- Department of Neurology, Baylor College of Medicine, Houston, Texas, United States.
- Department of Neurosurgery, Baylor College of Medicine, Houston, Texas, United States.
Correspondence Address:
Zulfi Haneef, Department of Neurology, Baylor College of Medicine, Houston, Texas, United States.
DOI:10.25259/SNI_692_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Zulfi Haneef1, Alexandr Karimov1, Vaishnav Krishnan1, Sameer A. Sheth2. Trigeminal paresthesia secondary to responsive neurostimulation (RNS) lead migration. 23-Nov-2021;12:577
How to cite this URL: Zulfi Haneef1, Alexandr Karimov1, Vaishnav Krishnan1, Sameer A. Sheth2. Trigeminal paresthesia secondary to responsive neurostimulation (RNS) lead migration. 23-Nov-2021;12:577. Available from: https://surgicalneurologyint.com/surgicalint-articles/11238/
Abstract
Background: The responsive neurostimulation system (RNS) is used in patients with drug-resistant epilepsy who are not candidates for surgical resection of a seizure focus. As a relatively new therapy option, the adverse effects of long-term implantation are still being clarified. We present a series of two patients who presented with similar symptoms which were attributable to migration of the intracranially implanted subdural leads.
Case Description: Two patients who had subdural RNS lead implantation presented with symptoms of paroxysmal unilateral facial pain which were thought to be related to the stimulation of the trigeminal nerve secondary to RNS lead migration. Adjustment of the stimulation parameters improved the symptoms in both patients.
Conclusion: Chronically implanted subdural RNS leads can migrate over time stimulating nerves in the intracranial space. Strategies to avoid and overcome the complication are discussed.
Keywords: Lead migration, Responsive neuro-stimulation, Stimulation triggered symptoms, Trigeminal nerve
INTRODUCTION
The Responsive Neurostimulation (RNS) system (Neuropace RNS® System, Mountain View, CA, USA) is a therapy for patients with drug-resistant epilepsy who are not candidates for surgical resection of a seizure focus.[
CASE REPORT
We present two patients with symptoms of paroxysmal facial sensation ipsilateral to subtemporal RNS strip leads months after uneventful implantation. The patients did not report any sensory symptoms in the immediate post-implant period; however, they both presented independently complaining of episodes of unilateral facial sensation months later. In both patients, the symptoms developed relatively rapidly over a few weeks. Patient 1 is a 39-year-old male who developed a shock-like sensation in the right lower part of the face nearly 1.5 years after implantation.
Patient 2 is a 33-year-old male who reported tingling in the right upper part of the face approximately 9 months after implantation.
We did not appreciate any objective facial sensory abnormalities on examination in either patient. The explanation of the new symptom was not apparent initially, as the trigeminal nerve and its branches that provide facial sensation are rarely injured during this type of procedure. Furthermore, the paroxysmal nature of the reported symptoms raised the suspicion that they were related to stimulation delivery. Around the time of symptom onset, we measured impedance from the RNS contacts, and it appeared to be increased in the subtemporal leads. Impedance measurements in the other leads (hippocampal) were not altered. As lead impedance can be elevated with loss of contact with the underlying brain, we hypothesized that migration of the subtemporal RNS strips toward the intracranial portion of the trigeminal nerve might be responsible for the patients’ symptoms by electrical stimulation of the nerve. There was no apparent involvement of the jaw musculature or facial muscles to suggest trigeminal motor or facial involvement.
