- Department of Neurosurgery, Hacettepe University, Ankara, Turkey.
Correspondence Address:
Muhammet Enes Gurses, Department of Neurosurgery, Hacettepe University, Ankara, Turkey.
DOI:10.25259/SNI_186_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Muhammet Enes Gurses, Siyar Bahadir, Burcak Bilginer. Traumatic subgaleal hematoma in patient with Ehlers-Danlos syndrome: A rare case report. 23-Jun-2022;13:265
How to cite this URL: Muhammet Enes Gurses, Siyar Bahadir, Burcak Bilginer. Traumatic subgaleal hematoma in patient with Ehlers-Danlos syndrome: A rare case report. 23-Jun-2022;13:265. Available from: https://surgicalneurologyint.com/surgicalint-articles/11672/
Abstract
Background: A subgaleal hematoma (SGH) describes scalp bleeding in the potential space between the periosteum and the galea aponeurosis. This hematoma generally occurs after vacuum-assisted and forceps delivery, but may also be seen following head trauma. Despite its benign course, SGHs may complicate by life-threatening events.
Case Description: We report a case of a 10-year-old male with Ehlers-Danlos syndrome presenting with scalp swelling following minor head trauma. On examination, a small swelling was observed in the occipital region. During the follow up, as the volume of subgaleal hematoma was increasing, we performed needle aspiration to achieve volume reduction, and dressed with a cap like bandage that wrapped and compressed scalp. The patient was hospitalized due to hemodynamic instability and a blood transfusion was performed. Due to extended usage of compressive bandage, a large area of scalp tissue became necrotic. The necrotic scalp tissue was debrided and reconstructed by plastic and reconstructive surgery. After surgery, another hematoma formed extending from the front of the ear to the ipsilateral neck caused facial paralysis, this hematoma was evacuated and a drain was placed. The patient was followed up for 1 year and no recurrent cephalhematoma was observed.
Conclusion: Ehlers-Danlos is a rarely encountered connective tissue syndrome, this case underscores the importance for neurosurgery physicians to recognize the potential catastrophes, these patients may present with following even minor injury.
Keywords: Ehlers-Danlos syndrome, Pediatric neurosurgery, Subgaleal hematoma, Trauma
INTRODUCTION
A subgaleal hematoma (SGH) is generally related to head trauma. The galea in a newborn can be pulled out in a vertical plane and slipped in a tangential direction when vulnerable to an external force as the scalp is tender, the subcutis and periosteum are sensitive, and there is a fragile connection between these tissues. In case of an injured vein, a subcutaneous hematoma may occur; therefore, the infant is sensitive to an SGH or subperiosteal hematoma. A few cases have been described in older children, occasionally as a result of minor head trauma such as hair braiding or hair pulling.[
CASE PRESENTATION
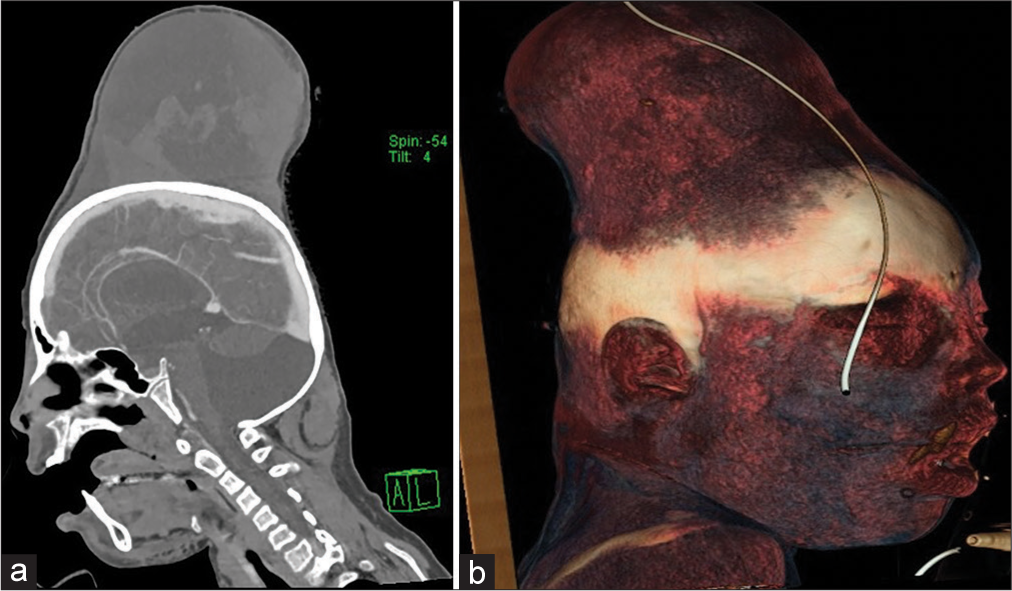
A 10-year-old boy was admitted to the Hacettepe University Department of Emergency following a minor head injury 1 h before arrival. He had fallen and striking the occipital region of his head on the edge of the table. He presented to the emergency department with a chief complaint of minor scalp swelling. On initial presentation, the patient’s vitals were within normal limits. He was awake and alert on admission. His neurological examination was normal excluding a minor swelling in the occipital region. His history also revealed joint hypermobility, fatigue, syncope, easy bruising, and hematoma formation resulting from minor trauma due to Ehlers-Danlos syndrome. The patient was consulted to our neurosurgery department within half an hour on admission. A stat computed tomography (CT) of the brain with the angiographic study was ordered. A CT showed no intracranial hemorrhage. The neurosurgery team decided to wrap a compressive bandage around his head in an attempt to stop the bleeding by compression. After around ½ h, the neurosurgery team was contacted again, only to be informed that the compressive bandage did not stop swelling. The scalp started to swell over the bandage. A CT has performed again. There was a massive increase in blood volume in subgaleal space [
DISCUSSION
