- Department of Medical Technology Center, Nara Medical University, Kashihara, Japan.
- Department of Neurosurgery, Nara Medical University, Kashihara, Japan.
- Department of Respiratory Medicine, Nara Medical University, Kashihara, Japan.
- Department of Rehabilitation Medicine, Nara Medical University, Kashihara, Japan.
Correspondence Address:
Ryosuke Matsuda, MD,PhD, Department of Neurosurgery, Nara Medical University, Shijo-cho, Kashihara, Nara, Japan.
DOI:10.25259/SNI_500_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shigeto Soyama1, Ryosuke Matsuda2, Shigeto Hontsu3, Satsuki Ando1, Saori Tatsumi1, Tetsuro Kitamura1, Ichiro Nakagawa2, Akira Kido4, Hiroyuki Nakase2. Treatment of transient prosopagnosia with a tyrosine kinase inhibitor in a case of brain metastasis from EGFR-mutated lung adenocarcinoma. 01-Jul-2022;13:280
How to cite this URL: Shigeto Soyama1, Ryosuke Matsuda2, Shigeto Hontsu3, Satsuki Ando1, Saori Tatsumi1, Tetsuro Kitamura1, Ichiro Nakagawa2, Akira Kido4, Hiroyuki Nakase2. Treatment of transient prosopagnosia with a tyrosine kinase inhibitor in a case of brain metastasis from EGFR-mutated lung adenocarcinoma. 01-Jul-2022;13:280. Available from: https://surgicalneurologyint.com/surgicalint-articles/11690/
Abstract
Background: Prosopagnosia is a rare form of apraxia, in which a person has normal memory and vision, but has impaired cognition of human faces that are manifested through symptoms such as not being able to recognize the face of a familiar person, one has known or not being able to remember the face of a person. Here, we report the case of a patient with transient prosopagnosia associated with brain metastasis from epidermal growth factor receptor (EGFR)-mutated lung adenocarcinoma who was treated with tyrosine kinase inhibitors (TKIs).
Case Description: A 52-year-old right-handed man with lung adenocarcinoma was introduced to our department because brain metastasis. On admission, he complained that he could not recognize his wife’s face, but he could recall her face based on her voice. MRI revealed a right temporo-occipital enhancing lesion with perifocal edema and dissemination that were indicative of brain metastasis from lung adenocarcinoma. Two weeks after open biopsy, he was started on TKI therapy with osimertinib at a dosage of 80 mg/day. An MRI scan taken 1 month later revealed shrinkage of the metastasis. In addition, he had recovered from transient prosopagnosia and returned to normal life.
