- Department of Neurosurgery, Kansai Medical University, Hirakata, Osaka, Japan.
Correspondence Address:
Masahiro Nonaka, Department of Neurosurgery, Kansai Medical University, Hirakata, Osaka, Japan.
DOI:10.25259/SNI_99_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Nobuaki Naito, Masahiro Nonaka, Mayuko Miyata, Katsuya Ueno, Takamasa Kamei, Akio Asai. Treatment of refractory giant suprasellar arachnoid cyst by endoscopic expansion of a fenestrated stoma. 31-Mar-2022;13:112
How to cite this URL: Nobuaki Naito, Masahiro Nonaka, Mayuko Miyata, Katsuya Ueno, Takamasa Kamei, Akio Asai. Treatment of refractory giant suprasellar arachnoid cyst by endoscopic expansion of a fenestrated stoma. 31-Mar-2022;13:112. Available from: https://surgicalneurologyint.com/surgicalint-articles/11505/
Abstract
Background: Although endoscopic ventriculo-cysto-cisternostomy is considered to be effective for suprasellar arachnoid cysts, we encountered a giant suprasellar arachnoid cyst that recurred despite surgery using this technique.
Case Description: The patient was a 9-month-old boy. Magnetic resonance imaging revealed a huge suprasellar arachnoid cyst extending from the suprasellar region to the anterior skull base and both middle cranial fossa. First, an endoscopic procedure was performed to open the cyst wall between the right ventricle and the