Ehlers-Danlos syndrome is a collagen tissue disorder described by Job van Meekeren.[
Anatomically, the subgaleal area binds the cranial periosteum and the galea aponeurotica. The subgaleal area includes loose connective tissue and minor emissary vessels connecting the extracranial venous system and the intracranial venous sinuses. SGH results from the impairment of these emissary veins. SGH expressed as a gathering of blood under the galea aponeurotica layer can be classified as nontraumatic or traumatic depending on the mechanism of the event. Traumatic SGH can be caused by minor head trauma such as hair pulling[
In our case, the patient is 10 years old with a SGH in the occipital region. This is a rare case of traumatic SGH presenting in adolescence and this report describes a giant occipital SGH with protrusion and anemia in a 10-year-old boy for which we utilized a more conservative approach, which leads to compression necrosis and further complications. The clinical features of the patient were found to be compatible with the EDS Kosho type (EDSKT). The new Ehlers-Danlos syndrome, also known as EDSKT, is a connective tissue disorder that causes massive subcutaneous hematomas in individuals.[
CONCLUSION
Ehlers-Danlos syndrome is an uncommon connective tissue disorder. Our case underlines the importance for neurosurgeons to recognize the potential catastrophes of minor trauma in these patients.
DECLARATIONS
Statement of ethics
The authors have no ethical conflicts to disclose. Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Adeleye A. Subgaleal hematoma extending into the orbit following blunt head trauma as a cause of permanent blindness: A case illustrated review. Niger J Ophthalmol. 2017. 25: 1
2. Edmondson SJ, Ramman S, Hachach-Haram N, Bisarya K, Fu B, Ong J. Hair today; scalped tomorrow: Massive subgaleal haematoma following sudden hair pulling in an adolescent in the absence of haematological abnormality or skull fracture. J Craniofac Surg. 2016. 27: 1261-2
3. Felton BM, White JM, Jones RA. Cephalohematoma in a patient with ehlers-danlos syndrome. West J Emerg Med. 2013. 14: 419-20
4. Fujimoto S, Ota T, Mizutani T. Life-threatening large subcutaneous hematoma after minor head trauma: A young female patient who was suspected of having new EhlersDanlos syndrome. Asian J Neurosurg. 2015. 10: 148-50
5. Gupta P, Gleeson AP. A rare case of head injury associated with Ehlers-Danlos syndrome. Injury. 2000. 31: 641-3
6. Henderson FC, Austin C, Benzel E, Bolognese P, Ellenbogen R, Francomano CA. Neurological and spinal manifestations of the Ehlers-Danlos syndromes. Am J Med Genet Part C Semin Med Genet. 2017. 175: 195-211
7. Herrero FA. EEG changes in ehlers-danlos syndrome: A case study. Clin Electroencephalogr. 1973. 4: 57-61
8. Kato T, Hattori H, Yorifuji T, Tashiro Y, Nakahata T. Intracranial aneurysms in Ehlers-Danlos syndrome type IV in early childhood. Pediatr Neurol. 2001. 25: 336-9
9. Koizumi K, Suzuki S, Utsuki S, Nakahara K, Niki J, Mabuchi I. A case of non-traumatic subgaleal hematoma effectively treated with endovascular surgery. Interv Neuroradiol. 2010. 16: 317-21
10. Kosho T, Miyake N, Hatamochi A, Takahashi J, Kato H, Miyahara T. A new Ehlers-Danlos syndrome with craniofacial characteristics, multiple congenital contractures, progressive joint and skin laxity, and multisystem fragility-related manifestations. Am J Med Genet A. 2010. 152: 1333-46
11. Morel C, Rizk T, Fischer G. Giant cephalhaematoma in a 17-year-old boy with Ehlers-Danlos syndrome. Br J Neurosurg. 1998. 12: 54-5
12. Nakamura M, Yajima J, Oikawa Y, Ogasawara K, Uejima T, Abe K. Vascular Ehlers-Danlos syndrome. All three coronary artery spontaneous dissections. J Cardiol. 2009. 53: 458-62
13. Shimizu K, Okamoto N, Miyake N, Taira K, Sato Y, Matsuda K. Delineation of dermatan 4-O-sulfotransferase 1 deficient Ehlers-Danlos syndrome: Observation of two additional patients and comprehensive review of 20 reported patients. Am J Med Genet A. 2011. 155A: 1949-58
14. Van Meekeren JA.editors. De dilatabilitate extraordinaria cutis. Observations Mediochirugicae. Amsterdame. 1997. p. 82-105
15. Wimmer PJ, Howes DS, Rumoro DP, Carbone M. Fatal vascular catastrophe in Ehlers-Danlos syndrome: A case report and review. J Emerg Med. 1996. 14: 25-31