- Institute of Neurosurgery, Catholic University School of Medicine, Rome, Italy
- Department of Neurosurgery, University of Brescia, Brescia, Italy
Correspondence Address:
Pier Paolo Mattogno
Department of Neurosurgery, University of Brescia, Brescia, Italy
DOI:10.4103/2152-7806.163317
Copyright: © 2015 Lauretti L. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Lauretti L, Mattogno PP, Bianchi F, Pallini R, Fernandez E, Doglietto F. Treatment of giant congenital cysts of the midline in adults: Report of two cases and review of the literature. Surg Neurol Int 20-Aug-2015;6:
How to cite this URL: Lauretti L, Mattogno PP, Bianchi F, Pallini R, Fernandez E, Doglietto F. Treatment of giant congenital cysts of the midline in adults: Report of two cases and review of the literature. Surg Neurol Int 20-Aug-2015;6:. Available from: http://surgicalneurologyint.com/surgicalint_articles/treatment-of-giant-congenital-cysts-of-the-midline-in-adults/
Abstract
Background:Giant cysts of the midline, not associated to a tumor, are exceptional finding in the brain of adults. Here we present two cases of symptomatic giant cerebral cysts of the midline occurred in an elderly and in a young adult patients both treated with mini-invasive unilateral neuroendoscopic procedure. In the recent literature (since 1999) similar cases have not been reported. Beside the clinical report, review of literature and major anatomical features of the region are described.
Case Description:These two adults (82 and 41 years old respectively) had a slow progressive development of headache, gait disturbances, memory impairment and urinary incontinence. Magnetic resonance imaging showed giant cyst of the midline and hydrocephalus. Surgery with the endoscopic procedure, through a right frontal burr hole, was followed by clinical and radiological improvement.
Conclusion:Giant cerebral cysts of the midline in adults can be successfully treated through a neuroendoscopic monolateral approach that comprehends multiple openings, diffuse coagulation of the capsule, and careful releasing of capsule-ependyma adherences. Knowledge of major anatomical and developmental details of the septal region is necessary to avoid complication in a mini-invasive surgical procedure.
Keywords: Cyst, midline, neuroendoscopy, septum pellucidum
INTRODUCTION
Cavum septi pellucidi (CSP), cavum vergae (CV) as well as cavum veli interpositi (CVI) are midline cerebrospinal fluid (CSF) collections that do not communicate with ventricles or subarachnoidal spaces and usually do not necessitate of any treatment. Reported as incidental findings at autopsy and during neuro-radiological exams, their incidence decreases from premature birth to adult age. When such CSF collections are larger than 1 cm, they are called “cysts” of CSP, CV, CVI. Given that there are not further classifications, in this study we reasonably considered as giant a cyst with a diameter bigger than 4 cm at least in two out of three directions (cranio-caudal, latero-lateral or antero-posterior). Symptomatic cysts cause different disorders that vary from humor changes to signs of chronic hydrocephalus as well as vomit or loss of consciousness. Shunting, craniotomy, stereotactic or endoscopic approaches have been used to treat these cysts.
Giant cysts of the midline are exceptional, especially in adults. Here we report on two cases of giant, cerebral cysts of the midline, remarkable like dimensions and age of appearance, which were treated with the endoscopic procedure. To our knowledge, these are the only two cases reported in adults since 1999.
CASE REPORT
Patients
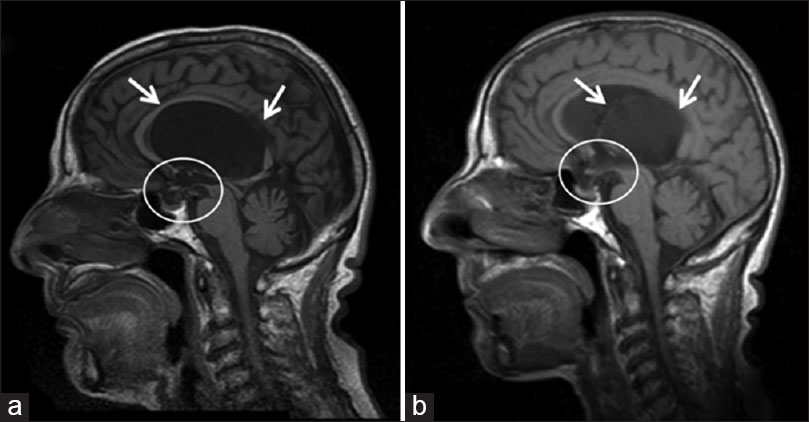
These two female patients, 82 (case 1) and 41 (case 2) years old, had a slow history of progressive short-term memory deficits and gait instability with frequent falls; urinary incontinence had lately appeared. The older patient was taking medications for arterial hypertension. In each, computed tomography (CT) scan and magnetic resonance imaging (MRI) showed a giant (diameters in the three-dimensions over 4 cm, the biggest of them over 7 cm), supratentorial cyst of the midline determining biventricular hydrocephalus: In case 1 the third ventricle and brain-stem were downward displaced [
Figure 1