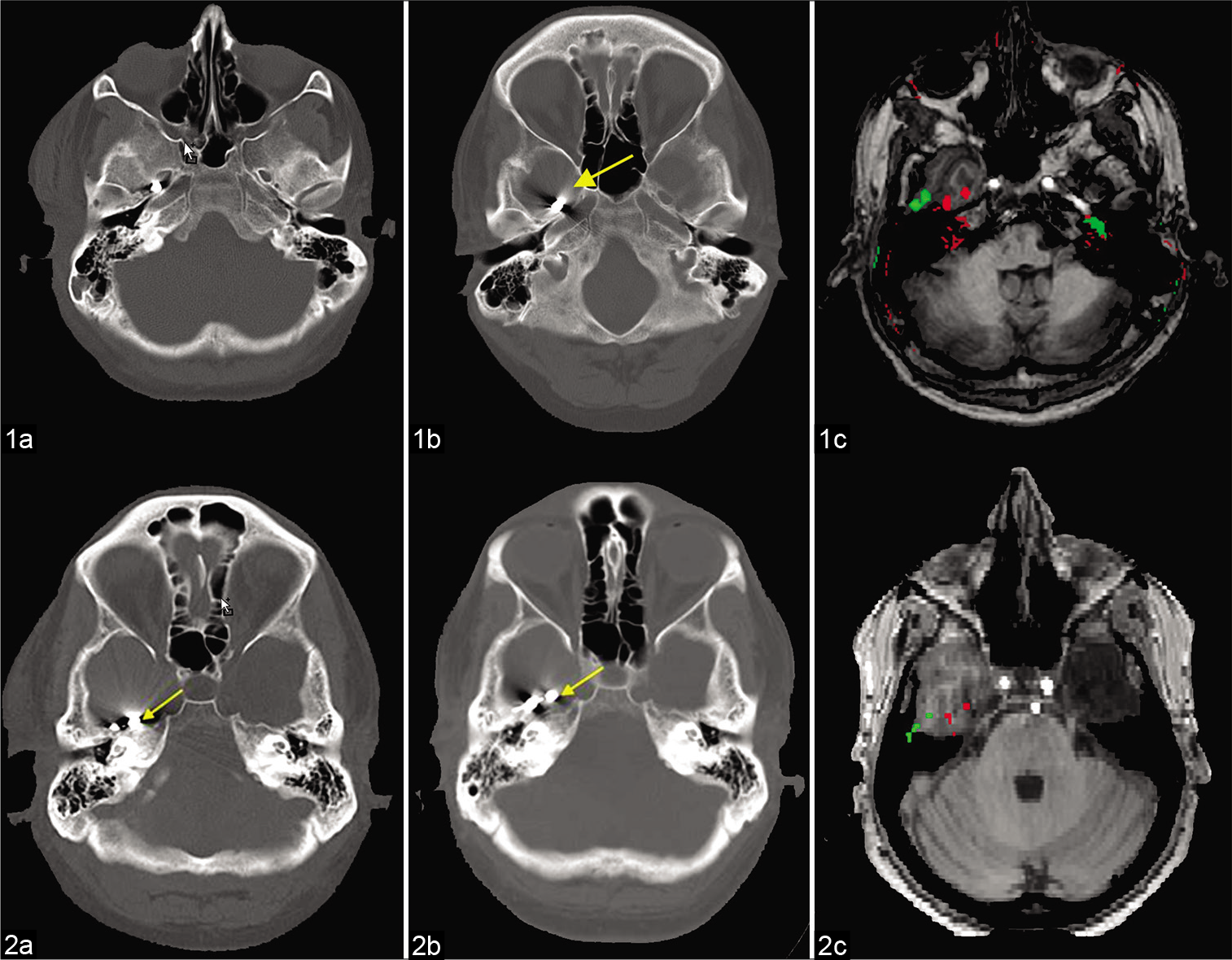
Stimulation at the same current as the stimulation current reproduced the symptoms in the patients. Turning off the subtemporal strip caused resolution of the symptoms. We analyzed medical records and neuroimaging of the two patients. Structural brain magnetic resonance images (MRI) were co-registered with computed tomography (CT) scans to compare RNS lead locations between the immediate post-implant period and the time of symptomatic presentation. Imaging analysis of co-registered MRI-CT scans revealed anterior migration of the RNS lead tip in both cases [
Figure 1:
Images for patients 1 and 2 show the sub-temporal lead adjacent to the bone immediately after implantation (1a, 2a); repeat images reveal displacement of the same lead over time (1b, 2b). Images 1c and 2c show the relative position of the lead at implantation (red) and at presentation (green).
