- Department of Neurosurgery, Juntendo University Urayasu Hospital, Chiba, Japan.
- Department of Neurological Surgery, Juntendo University and Graduate School of Medicine, Tokyo, Japan.
Correspondence Address:
Senshu Nonaka, Department of Neurosurgery, Juntendo University Urayasu Hospital, Chiba, Japan.
DOI:10.25259/SNI_662_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Senshu Nonaka1, Hidenori Oishi2, Satoshi Tsutsumi1, Hisato Ishii1. Traumatic cervical vertebral artery aneurysm associated with suicidal stabs. 06-Sep-2021;12:452
How to cite this URL: Senshu Nonaka1, Hidenori Oishi2, Satoshi Tsutsumi1, Hisato Ishii1. Traumatic cervical vertebral artery aneurysm associated with suicidal stabs. 06-Sep-2021;12:452. Available from: https://surgicalneurologyint.com/surgicalint-articles/11089/
Abstract
Background: Cervical vertebral artery (VA) aneurysm occasionally develops in association with penetrating injury. However, its treatment strategy is not yet determined.
Case Description: A 50-year-old woman with bipolar disorder attempted suicide by stabbing herself in the lateral neck. At presentation, focal neurological deficits were not observed. Spinal computed tomography (CT) showed unclear delineation of the VA in the right C4/5 intervertebral foramen. CT performed 7 days later identified an aneurysm of the right VA at C4/5, with abnormal arteriovenous shunts between the aneurysm and paravertebral venous plexus. The patient underwent coil embolization of the VA segment involving the aneurysm on the same day that was complicated by cerebellar ataxia due to procedure-associated infarction.
Conclusion: Traumatic VA aneurysms associated with penetrating injuries should be carefully managed with a detailed presurgical evaluation of the relevant cranial and spinal structures.
Keywords: C4/5 intervertebral foramen, Cervical vertebral artery, Coil embolization, Penetrating injury
INTRODUCTION
Vertebral artery (VA) injury can be caused by trauma involving the head-and-neck regions. Most extra-cranial VA injuries are known to occur due to penetrating injuries with knives. Although infrequent, such VA injuries have been managed as distinct entities that can result in a pseudoaneurysm and subsequent stroke.[
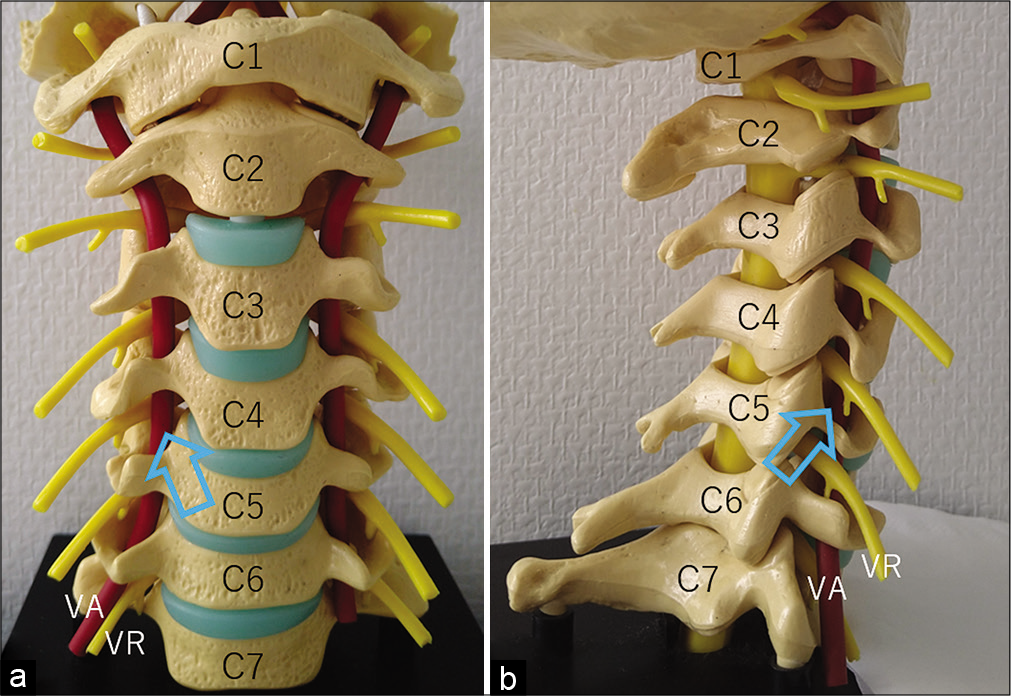
The three-dimensional morphology and size of the intervertebral foramina differ at each level from C2/3 to C6/7 [
Figure 1:
Frontal (a) and right posterolateral (b) views of cervical spine model showing the right C4/5 intervertebral foramen (arrow) where the vertebral artery segment is lying in the anteromedial aspect of the spinal ventral root. The three-dimensional morphology and size of the right intervertebral foramina are different at each level between C2/3 and C6/7. VA: Vertebral artery, VR: Ventral root.