Conclusion: In this study, the TKI osimertinib was administered to a patient with brain metastasis of EGFR-mutated lung adenocarcinoma who presented with prosopagnosia, and the patient’s lesion shrunk and his symptoms were reversed with this treatment.
Keywords: Brain metastasis, Lung adenocarcinoma, Prosopagnosia, Tyrosine kinase inhibitor
INTRODUCTION
Prosopagnosia is a neurocognitive disorder that selectively disrupts facial recognition caused by brain injury.[
With regard to brain tumors, lesions in the right lingual and fusiform gyrus are generally considered to be responsible for prosopagnosia.[
For lung adenocarcinoma with epidermal growth factor receptor (EGFR) mutation, tyrosine kinase inhibitors (TKIs) have become the first-line drugs of choice. In particular, TKIs are expected to be effective in cases with metastatic brain tumors, because they have good CSF transferability, unlike other anticancer agents.[
CASE REPORT
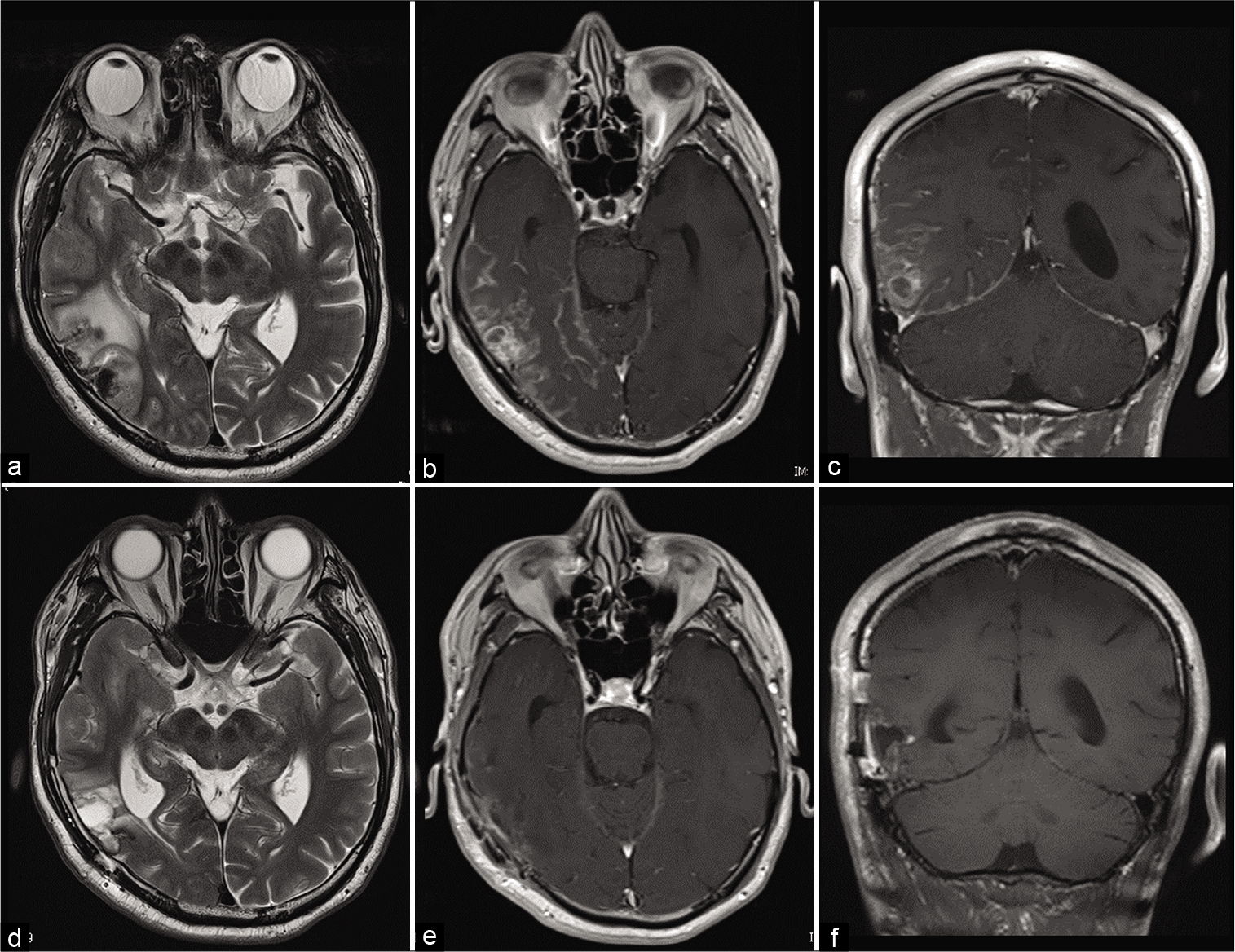
A 52-year-old right-handed man was introduced to our department, because he had presented at a local clinic with headache and was diagnosed with brain tumor based on magnetic resonance imaging (MRI) findings. Two years before the visit, the patient had been diagnosed with lung adenocarcinoma (stage pT1cN0M0), but MRI of the brain taken at that time did not show any brain metastases. The patient underwent video-assisted thoracoscopic surgery (VATS) for the lung adenocarcinoma at another hospital and was subsequently administered chemotherapy with uracil/tegafur at a dosage of 400 mg/day. After VATS, computed topography indicated that the lung cancer had not recurred for 2 years after the procedure. MRI taken at our department revealed a right temporo-occipital enhancing lesion with perifocal edema and dissemination that was indicative of brain metastasis [
Figure 1:
MRI findings indicative of brain metastasis. Pretreatment MRI T2-weighted image showing brain metastasis with perifocal edema in the right inferior temporal gyrus. (a) Preoperative enhanced MRI image showing brain metastasis with dissemination. (b and c) Posttreatment MRI showing shrinkage of the brain metastasis after the administration of the TKI osimertinib. (d: T2-weighted scans, e and f: enhanced MRI scan).
