- Department of Neurosurgery, Warren Alpert Medical School, Brown University, Providence, Rhode Island, United States.
DOI:10.25259/SNI_119_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: David D. Liu, Joaquin Q. Camara-Quintana, Owen P. Leary, Sohail Syed, Adetokunbo A. Oyelese, Albert E. Telfeian, Ziya L. Gokaslan, Jared S. Fridley, Tianyi Niu. Traumatic unilateral jumped facet joint in the upper thoracic spine: Case presentation and literature review. 25-Apr-2020;11:77
How to cite this URL: David D. Liu, Joaquin Q. Camara-Quintana, Owen P. Leary, Sohail Syed, Adetokunbo A. Oyelese, Albert E. Telfeian, Ziya L. Gokaslan, Jared S. Fridley, Tianyi Niu. Traumatic unilateral jumped facet joint in the upper thoracic spine: Case presentation and literature review. 25-Apr-2020;11:77. Available from: https://surgicalneurologyint.com/surgicalint-articles/9976/
Abstract
Background: A jumped facet joint is defined by when the inferior articular process of the superior vertebra becomes locked anterior to the superior articular process of the inferior vertebra. These typically traumatic lesions are exceedingly rare in the thoracic spine. Here, we present a patient with a unilateral jumped facet joint in the upper thoracic spine treated with open reduction and an instrumented fusion.
Case Description: A 45-year-old male presented after a significant motor vehicle accident. In the emergency room, he had a Glasgow Coma Score of 13 without any neurologic deficit. The thoracic computed tomography (CT) showed a significant jumped left facet at the T2-T3 level. Two days later, utilizing intraoperative CT-guided navigation and neuromonitoring, he underwent open reduction of the T2-T3 jumped facet plus an instrumented T1-T5 fusion. X-rays taken 3-month postoperatively showed a stable construct. Six months postoperatively, he remained neurologically intact.
Conclusion: A unilateral jumped thoracic facet may be present in patients with fractured ribs. The mechanism of injury is most likely axial rotation. Both CT and magnetic resonance imaging studies allow for early detection of these very rare lesions and warrant open reduction and instrumented fusion.
Keywords: Jumped facet, Spinal trauma, Thoracic spinal dislocation, Unilateral thoracic facet dislocation
INTRODUCTION
A jumped facet joint occurs when the inferior articular process of the superior vertebra is locked anteriorly to the superior articular process of the inferior vertebra. A unilateral jumped facet reflects biomechanical disruption of the posterior spinal column with/without instability that can lead to cord injury.[
CASE DESCRIPTION
History and examination
A 45-year-old male presented to the emergency room following a front-end motor vehicle collision. The patient’s baseline Glasgow Coma Score was 13 (E:4, V:4, M:5); there were no reports of loss of consciousness or signs of head trauma and he remained neurologically intact.
Imaging
The thoracic computed tomography (CT) showed an anterior inferior corner fracture of the T2 vertebral body, jumped left T2- T3 facet, T2-T3 vertebral distraction (i.e., Arbeitsgemeinschaft für Osteosynthesefragen classification T2-T3C (T2: A1; N0),[
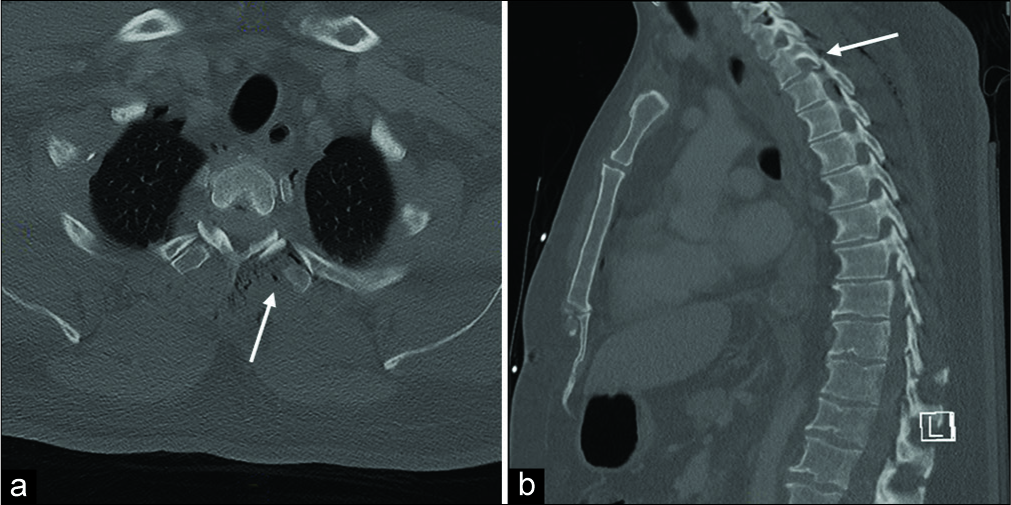
Figure 1:
Computed tomography from time of presentation. (a) Axial section at the T2-T3 level. The solid arrow points at the left T2-3 jumped facet showing the classic “empty facet sign” at the left facet joint. (b) Left paramedian sagittal section. The solid arrow shows the superior articulating facet of T3 situated superficial to the inferior articulating facet of T2, creating the “jumped” facet at T2-T3 and mild anterolisthesis.