Case 1. (a) Preoperative T1-weighted, sagittal plane image: The cyst (arrows) determines biventricular hydrocephalus developing over the third ventricle that is downward displaced (circle); note also the compression of both pituitary gland and its stalk (circle). (b) The postoperative corresponding magnetic resonance image shows the shrinkage of the cyst (arrows), re-expansion of the third ventricle, patency of the foramen of Monro as well as the decompression of pituitary complex (circle)
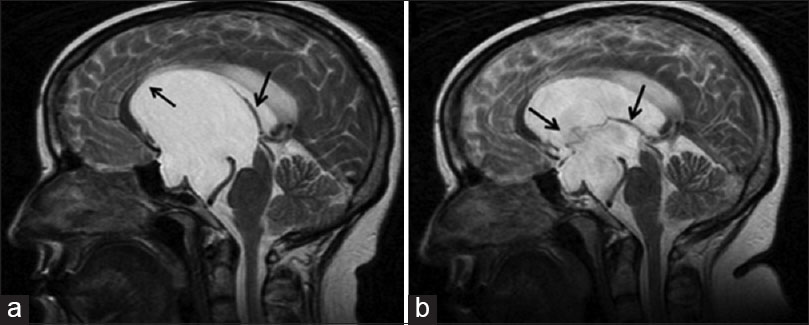
Figure 2
Case 2. (a) Preoperative magnetic resonance imaging (MRI): The sagittal plane T2-weighted image shows the enormous cyst (arrows) displacing the corpus callosum (CC) and the brain-stem. (b) The corresponding postoperative MRI: After treatment the deflated cyst wall is visible (arrows) and the CC with internal cerebral veins as well as the brain-stem appear decompressed
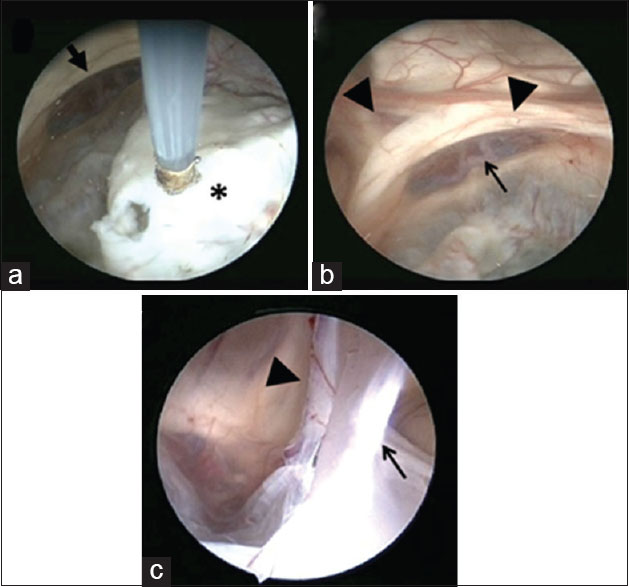
Figure 3
Endoscopic images during surgery. (a) Step by step the thick capsule (asterisk) is coagulated and fenestrated. (b and c) At the end of the procedure the cyst is clearly reduced and the surrounding anatomical structures, altered by the chronic compression, are visualized: The anterior cerebral and communicating arteries (black arrow), the absence of the septum pellucidum and the fornix of each side (bold arrows). The opened cyst wall and its adherences to the surrounding ependyma (arrows) are visible: Some of them hide dangerous veins (bold arrow)
RESULTS
The postoperative period was uneventful. The preoperative symptoms progressively improved. 12 months later they had recovered normal gait, urinary continence, and neuropsychological testing showed only minor difficulties. MRI confirmed the reduction of the cyst [Figure
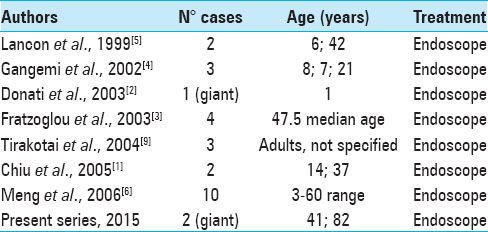
Reviewed literature has been summarized in
DISCUSSION
Cerebrospinal fluid cysts of the cerebral midline are rare and hardly ever they necessitate of any treatment. The septum region is part of the medial surface of the cerebral hemispheres, is well developed also in humans and plays an important role in pleasure and rewarding sensations. Its development is rather complex since it is made up by at least four telencephalic structures.[
The “septum pellucidum” (two layers, each one of gray and white matter), is placed between the genu of the corpus callosum (CC) anteriorly, the body of the CC dorsally, the fornix postero-ventrally, and the lateral ventricles laterally. The cavities between the layers of the “septum pellucidum,” formed during the first stages of fetal development, disappear during the first semester after birth except in 10% of the adult population with an incidence of 0.73% in the CT exams. When the anterior cavity persists, it is called “CSP.” This can be isolated but more frequently is associated to the persistence of the posterior cavity, named “CV,” which extends beyond the anterior columns of the fornix up to the splenium of CC.[
The “septum verum” contains the lateral and medial nuclei of the limbic system and is bounded anteriorly by the rostrum of the CC, ventrally by the anterior commissure and the preoptic region, and laterally by the nucleus accumbens.[
The “velum interpositum” is a double fold triangle of pia mater, enclosing subarachnoid trabeculae, between the fornix and hippocampal commissure dorsally and the ependymal roof of the third ventricle, the thalami and the superior surface of the pineal body ventrally; at each lateral margin there is a vascular fringe projecting into the choroidal fissure of the lateral ventricle. The apex of the triangle points anteriorly reaching the plane of foramina of Monro. Usually, the “velum interpositum” contains the internal cerebral veins with tributaries and the medial posterior choroidal arteries.[
The mechanisms underlying the growth of the CSF cysts of the cerebral midline are not clearly understood. Histology of the cyst wall has revealed tissue derived from “septum pellucidum” rather than arachnoid or choroid plexus.[
Common to the three different kinds of cysts are the clinical symptoms of hydrocephalus from obstruction of Monro's foramina or Silvius's acqueduct. Then, headache, gait disturbances, urinary incontinence, cognitive deterioration, vomiting and loss of consciousness are the symptoms. The anterior cysts can also compress optic and fronto-temporal structures causing visual disturbances, neuropsychiatric disorders, and memory deficit. Sometimes, because of the slow growth, large cysts can be asymptomatic and can be found incidentally.