Here, we present a unique case of traumatic cervical VA aneurysm that developed following penetrating injuries with a knife and was treated with coil embolization.
CASE PRESENTATION
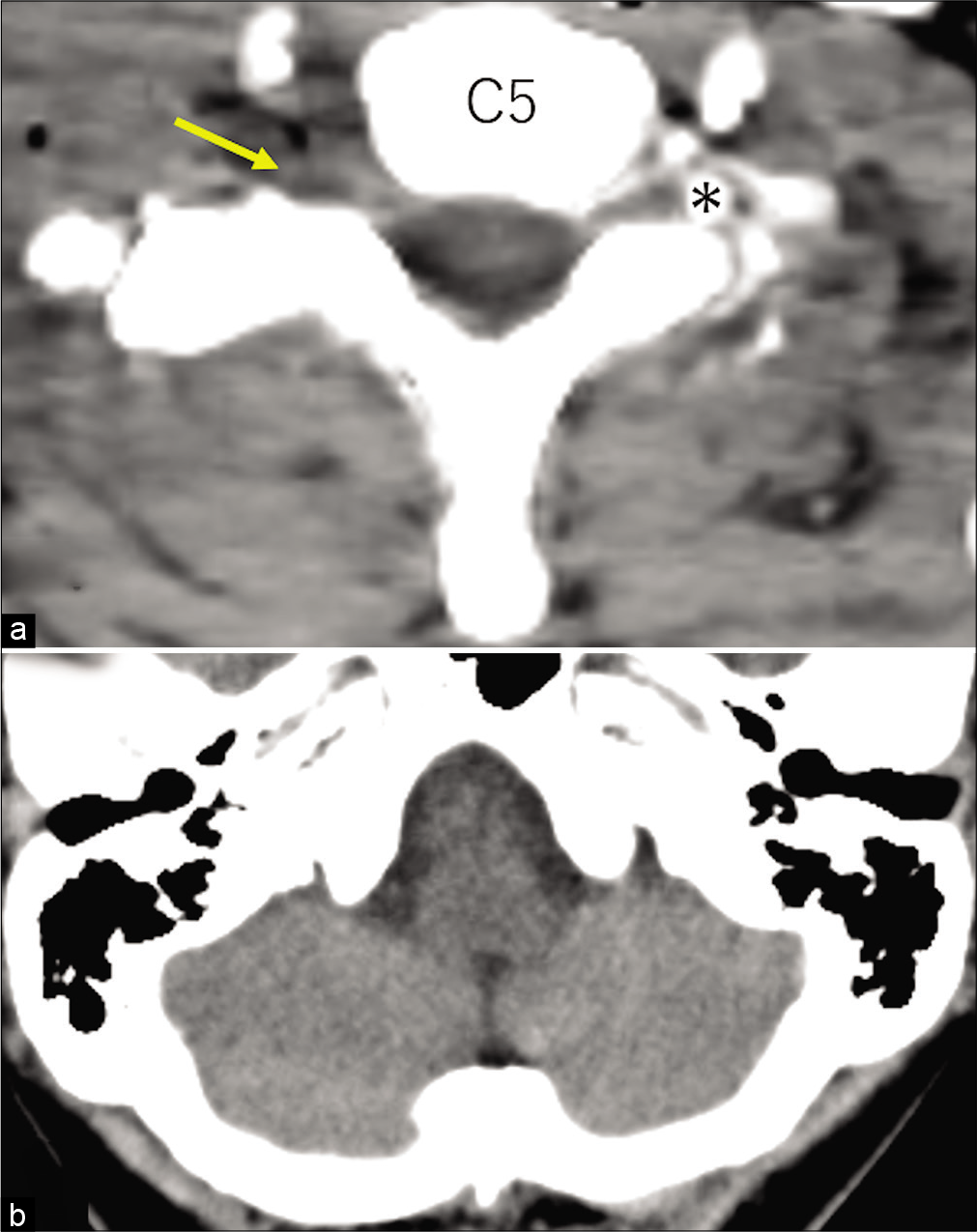
A 50-year-old woman with bipolar disorder attempted suicide by stabbing herself in the lateral neck with a stainless-steel fruit knife with a 15 cm long blade. The patient was emergently transported to our hospital on the day. At presentation, the patient was awake, with 14 points on the Glasgow Coma Scale, and did not present focal neurological deficits. Her blood pressure was 96/42 mmHg, and her serum hemoglobin level was 11.4 g/dl. Four stab wounds were identified on the lateral surface of her neck, but active bleeding was not observed. The spinal CT at presentation revealed crushed paraspinal soft tissues around the right C4/5 intervertebral foramen with unclear delineation of the VA [
Figure 2:
