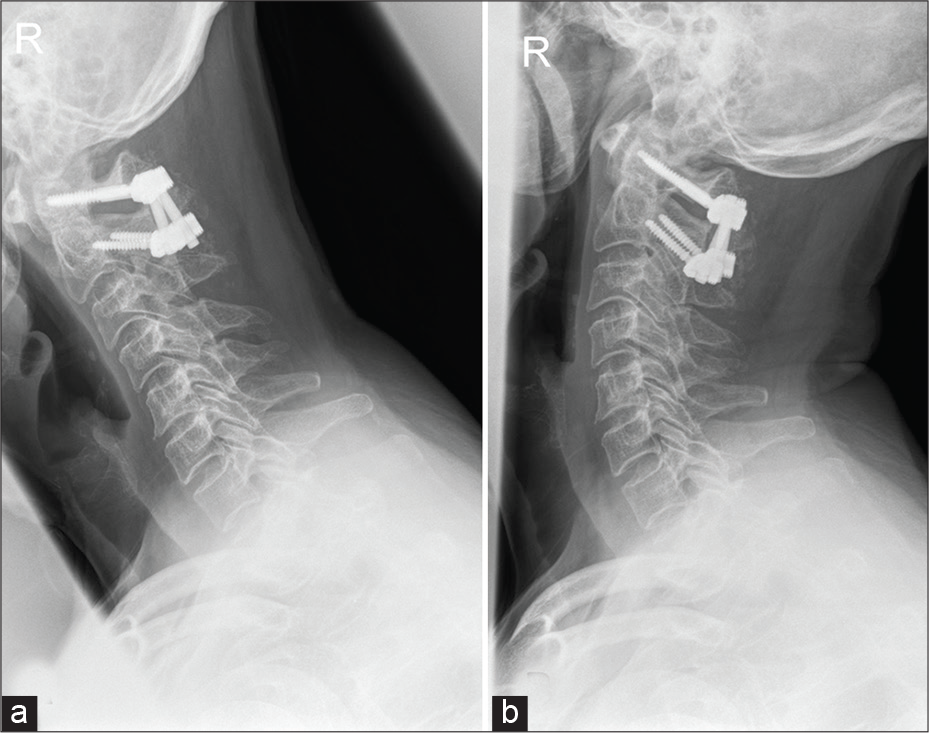
Within 24 h of the fall, and after a failed attempt at external reduction under general anesthesia, the patient underwent an open surgical reduction, and Harms-technique of C1-C2 fusion.[
DISCUSSION
Atlantoaxial subluxation is rare in the elderly, and early diagnosis and treatment are essential to ensure satisfactory neurological outcomes. Although CT remains the gold standard for documenting these injuries, those with suspected AARS should also undergo MRI for fuller evaluation of the attendant soft tissue injuries (e.g., ligamentous injuries, and/ or extent of spinal cord compression).[
Literature review of AARS
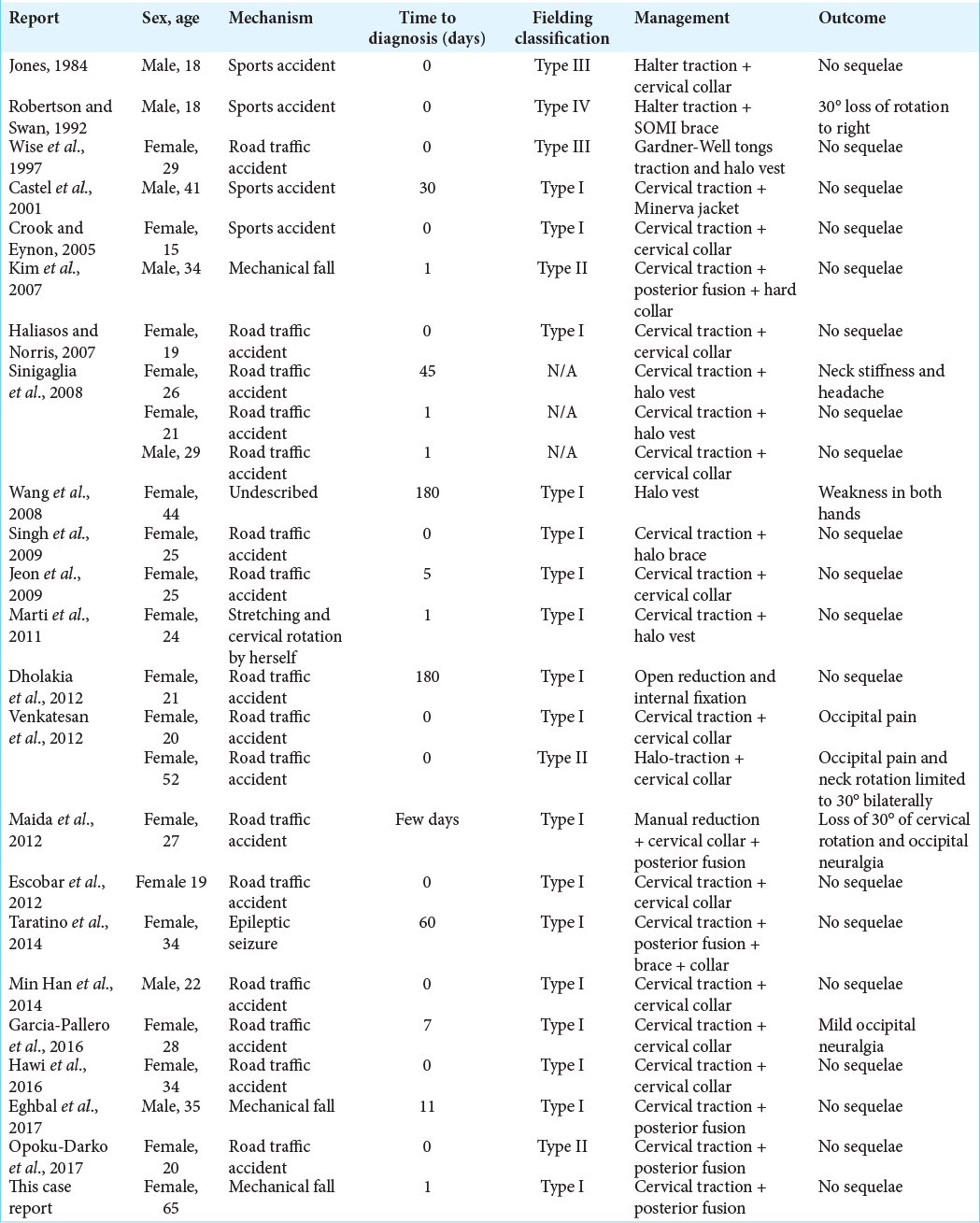
Using MEDLINE, we identified 25 adults who previously sustained C1-C2 AARS injuries [
CONCLUSION
AARS (especially Fielding I) following cervical trauma is rare in the elderly.
Both CT and MRI studies are essential for documenting the extent of C1-C2 injury, and there should be a low threshold for open operative reduction/fixation.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Chaudhary SB, Martinez M, Shah NP, Vives MJ. Traumatic atlantoaxial dislocation with hangman fracture. Spine J. 2015. 15: e15-8
2. García-Pallero MA, Torres CV, Delgado-Fernández J, Sola RG. Traumatic atlantoaxial rotatory fixation in an adult patient. Eur spine J. 2019. 28: 284-9
3. Missori P, Miscusi M, Paolini S, DiBiasi C, Finocchi V, Peschillo S. A C1-2 locked facet in a child with atlantoaxial rotatory fixation. Case report. J Neurosurg. 2005. 103: 563-6
4. Sikander M, Martin S, Dabbous B, Griffiths S, Pereira SK, Cadoux-Hudson T. Combined C1-C2 transarticular with C1 lateral mass screw fixation for the treatment of atlantoaxial instability: A single center experience. J Spinal Surg. 2016. 3: 133-9
5. Singh VK, Singh PK, Balakrishnan SK, Leitao J. Traumatic bilateral atlantoaxial rotatory subluxation mimicking as torticollis in an adult female. J Clin Neurosci. 2009. 16: 721-2
6. Tarantino R, Donnarumma P, Marotta N, Missori P, Viozzi I, Landi A. Atlanto axial rotatory dislocation in adults: A rare complication of an epileptic seizure-case report. Neurol Med Chir (Tokyo). 2014. 54: 413-6