- Department of Neurosurgery, Niigata City General Hospital, 463-7 Shumoku, Chuo-ku, Niigata, Japan 950-1197
- Department of Pathology, Niigata City General Hospital, 463-7 Shumoku, Chuo-ku, Niigata, Japan 950-1197
Correspondence Address:
Osamu Sasaki
Department of Pathology, Niigata City General Hospital, 463-7 Shumoku, Chuo-ku, Niigata, Japan 950-1197
DOI:10.4103/2152-7806.159074
Copyright: © 2015 Sasaki O. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Sasaki O, Nakamura K, Nashimoto T, Shibuya H. Tumoral calcinosis involving the cervical spine. Surg Neurol Int 18-Jun-2015;6:109
How to cite this URL: Sasaki O, Nakamura K, Nashimoto T, Shibuya H. Tumoral calcinosis involving the cervical spine. Surg Neurol Int 18-Jun-2015;6:109. Available from: http://surgicalneurologyint.com/surgicalint_articles/tumoral-calcinosis-involving-cervical-spine/
Abstract
Background:Tumoral calcinosis (TC) is a disease of unknown etiology characterized by the presence of calcified masses in the juxta-articular regions of the extremities. Involvement of the cervical spine is very rare. In this report, the characteristics of TC of the cervical spine, including the clinical presentation, radiographic features, and surgical management are discussed.
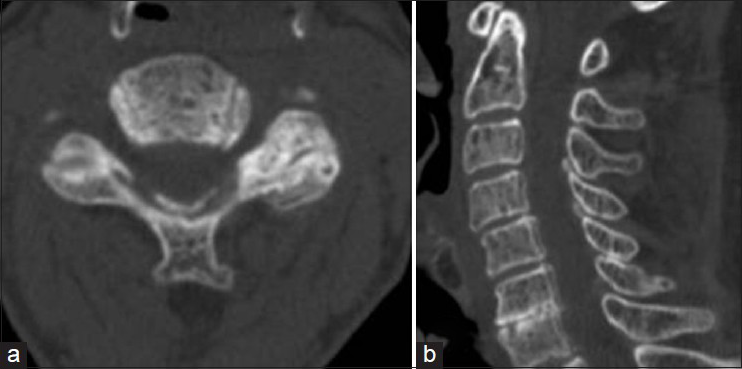
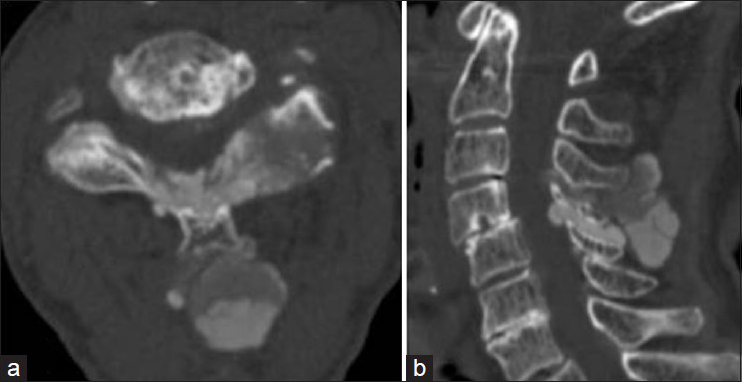
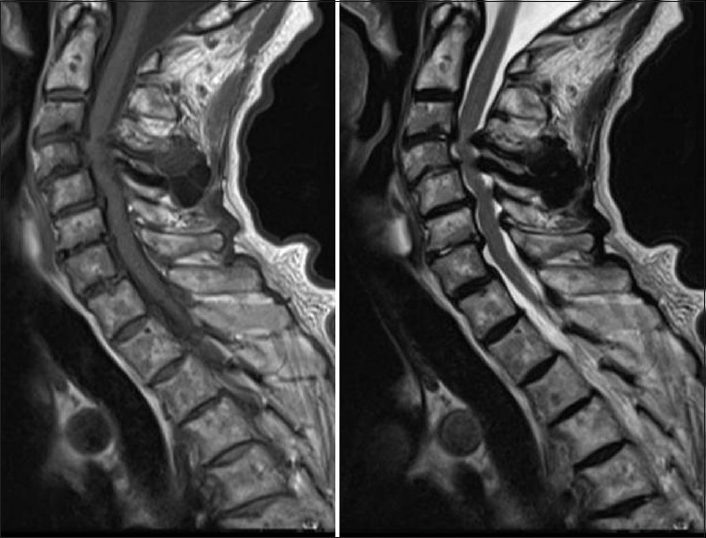
Case Description:A 90-year-old healthy female suffering from numbness of the upper extremities for 3 months presented with a 2-week history of progressive weakness of the lower extremities. A neurological examination revealed mild weakness and sensory impairment of the bilateral upper and lower extremities. Computed tomography (CT) scans demonstrated amorphous calcified masses posterior to the spinous process that extended into the interlaminar spaces of C3/4 and C4/5. The masses involved the posterior elements of C3-C4. Interestingly, CT scans performed 4 years earlier showed subtle calcification of a yellow ligament at C3/4 and C4/5. However, neither calcified masses nor bone erosion were observed. On magnetic resonance (MR) imaging, the mass showed hypointensity on T1- and T2-weighted images. The lesion was compressing the spinal cord and was resected surgically. The pathological findings were consistent with those of TC. The natural history of TC is not understood. However, this case suggests that calcified masses may progress within several years and that the bone around the mass may be involved. Postoperatively, residual masses may disappear spontaneously, while new bone is formed in the erosive lamina and facet.