DISCUSSION
We describe a unique long-term complication of RNS subdural strip implantation in the sub-temporal location. Migration of the lead can lead to stimulation of the trigeminal nerve/branches, potentially causing paroxysmal ipsilateral facial sensations or pain. Another potential explanation of the sensory symptoms can be nerve injury during lead implantation, for example, due to direct and indirect trauma related to retraction, cautery, and suction. Although uncommon, trigeminal neuropathic pain has been reported as a complication of anterior temporal lobe resection.[
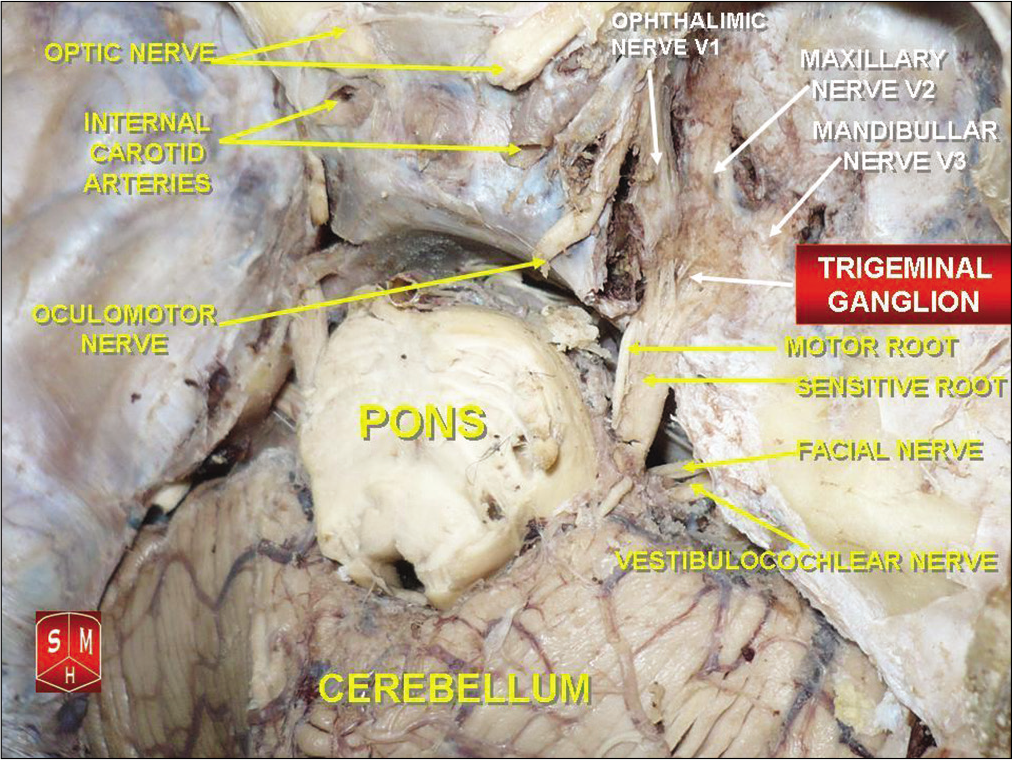
Figure 2:
Representative image showing the anatomy of the middle cranial fossa and brainstem with relations between the petrous ridge, trigeminal ganglion, mandibular nerve (V3) at foramen ovale and maxillary nerve (V2) at foramen rotundum. Image credit: Anatomist 90. licensed under the Creative Commons Attribution-Share Alike 3.0 Trigeminal ganglion 2011.
The term stimulation-triggered signs/symptoms (STS) has been proposed to describe uncomfortable or noticeable motor or sensory effects of stimulation in patients with RNS. In a single institution case series, STS were seen in approximately 10% (six out of 58) of RNS implants.[
Electrical stimulation of the sensate meninges is likely to cause sensory symptoms while stimulation of the insensate brain is unlikely to cause symptoms. It is plausible that volume conduction of electrical current to the nearby nerves led to the development of symptoms as the leads migrated closer to them. The previously described case series did not report lead inversion as a cause of STS.[
CONCLUSION
Facial sensations may be associated with stimulation of subtemporal strips using the RNS system. Newly elevated contact impedances may suggest lead migration, although other reasons such as gliosis can also cause progressively elevated RNS lead impedance.[
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Dr. Haneef ’s work is funded by the Hogg foundation. Dr. Sheth is a consultant for Boston Scientific, Abbott, Neuropace, and Zimmer Biomet. Dr. Krishnan and Dr. Karimov reports no disclosures.
Conflicts of interest
There are no conflicts of interest.
References
1. Geller EB, Skarpaas TL, Gross RE, Goodman RR, Barkley GL, Bazil CW. Brain-responsive neurostimulation in patients with medically intractable mesial temporal lobe epilepsy. Epilepsia. 2017. 58: 994-1004
2. Gill I, Parrent AG, Steven DA. Trigeminal neuropathic pain as a complication of anterior temporal lobectomy: Report of 2 cases. J Neurosurg. 2016. 124: 962-5
3. Hixon AM, Brown MG, McDermott D, Destefano S, Abosch A, Kahn L. RNS modifications to eliminate stimulation-triggered signs or symptoms (STS): Case series and practical guide. Epilepsy Behav. 2020. 112: 107327
4. Sillay KA, Ondoma S, Wingeier B, Schomberg D, Sharma P, Kumar R. Long-term surface electrode impedance recordings associated with gliosis for a closed-loop neurostimulation device. Ann Neurosci. 2018. 25: 289-98