(a) Post-contrast axial computed tomography at the C5 level showing crushed paraspinal soft tissues around the right C4/5 intervertebral foramen with unclear delineation of the right vertebral artery (arrow). No extravasation of contrast agent is observed. (b) Non-contrast axial computed tomography of the head showing no abnormal findings in the lower cerebellum. Asterisk: Left vertebral artery.
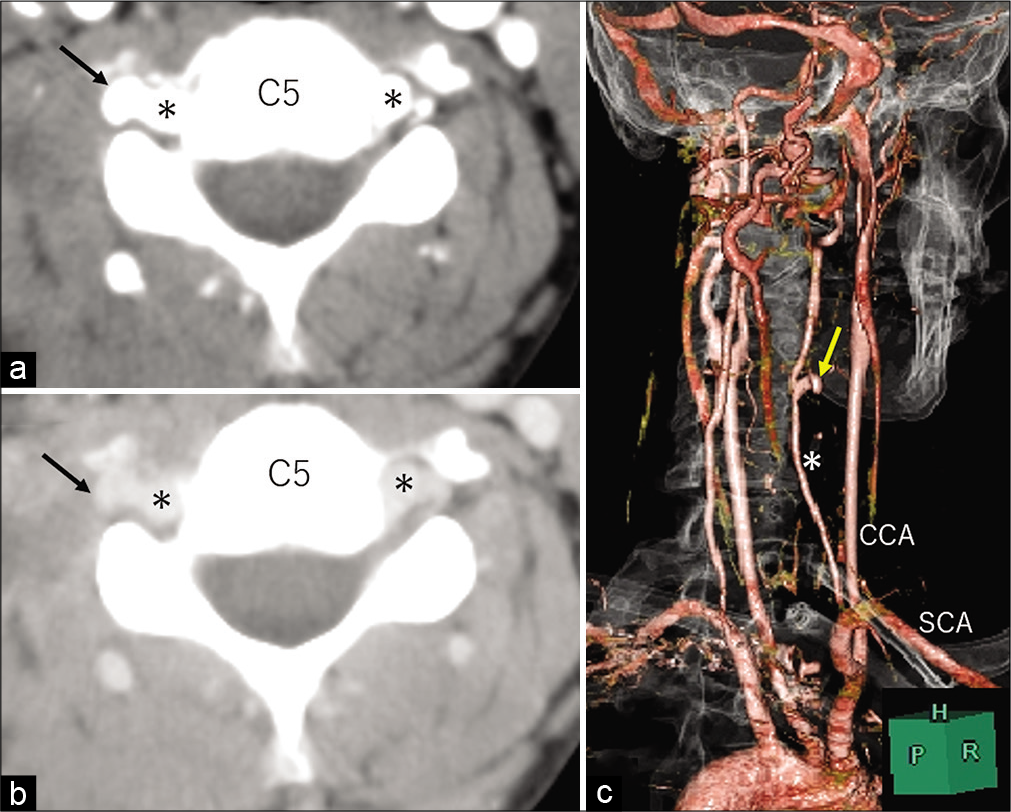
Figure 3:
Post contrast axial computed tomography at the C5 level (a) and its delayed-phase image (b) showing lateral protrusion of the right vertebral artery wall (arrow). (c) Three-dimensional computed tomography angiography, right posterolateral view, showing an aneurysm with a maximal dimension of 10 mm projecting laterally (arrow) at the C4/C5 level. Dominance between the vertebral arteries is not observed. CCA: common carotid artery, H: head side, P: posterior, R: right, SCA: subclavian artery, Asterisk: vertebral artery.