cyst and between the cyst and the prepontine cistern. Although the cyst initially shrank, it recurred over the next 2 months, and hence, we performed another endoscopic surgery. At the second surgery, both the previously opened stomas were found to be occluded. To reopen the cyst wall between the ventricle and the cyst, multiple holes were made with monopolar electrodes, and forceps were used to connect the holes by grasping and twisting the cyst wall so that the stoma was much larger than at the previous surgery. Postoperatively, the cyst shrank and the patient’s head circumference stopped expanding.
Conclusion: Following the treatment of large cysts, the stoma might become narrower as the cyst shrinks, resulting in obstruction. Using the technique reported here might prevent occlusion of large arachnoid cysts.
Keywords: Endoscopic fenestration, Flexible endoscope, Suprasellar arachnoid cyst
INTRODUCTION
The accepted treatment for suprasellar arachnoid cysts is creation of a window using an endoscope, while ventriculo-cysto-cisternostomy (VCC) in the arachnoid cyst[
CASE REPORT
The patient was a 9-month-old boy born by normal delivery at 38 weeks.
At the 4-month checkup, his head circumference was large for age and his neck was not yet fixed.
At 5 months, his head circumference had enlarged to 46.9 cm and he was unable to raise his head in the prone position and did not show grasping movements.
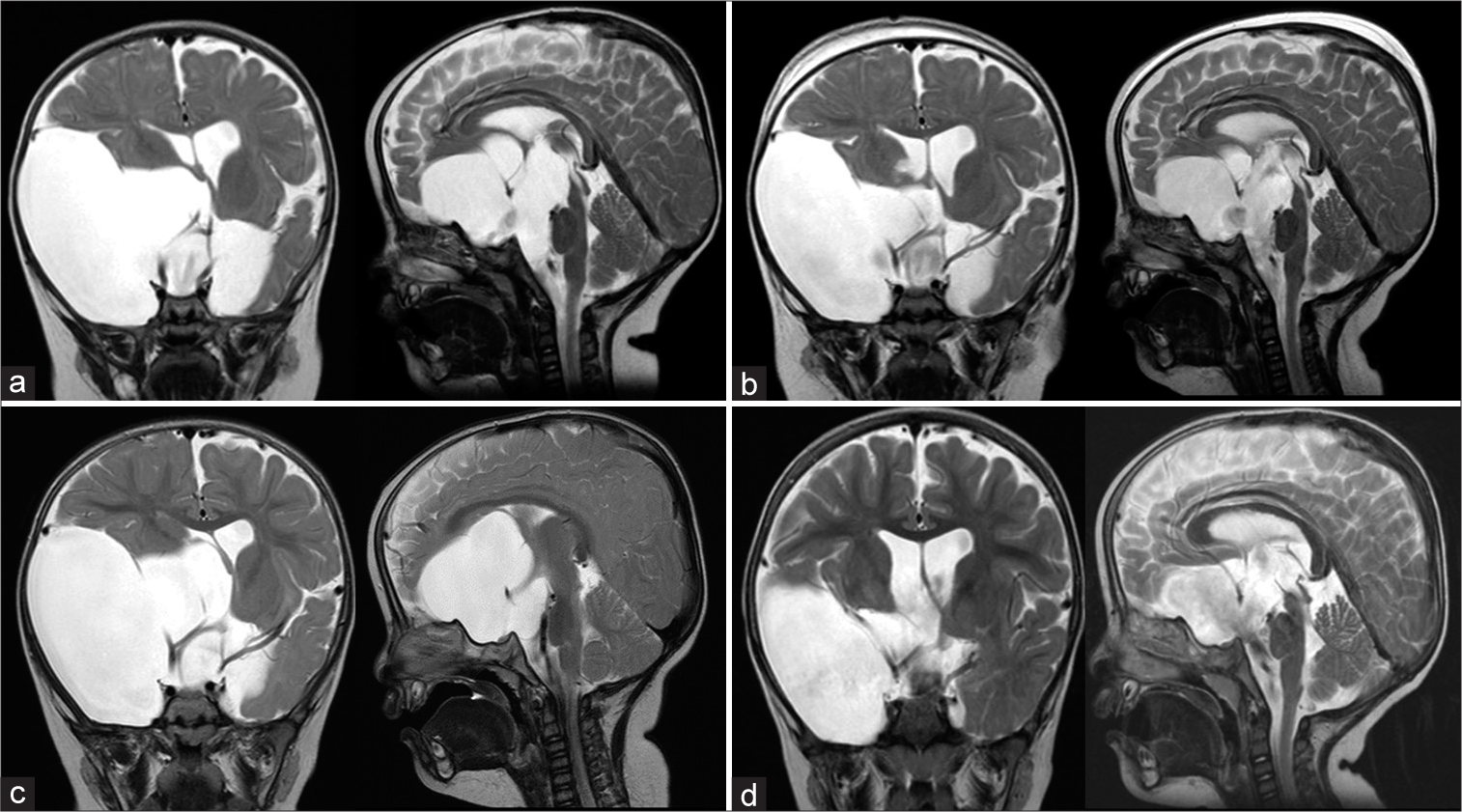
Magnetic resonance imaging (MRI) of the head showed a huge arachnoid cyst extending from the suprasellar region to the anterior skull base and middle cranial fossa bilaterally [
Surgical findings (at the first surgery)
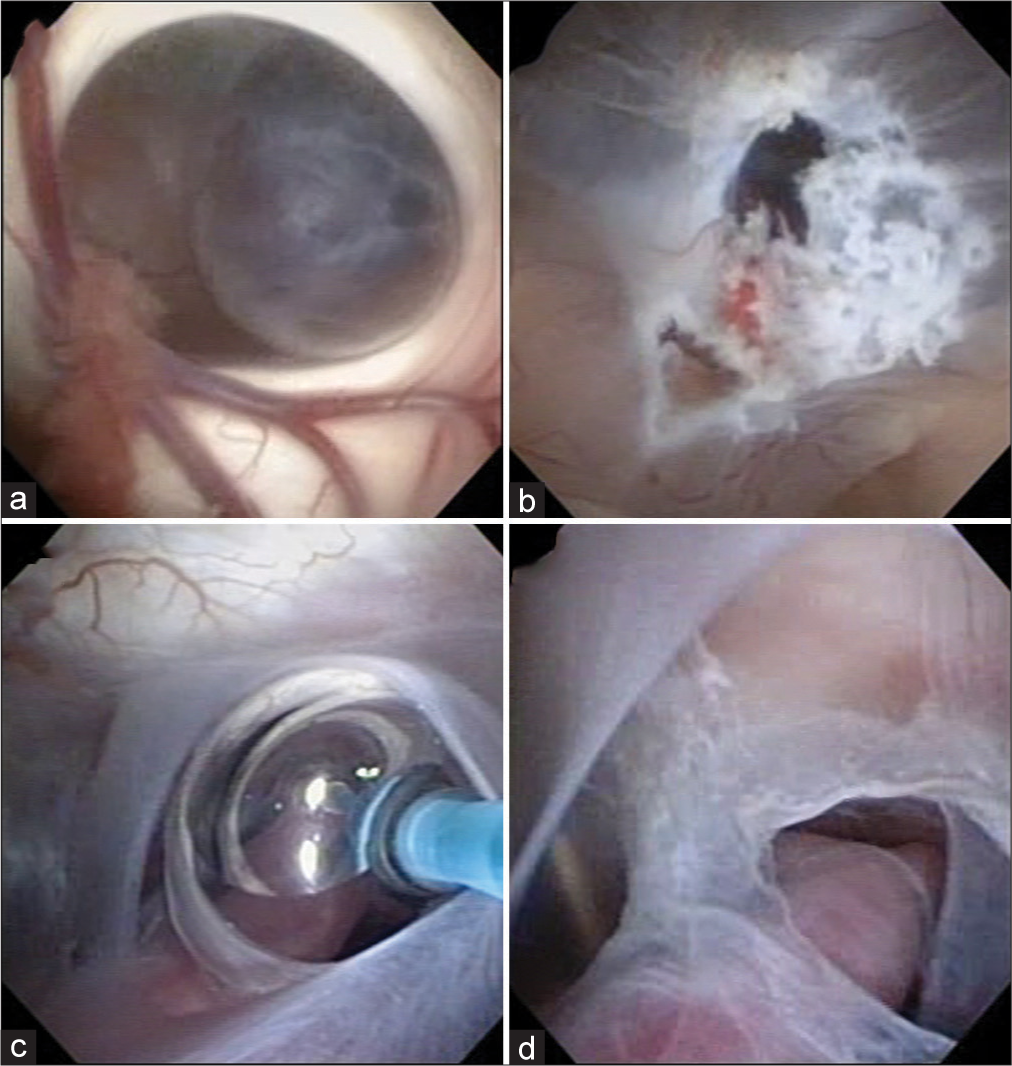
A flexible endoscope (Olympus VEF-V) was inserted through the right anterior horn of the lateral ventricle, and the cyst wall was seen through the foramen of Monro [
Figure 3:
Intraoperative endoscopic findings during the first surgery. (a) The cyst wall was seen through the foramen of Monro. (b) Cauterization and perforation of the cyst wall was performed using a monopolar electrode (RAF electrode, Aims Co., Japan). (c) A balloon catheter was used to expand the stoma. (d) Fenestration between the cyst and the prepontine cistern.
Postoperative course
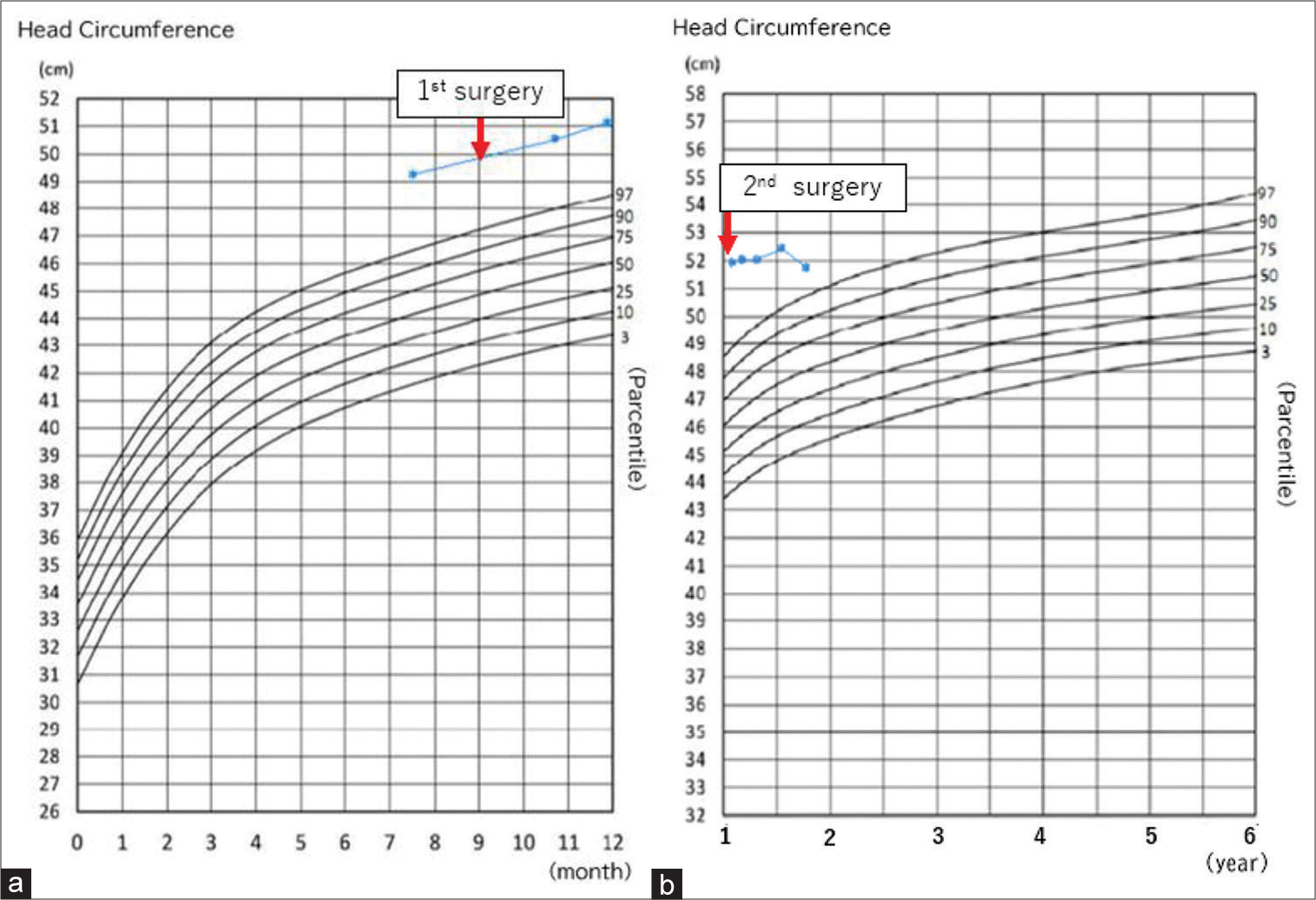
Postoperative MRI 2 days after the surgery showed reduction in the size of the cyst, and the patient was discharged without complications. The patient was subsequently monitored on an outpatient basis. However, 2 months later, at the age of 11 months, MRI again showed enlargement of the arachnoid cyst, leading to the suspicion of obstruction of the stoma.
Surgical findings (at the second surgery)