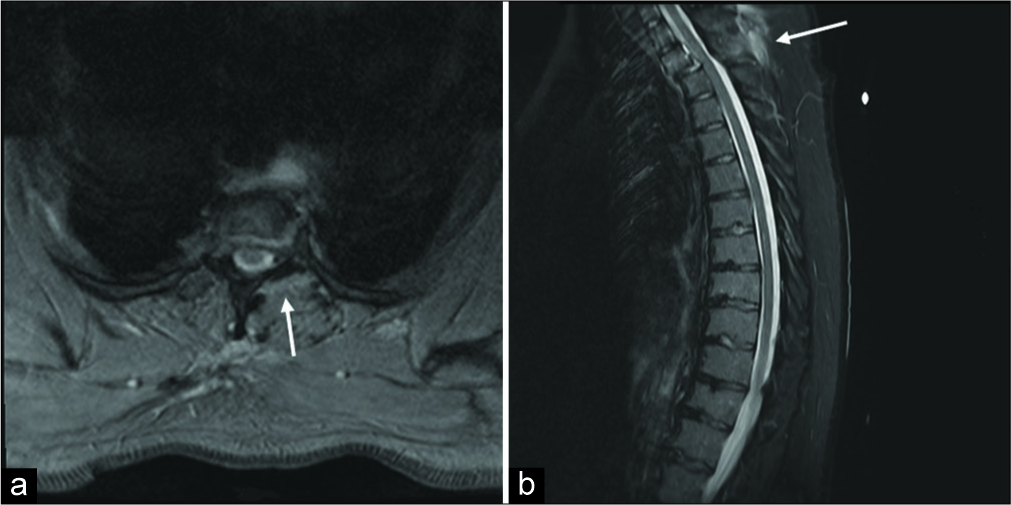
Figure 2:
Magnetic resonance imaging from time of presentation. (a) Axial T2 section image at T2-T3 level. The solid arrow shows the significant edema around the left T2-3 facet joint, the disruption of the joint capsule, and the jumped facet on the left. (b) Mid sagittal short T1 inversion recovery image, showing no cord compression. The solid arrow points out the significant disruption of the ligamentum flavum and interspinous ligament and the associated vasogenic edema.
Surgical treatment
Two days later, the patient underwent an open reduction at T2-T3 with an instrumented fusion from T1 to T5. This was performed under CT-guided navigation and neuromonitoring. Polyaxial pedicle screws were placed bilaterally from T1 to T5. The left jumped superior articular process of T3 was identified and drilled off with a matchstick high-speed electric drill, allowing for open reduction of the jumped facets. Two contoured titanium 5.5 mm rods were cut to length, put into the screw heads, and fixed with set screws and tightened. The bony surfaces were decorticated and packed with a mixture of cancellous bone chips and demineralized bone matrix allograft.
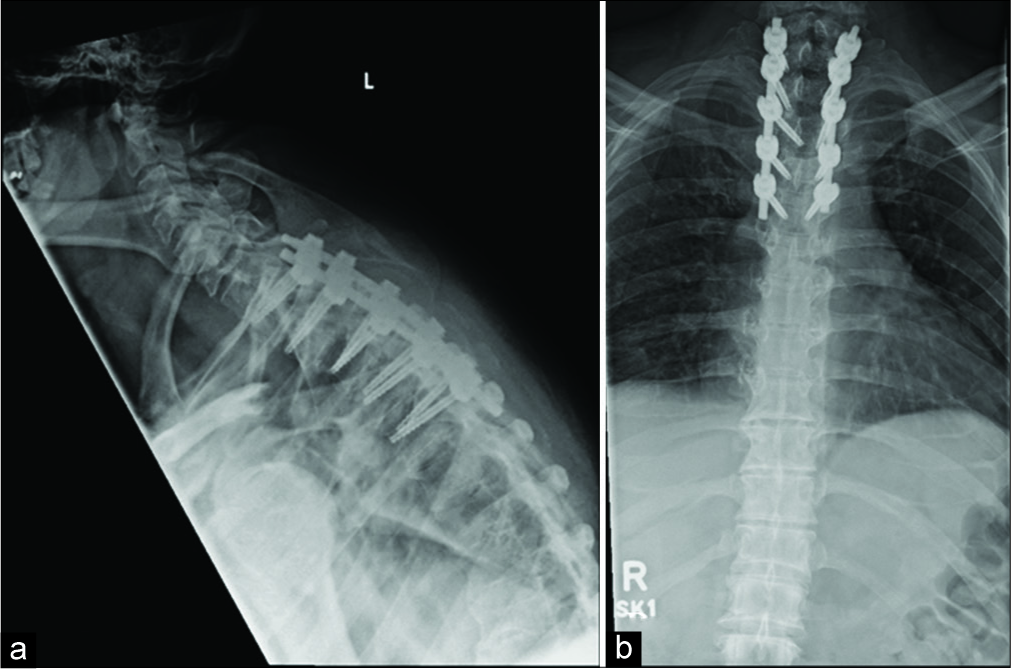
Postoperatively, the patient remained neurologically intact. X-rays taken at 3-month follow-up showed a stable construct with no significant anterolisthesis [
DISCUSSION
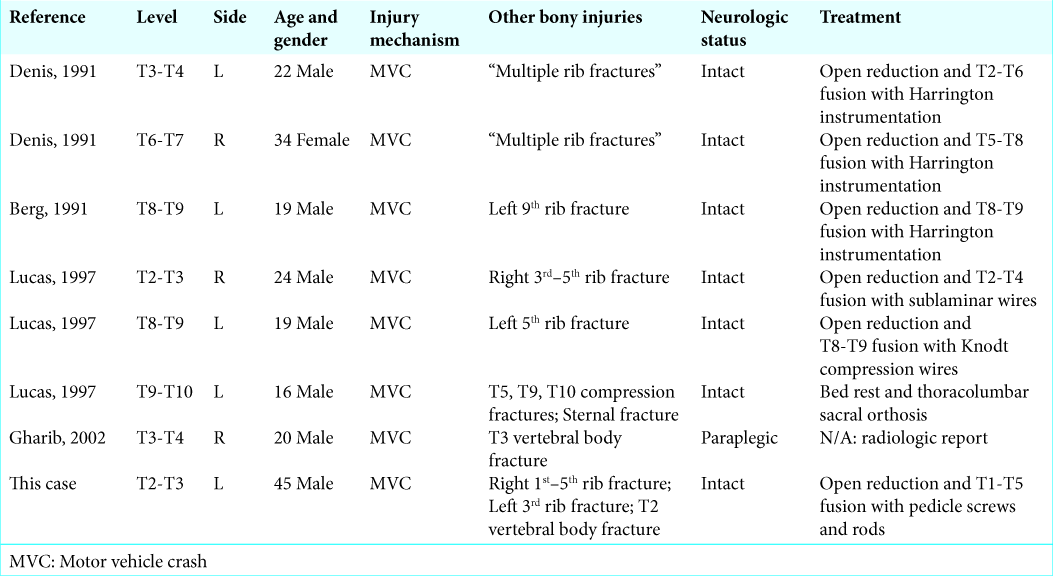
Unilateral jumped facets are much rarer than bilateral jumped facets in the thoracic spine due to the large amount of axial rotation required for the dislocated facet to rotate about the undisrupted facet joint. All but one previously reported cases of unilateral jumped thoracic facets have been associated with ipsilateral rib fracture at the same level or sternal fracture.[
Unilateral thoracic jumped facets rarely cause cord compression or neurologic symptoms due to a lack of significant listhesis. Bilateral jumped facets have a considerably higher risk of neurologic symptoms or paraplegia.[