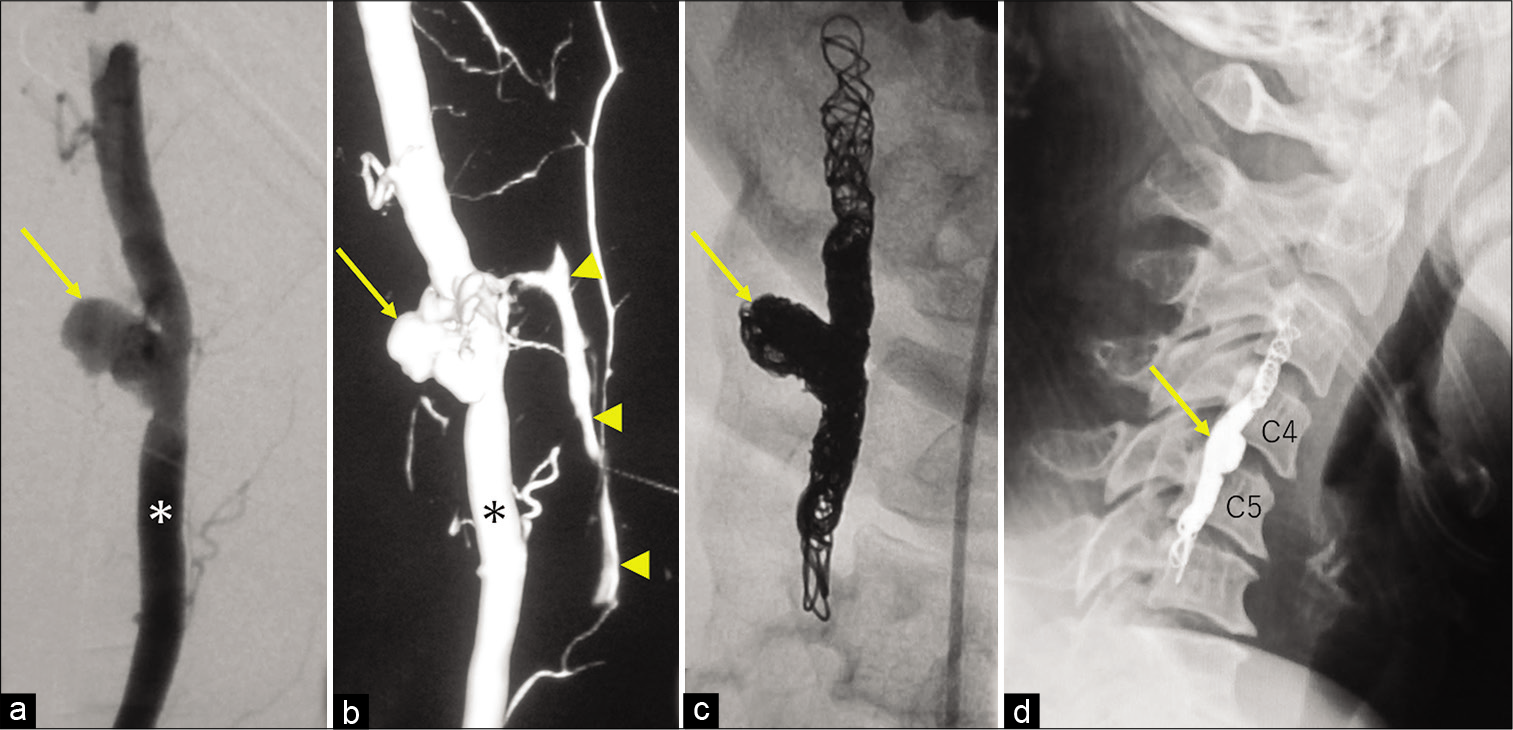
Figure 4:
Intraprocedural images. (a) Right vertebral arteriogram, oblique view, showing a broad-based aneurysm with an irregular contour (arrow). (b) Three-dimensional right vertebral angiogram, oblique view, showing abnormal shunts formed between the aneurysm (arrow) and paravertebral venous plexus (arrowheads). Oblique view of the right vertebral arteriogram (c) and lateral view of the cervical X-ray (d) showing obliteration of the vertebral artery segment involving the aneurysm (arrow). Asterisk: Vertebral artery.