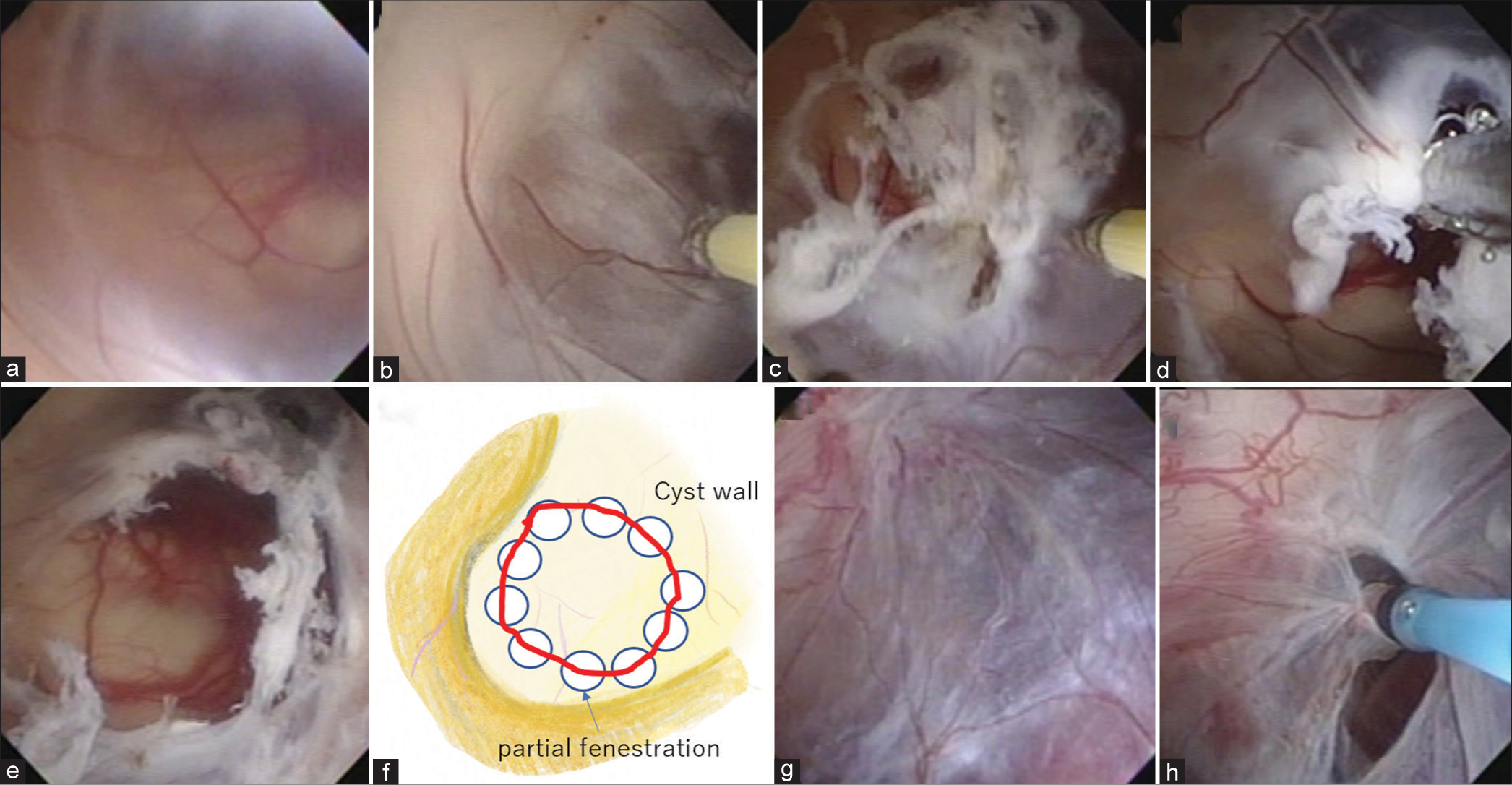
As in the first surgery, a flexible endoscope (Olympus VEF-V) was introduced into the right anterior horn of the lateral ventricle. The cyst wall was seen through the foramen of Monro and the previous stoma was seen to be occluded [
Figure 4:
Intraoperative endoscopic findings during the second surgery. (a) Obstructed cyst wall. (b: Cauterization and perforation of the cyst wall. (c) Multiple perforations were performed. (d and e) The cyst wall was grasped by biopsy forceps and the hole was enlarged. (f) Schema of cyst wall fenestration enlargement. (g) Reocclusion of the space between the cyst and the prepontine cistern. (h) Enlargement of the stoma to the prepontine cistern using a balloon catheter.
Postoperative course
MRI performed immediately after the surgery showed reduction in the size of the cyst. MRI at 3 months and 8 months after the second surgery showed diminution of the cyst over time. Developmentally, the child was able to walk unaided at the age of 1 year and 6 months and babbling increased at 1 year and 9 months. His head circumference was approximately within the normal range.
IRB/ethics committee approval
This study has been approved by the Ethical Review Committee of Kansai Medical University (No. 2019302).
DISCUSSION
We described here a congenital giant suprasellar arachnoid cyst extending to the anterior skull base and middle cranial fossa, which was discovered due to an enlarged head circumference and developmental delay. Endoscopic cyst fenestration was performed, although the patient required a second endoscopic surgery due to cyst recurrence. Suprasellar arachnoid cysts account for about 5–12% of intracranial arachnoid cysts[
Although shunt insertion can be effective, there is a risk of postoperative infection and shunt malfunction. When an arachnoid cyst is shunted, the cyst shrinks or disappears, and the cerebrospinal fluid (CSF) that flows into the cyst flows out through the shunt. If the shunt malfunctions, however, the diagnosis is delayed because the cyst does not increase in size and only intracranial pressure rises, and shunt reconstruction is difficult in this situation because there is no place to insert the proximal catheter.[
Endoscopic fenestration was associated with the fewest complications in the previous reports, although the anatomical location of the blood vessels and cranial nerves in the cistern must be understood when fenestrating the wall between the cyst and the cistern.[
In this case, although VCC was performed as the initial treatment, the cyst recurred. We hypothesized that as the cyst shrank, the cyst walls began to overlap, resulting in stomal adhesion and obstruction.
