- Department of Ortho-Spine Surgery, Sir Ganga Ram Hospital, New Delhi, India.
DOI:10.25259/SNI_298_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Vishnu Prasad Panigrahi, Nitin Adsul, R. S. Chahal, K. L. Kalra, Shankar Acharya. Traumatic posterior dislocation of sacrococcygeal joint: A case report and review of the literature. 18-Jul-2020;11:197
How to cite this URL: Vishnu Prasad Panigrahi, Nitin Adsul, R. S. Chahal, K. L. Kalra, Shankar Acharya. Traumatic posterior dislocation of sacrococcygeal joint: A case report and review of the literature. 18-Jul-2020;11:197. Available from: https://surgicalneurologyint.com/surgicalint-articles/10141/
Abstract
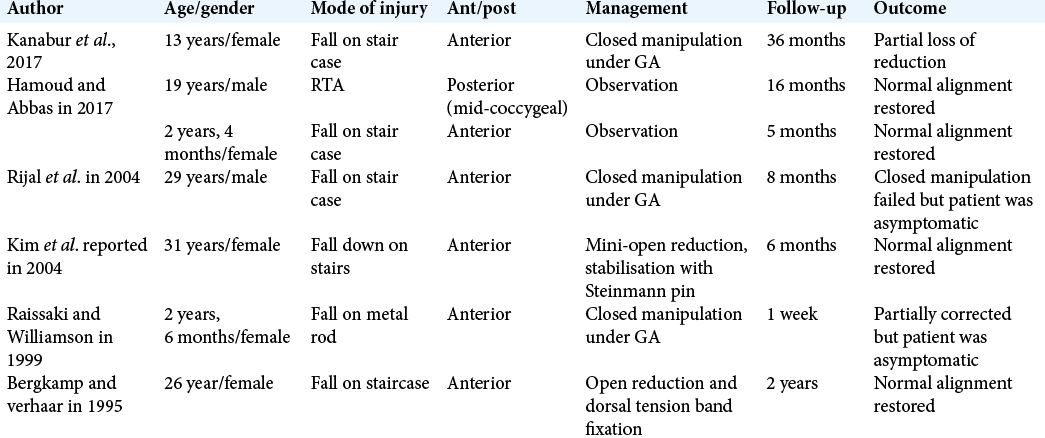
Background: Sacrococcygeal joint dislocation is very rare. There are seven cases of sacrococcygeal joint dislocation found in the literature; most are anterior, and only one prior case of posterior dislocation was reported involving the mid-coccygeal joint. Here, we report another case of posterior dislocation of the sacrococcygeal joint.
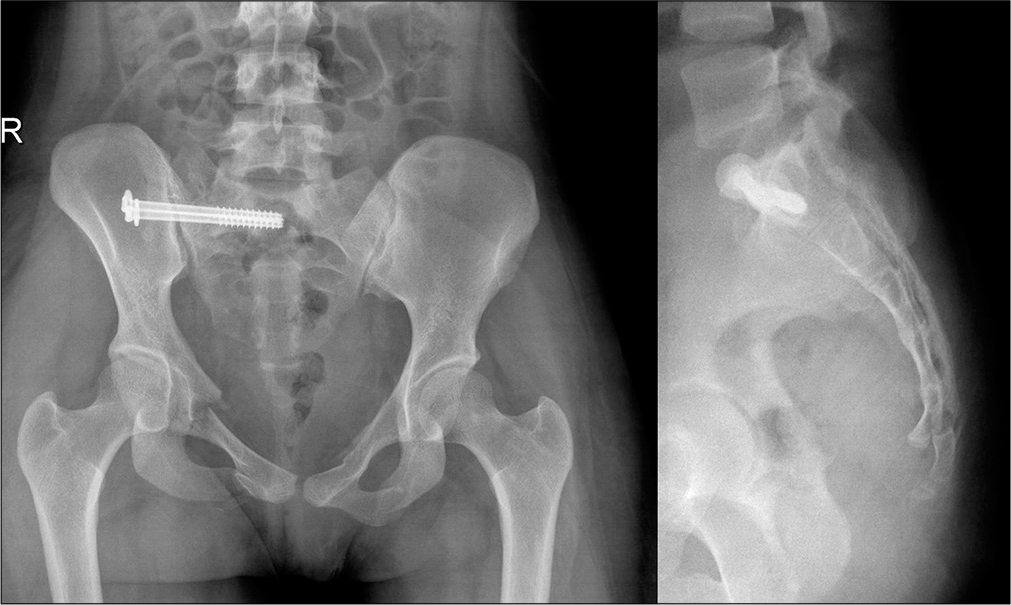
Case Description: A 19 year-old female developed acute low-back and groin pain following a fall from the first floor. She was diagnosed with an unstable pelvic fracture along with posterior dislocation of the sacrococcygeal joint. The next day, after being hemodynamically stabilized, she underwent percutaneous fixation of the sacral fracture, while the sacrococcygeal joint dislocation was managed conservatively. Her pain decreased, and she was discharged on the third postoperative day and followed up to 6 weeks.
Conclusion: Most sacrococcygeal joint dislocations can be managed conservatively.
Keywords: Coccyx, Posterior sacrococcygeal joint dislocation, Sacrococcygeal joint
INTRODUCTION
The sacrococcygeal symphysis is a fibrocartilaginous joint that connects the apex of the sacrum to the coccyx.[
CASE DESCRIPTION
A 19-year-old female sustained a fall from the first floor of her home. She presented with acute lower back and groin pain. The pelvic X-rays [
DISCUSSION
Sacrococcygeal dislocation has no standard treatment guidelines. There are only isolated case reports that show the equal success of conservative[
Rijal et al.,[
Here, the authors concluded that fracture–dislocations of the coccyx in young adults could be effectively treated conservatively and avoided performing a closed reduction due to their high failure rates.[
CONCLUSION
In this case, a 19-year-old female underwent sacral fracture reduction with percutaneous placed double iliosacral screw fixation, while the sacrococcygeal posterior dislocation was managed conservatively.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bergkamp A, Verhaar J. Dislocation of the coccyx: A case report. J Bone Joint Surg Br. 1995. 77: 831-2
2. Hamoud K, Abbas J. Fracture dislocations of the coccyx: A case series and literature review. J Clin Case Rep. 2017. 7: 1005-
3. Kanabur P, Gowd A, Bulkeley JA, Behrend CJ, Carmouche JJ. Symptomatic sacrococcygeal joint dislocation treated using closed manual reduction: A case report with 36-month follow-up and review of literature. Trauma Case Rep. 2017. 12: 11-5
4. Kim WY, Han CW, Kim YH. Joystick reduction and percutaneous pinning for an acutely anteriorly dislocated coccyx: A case report. J Orthop Trauma. 2004. 18: 388-9
5. Raissaki MT, Williamson JB. Fracture dislocation of the sacro-coccygeal joint: MRI evaluation. Pediatr Radiol. 1999. 29: 642-3
6. Rijal K, Pradhan R, Sharma S, Lakhey S, Pandey B. Acute sacrococcygeal dislocation (anterior type): A case report. Kathmandu Univ Med J (KUMJ). 2004. 2: 367-8
7. Sinnatamby CS.editors. Last’s Anatomy E-Book: Regional and Applied. Amsterdam: Elsevier Health Sciences; 2011. p.
8. Standring S, Ellis H, Healy J, Johnson D, Williams A.editors. Gray’s Anatomy. London: Churchill Livingstone, Elsevier; 2008. p.