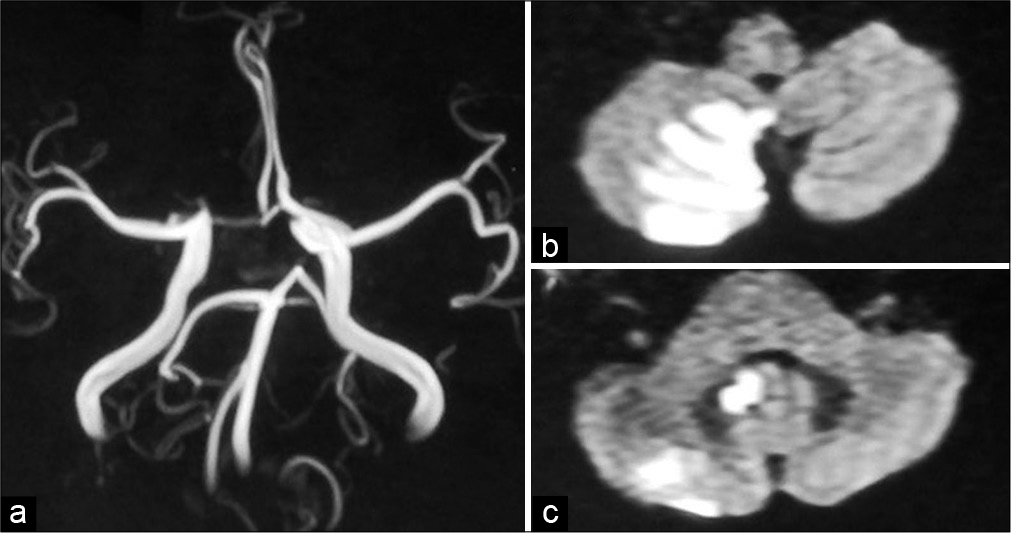
Figure 5:
Cerebral magnetic resonance angiography (a) performd immediately after surgery showing the intact flow of the right vertebral artery, while not detecting the posterior inferior cerebellar artery. Axial diffusion-weighted magnetic resonance image (b and c) showing an infarct in the distribution area of the right posterior inferior cerebellar artery.