Unilateral thoracic jumped facets should be considered unstable due to the lesions that result from the large amount of rotational force required for facet dislocation. Treatment guidelines for jumped facets in the thoracic spine involve open reduction in almost all cases. Although Lucas presents a case of a jumped left T9-T10 facet with minimal anterolisthesis that was treated nonoperatively,[
CONCLUSION
A unilateral jumped thoracic facet should be considered in patients with fractured ribs in the setting of trauma and is attributed to axial rotation. CT and MRI allow early detection of these lesions allowing for timely open reduction and instrumented fusion to optimize outcomes.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Andreshak JL, Dekutoski MB. Management of unilateral facet dislocations: A review of the literature. Orthopedics. 1997. 20: 917-26
2. Berg EE, Gilpin AT. Unilateral jumped thoracic facet dislocation. Spine (Phila Pa 1976). 1991. 16: 590-2
3. Denis F, Burkus JK. Lateral distraction injuries to the thoracic and lumbar spine. A report of three cases. J Bone Joint Surg Am. 1991. 73: 1049-53
4. Gellad FE, Levine AM, Joslyn JN, Edwards CC, Bosse M. Pure thoracolumbar facet dislocation: Clinical features and CT appearance. Radiology. 1986. 161: 505-8
5. Gharib A, Postel G, Mirza S, Mann FA. A thoracic spine translation injury with lateral facet dislocation. AJR Am J Roentgenol. 2002. 178: 1450-
6. Jaumard NV, Welch WC, Winkelstein BA. Spinal facet joint biomechanics and mechanotransduction in normal, injury and degenerative conditions. J Biomech Eng. 2011. 133: 71010-
7. Lucas MJ, Berg EE. Unilateral thoracic facet dislocation. Clin Orthop Relat Res. 1997. 335: 162-5
8. Payer M, Schmidt MH. Management of traumatic bilateral locked facets of the subaxial cervical spine. Contemp Neurosurg. 2005. 27: 1-3
9. Rorabeck CH, Rock MG, Hawkins RJ, Bourne RB. Unilateral facet dislocation of the cervical spine. An analysis of the results of treatment in 26 patients. Spine (Phila Pa 1976). 1987. 12: 23-7
10. Vaccaro AR, Oner C, Kepler CK, Dvorak M, Schnake K, Bellabarba C. AOSpine thoracolumbar spine injury classification system: Fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976). 2013. 38: 2028-37