On admission to our department, the patient complained that he could not recognize his wife’s face, but he could recall her face based on her voice. The preoperative mini-mental statement examination score was 30/30; IQ was 118 according to Kohs block-design test; and verbal IQ was 147 according to Wechsler Adult Intelligence Scale-III. These results did not indicate cognitive decline. On the Visual Perception Test for Agnosia, he was able to distinguish facial expression, age, sex, and gender, but had difficulty in recognizing and identifying unknown facial features. Further, he scored 44% on the Cambridge Face Memory Test at the time of admission.
The pathological diagnosis in the present case was EGFR-mutated adenocarcinoma. Two weeks after open biopsy, he was started on TKI therapy with osimertinib at a dosage of 80 mg/day. An MRI scan taken 1 month later revealed shrinkage of the metastasis. In addition, he had recovered from transient prosopagnosia and returned to normal life. His score for the Cambridge Face Memory Test conducted 1 month later after the start of osimertinib treatment improved to 75%. There has been no tumor recurrence after administration of osimertinib for 12 months [
DISCUSSION
There has been a long history of debate on the responsible foci for face recognition, and functional brain imaging studies have revealed the importance of the right lingual and fusiform gyrus in face recognition.[
Lang et al. reported a case of prosopagnosia caused by infarction of the right fusiform gyrus that gradually improved over the course of 1 month.[
CONCLUSION
In this study, the TKI osimertinib was administered to a patient with cerebral metastasis of EGFR-mutated lung adenocarcinoma who presented with prosopagnosia, and the patient’s lesion shrunk and his symptoms were reversed with this treatment. Thus, appropriate treatment of the causative factor of prosopagnosia can reverse the symptoms.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Anderson CA, Woodcock JH, Filley CM. Transient prosopagnosia with right temporal astrocytoma. J Neuropsychiatry Clin Neurosci. 2016. 28: e13-4
2. Corrivetti F, Herbet G, Moritz-Gasser S, Duffau H. Prosopagnosia induced by a left anterior temporal lobectomy following a right temporo-occipital resection in a multicentric diffuse low-grade glioma. World Neurosurg. 2017. 97: 756.e1-5
3. Corrow SL, Dalrymple KA, Barton JJ. Prosopagnosia: Current perspectives. Eye Brain. 2016. 8: 165-75
4. Das S, Burton E. Pearls and Oy-sters: Isolated prosopagnosia as the presenting complaint in glioblastoma: The face of deception. Neurology. 2019. 93: 642-4
5. Genova HM, Rajagopalan V, Chiaravalloti N, Binder A, Deluca J, Lengenfelder J. Facial affect recognition linked to damage in specific white matter tracts in traumatic brain injury. Soc Neurosci. 2015. 10: 27-34
6. Hashimoto R, Tagawa A, Komori N, Ogawa T, Kato H. Transient dyschromatopsia, static form agnosia, and prosopagnosia observed in a patient with Anti-NMDA receptor encephalitis. Case Rep Neurol Med. 2019. 2019: 2929782
7. Hosokawa H, Kanno S, Nishio Y, Kawasaki I, Hirayama K, Sunaga A. Facial memory ability and self-awareness in patients with temporal lobe epilepsy after anterior temporal lobectomy. PLoS One. 2021. 16: e0248785
8. Kanwisher N, McDermott J, Chun MM. The fusiform face area: A module in human extrastriate cortex specialized for face perception. J Neurosci. 1997. 17: 4302-11
9. Lang N, Baudewig J, Kallenberg K, Antal A, Happe S, Dechent P. Transient prosopagnosia after ischemic stroke. Neurology. 2006. 66: 916
10. Watanabe K, Yoh K, Hosomi Y, Usui K, Naka G, Kishi K. Efficacy and safety of first-line osimertinib treatment and postprogression patterns of care in patients with epidermal growth factor receptor activating mutation-positive advanced non-small cell lung cancer (Reiwa study): Study protocol of a multicentre, real-world observational study. BMJ Open. 2022. 12: e046451
11. Yuan Y, Huang F, Gao ZH, Cai WC, Xiao JX, Yang YE. Delayed diagnosis of prosopagnosia following a hemorrhagic stroke in an elderly man: A case report. World J Clin Cases. 2020. 8: 6487-98






Dr. Miguel A. Faria
Posted July 5, 2022, 5:10 am
This is very interesting case! As the authors write, “These findings indicate that the right lingual and fusiform gyrus were transiently affected [with prosopagnosia] by the brain metastasis, but not permanently damaged and the condition was reversible.”