DISCUSSION
In the present case, an initially undetected VA aneurysm, accompanied by abnormal arteriovenous shunts between the aneurysm and paravertebral venous plexus, appeared at the site of injury 7 days following penetrating injury. Therefore, the aneurysm was thought to be a traumatic pseudoaneurysm that developed in association with the preceding penetrating injury by a knife. Piper et al. described that VA injuries, especially penetrating injuries by gunshots and stabbings, were rare but considerably devastating. Mortality rates associated with penetrating VA injury were documented to be 3–19%, but they may be underestimated for associated brainstem infarction that results in a rapid death before hospitalization.[
The traumatic aneurysm appeared in the absence of spinal instability, suggesting the need for prompt management to prevent possible ischemic stroke. Radiologically, dominance was not found between the VAs. In contrast, substantial retrograde blood flow from the left VA was observed on occlusion of the right VA. Therefore, we assumed, as previous report, that obliteration of the VA segment involving the aneurysm would be tolerated by the patient without confirmation by antecedent balloon test occlusion.[
The cross-sectional areas of the intervertebral foramina are documented to be narrow at the C4/5.[
CONCLUSION
Traumatic VA aneurysms associated with penetrating injuries should be carefully managed with a detailed presurgical evaluation of the relevant cranial and spinal structures.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Enicker B, Gonya S, Hardcastle TC. Spinal stab injury with retained knife blades: 51 consecutive patients managed at a regional referral unit. Injury. 2015. 46: 1726-33
2. Fassett DR, Dailey AT, Vaccaro AR. Vertebral artery injuries associated with cervical spine injuries: A review of the literature. J Spinal Disord Tech. 2008. 21: 252-8
3. Knapik DM, Abola MV, Gordon ZL, Seiler JG, Marcus RE, Liu RW. Differences in cross-sectional intervertebral foraminal area from C3 to C7. Global Spine J. 2018. 8: 600-6
4. Leiderman DB, Zerati AE, Wolosker N, Hoffmann Melo HA, da Silva ES, de Luccia N. Endovascular treatment of penetrating injury to the vertebral artery by a stab wound: Case report and literature review. Ann Vasc Surg. 2017. 45: 267.e.1-5
5. Majidi S, Hassan AE, Adil MM, Jadhav V, Qureshi AI. Incidence and outcome of vertebral artery dissection in trauma setting: Analysis of national trauma data base. Neurocrit Care. 2014. 21: 253-8
6. Matsushima K, Matsuo S, Komune N, Kohno M, Lister JR. Variations of occipital artery-posterior inferior cerebellar artery bypass: Anatomic consideration. Oper Neurosurg (Hagerstown). 2018. 14: 563-71
7. Múnera F, Soto JA, Palacio D, Velez SM, Medina E. Diagnosis of arterial injuries caused by penetrating trauma to the neck: Comparison of helical CT angiography and conventional angiography. Radiology. 2000. 216: 356-62
8. Mwipatayi BP, Jeffery P, Beningfield SJ, Motale P, Tunnicliffe J, Navsaria PH. Management of extra-cranial vertebral artery injuries. Eur J Vasc Endovasc Surg. 2004. 27: 157-62
9. Núñez DB, Torres-León M, Múnera F. Vascular injuries of the neck and thoracic inlet: Helical CT-angiographic correlation. Radiographics. 2004. 24: 1087-98
10. Olteanu-Nerbe V, Bauer M, Vogl T, Marguth F. Endovascular treatment of traumatic arterio-venous fistulas of the vertebral artery. Neurosurg Rev. 1993. 16: 267-73
11. Piper K, Rabil M, Ciesla D, Agazzi S, Ren Z, Mokin M. Penetrating vertebral artery injuries: A literature review and proposed treatment algorithm. World Neurosurg. 2021. 148: e518-26
12. Uchikawa H, Kai Y, Ohmori Y, Kuratsu JI. Strategy for endovascular coil embolization of a penetrating vertebral artery injury. Surg Neurol Int. 2015. 6: 117
13. Vellimana AK, Lavie J, Chatterjee AR. Endovascular considerations in traumatic injury of the carotid and vertebral arteries. Semin Intervent Radiol. 2021. 38: 53-63
14. Xia X, Zhang F, Lu F, Jiang J, Wang L, Ma X. Stab wound with lodged knife tip causing spinal cord and vertebral artery injuries: Case report and literature review. Spine (Phila Pa 1976). 2012. 37: E931-4
15. Xu N, Zhang K, Meng H, Liu T, Wang H. Treatment of spontaneous dissecting aneurysm in extracranial vertebral artery with covered stent. World Neurosurg. 2018. 110: e330-2
16. Zoarski GH, Seth R. Safety of unilateral endovascular occlusion of the cervical segment of the vertebral artery without antecedent balloon test occlusion. AJNR Am J Neuroradiol. 2014. 35: 856-61