Currently, the treatment of choice of symptomatic CSP, CV, CVI cysts is endoscopic fenestration through frontal or, seldom, posterior approach. Other options, mostly used formerly, include craniotomy, shunting, and stereotactic drainage.
Reviewing the 25 symptomatic midline cysts operated on and reported since 1999 [
Regarding surgery, endoscopic treatment with flexible as well as rigid endoscope has been widely described, as well as different surgical approaches: Anterior (frontal) monolateral or bilateral, posterior (carrefour).[
During surgery, in both cases we used a monolateral, right frontal approach (precoronaric burr hole, 2 cm from the midline) and a rigid Storz-Decq endoscope: The cyst was reached at the depth of 3–4 cm and the capsule appeared white, tense, sulked by small vessels. Multiple openings were made by monopolar coagulation [
CONCLUSION
Giant cysts of CSP, CV and CVI in adults can be successfully treated through a monolateral endoscopic approach. Bilateral ventriculostomy is not required and adds an unnecessary risk of bifrontal damage. Differently from the newborn, to obtain an evident reduction of the cyst, multiple openings and diffuse coagulation of the capsule as well as a careful releasing of capsule-ependyma adherences can determine a better and lasting cure.
ACKNOWLEDGMENTS
Daniele Petricca (technical support for images).
References
1. Chiu CD, Huang WC, Huang MC, Wang SJ, Shih YH, Lee LS. Navigator system-assisted endoscopic fenestration of a symptomatic cyst in the septum pellucidum – Technique and cases report. Clin Neurol Neurosurg. 2005. 45: 105-8
2. Donati P, Sardo L, Sanzo M. Giant cyst of the cavum septi pellucidi, cavum vergae and veli interpositi. Minim Invasive Neurosurg. 2003. 46: 177-81
3. Fratzoglou M, Grunert P, Leite dos Santos A, Hwang P, Fries G. Symptomatic cysts of the cavum septi pellucidi and cavum vergae: The role of endoscopic neurosurgery in the treatment of four consecutive cases. Minim Invasive Neurosurg. 2003. 46: 243-9
4. Gangemi M, Maiuri F, Cappabianca P, Alafaci C, de Divitiis O, Tomasello F. Endoscopic fenestration of symptomatic septum pellucidum cysts: Three case reports with discussion on the approaches and technique. Minim Invasive Neurosurg. 2002. 107: 337-41
5. Lancon JA, Haines DE, Lewis AI, Parent AD. Endoscopic treatment of symptomatic septum pellucidum cysts: With some preliminary observations on the ultrastructure of the cyst wall: Two technical case reports. Neurosurgery. 1999. 45: 1251-7
6. Meng H, Feng H, Le F, Lu JY. Neuroendoscopic management of symptomatic septum pellucidum cysts. Neurosurgery. 2006. 59: 278-83
7. Nieuwenhuys R, Voogd J, van Huijzen C.editors. The Human Central Nervous System. Berlin/Heidelberg/New York: Springer-Verlag; 2007. p.
8. Nishijima Y, Fujimura M, Nagamatsu K, Kohama M, Tominaga T. Neuroendoscopic management of symptomatic septum pellucidum cavum vergae cyst using a high-definition flexible endoscopic system. Case report. Neurol Med Chir (Tokyo). 2009. 49: 549-52
9. Tirakotai W, Schulte DM, Bauer BL, Bertalanffy H, Hellwig D. Neuroendoscopic surgery of intracranial cysts in adults. Childs Nerv Syst. 2004. 20: 842-51






Nic
Posted February 20, 2019, 3:27 am
In 2013 I had a CT scan to investigate headaches. The CT report mentioned enlargement of the left lateral ventricle with bulging of the septum pellucidum towards the right side. Possible cyst. It is now 2019 and I did not have any further tests. I have frequent memory loss, headaches and dizziness. I am 52 years old and otherwise healthy. Should I look into surgery? Thank you.