Various methods have been reported for the prevention of stomal occlusion, including cauterization of the cyst itself to reduce its size[
The patient did well after the second surgery, and no untoward effects were observed at the 1-year follow-up. Although there is no fixed opinion on the size of the window for endoscopic fenestration of the arachnoid cyst wall, our experience suggests that in cases with a very large cyst, the hole should be made as large as possible because the cyst wall might overlap and cause stomal occlusion as it shrinks.
CONCLUSION
In this case, we first performed VCC and coagulation of the cyst wall for a huge arachnoid cyst extending from the suprasellar region to the anterior and middle cranial fossa, although the cyst re-expanded due to obstruction of the stomas. By creating another larger fenestration, good stomal patency and smooth drainage of CSF were obtained.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Grant-in-Aid from the Research Committee of CNS Degenerative Diseases, Research on Policy Planning and Evaluation for Rare and Intractable Diseases, Health, Labour and Welfare Sciences Research Grants, The Ministry of Health, Labour, and Welfare, Japan (20FC1049).
Conflicts of interest
There are no conflicts of interest.
References
1. Caemaert J, Abdullah J, Calliauw L, Carton D, Dhooge C, van Coster R. Endoscopic treatment of suprasellar arachnoid cysts. Acta Neurochir (Wien). 1992. 119: 68-73
2. Chen Y, Fang HJ, Li ZF, Yu SY, Li CZ, Wu ZB. Treatment of middle cranial fossa arachnoid cysts: A systematic review and meta-analysis. World Neurosurg. 2016. 92: 480-90.e482
3. Crimmins DW, Pierre-Kahn A, Sainte-Rose C, Zerah M. Treatment of suprasellar cysts and patient outcome. J Neurosurg. 2006. 105: 107-14
4. El-Ghandour NM. Endoscopic treatment of suprasellar arachnoid cysts in children. J Neurosurg Pediatr. 2011. 8: 6-14
5. Fewel ME, Levy ML, McComb JG. Surgical treatment of 95 children with 102 intracranial arachnoid cysts. Pediatr Neurosurg. 1996. 25: 165-73
6. Fujio S, Bunyamin J, Hirano H, Oyoshi T, Sadamura Y, Bohara M. A novel bilateral approach for suprasellar arachnoid cysts: A case report. Pediatr Neurosurg. 2016. 51: 30-4
7. Gangemi M, Colella G, Magro F, Maiuri F. Suprasellar arachnoid cysts: Endoscopy versus microsurgical cyst excision and shunting. Br J Neurosurg. 2007. 21: 276-80
8. Gangemi M, Seneca V, Colella G, Cioffi V, Imperato A, Maiuri F. Endoscopy versus microsurgical cyst excision and shunting for treating intracranial arachnoid cysts. J Neurosurg Pediatr. 2011. 8: 158-64
9. Gosalakkal JA. Intracranial arachnoid cysts in children: A review of pathogenesis, clinical features, and management. Pediatr Neurol. 2002. 26: 93-8
10. Laviv Y, Michowitz S. Acute intracranial hypertension and shunt dependency following treatment of intracranial arachnoid cyst in a child: A case report and review of the literature. Acta Neurochir (Wien). 2010. 152: 1419-23
11. Maher CO, Goumnerova L. The effectiveness of ventriculocystocisternostomy for suprasellar arachnoid cysts. J Neurosurg Pediatr. 2011. 7: 64-72
12. Sood S, Schuhmann MU, Cakan N, Ham SD. Endoscopic fenestration and coagulation shrinkage of suprasellar arachnoid cysts. Technical note. J Neurosurg. 2005. 102: 127-33
13. Wang JC, Heier L, Souweidane MM. Advances in the endoscopic management of suprasellar arachnoid cysts in children. J Neurosurg. 2004. 100: 418-26