Conclusion:The treatment of choice for TC, if the lesion causes progressive symptoms, is surgical resection.
Keywords: Cervical spine, myelopathy, tumoral calcinosis
INTRODUCTION
Tumoral calcinosis (TC) is a pathological entity with an unknown cause characterized by the formation of calcified masses in the periarticular soft tissue.[
CASE REPORT
A 90-year-old female presented with a 2-week history of progressive spastic quadriparesis visited our clinic. The laboratory data showed no remarkable abnormalities.
CT and MRI findings. A computed tomography (CT) scan of the cervical spine [
Operation and postoperative course
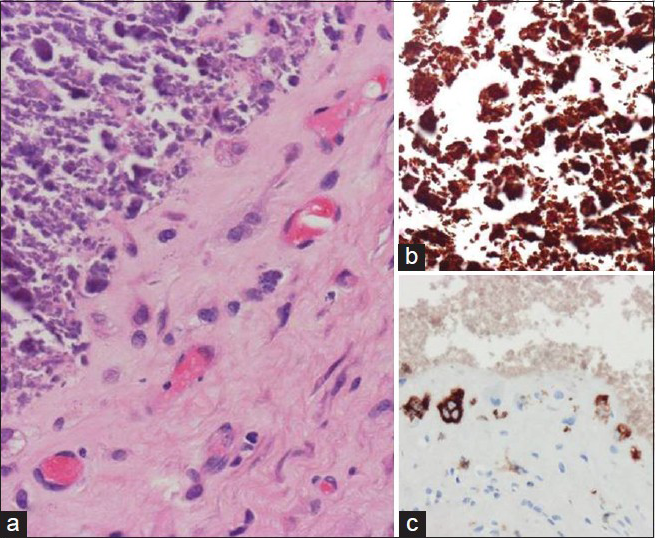
Calcification of the nuchal ligament was marked and, as the ligament was resected, leakage of yellow-whitish fluid was observed. In the interlaminar spaces of C3/4, a large calcified mass was observed. Laminotomy was performed at the C3/4 and C4/5 levels, and a large mass was resected. Pathological examinations [
The patient's postoperative course was good, and a CT scan showed some of the small calcified masses to be residual [
DISCUSSION
TC is a rare disease of unknown etiology characterized by the presence of large calcified masses occurring predominantly in the juxta-articular regions of the extremities.[
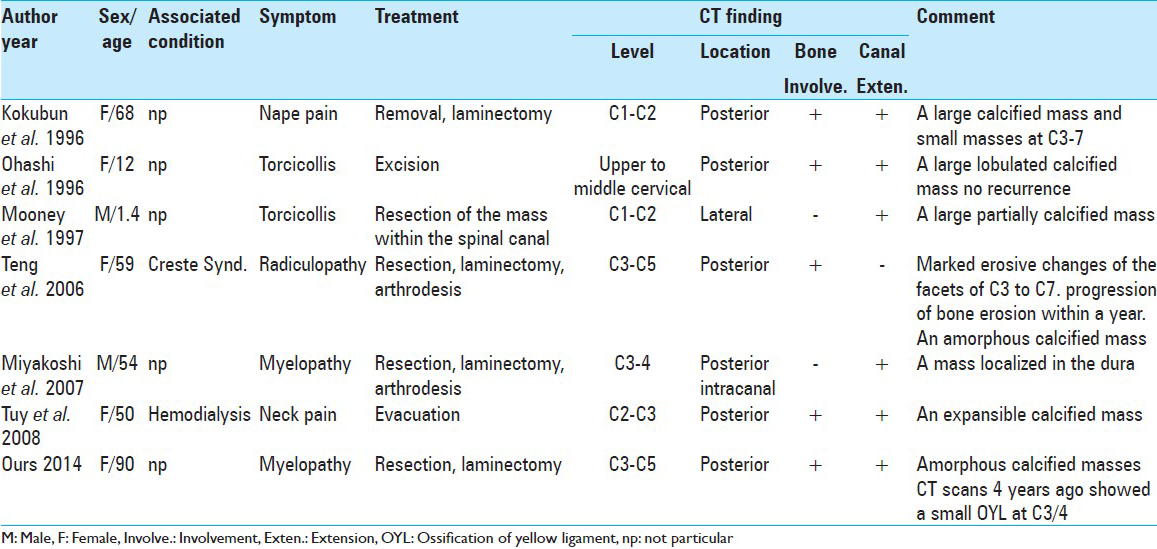
Reported Cases [
TC involving the cervical spine is rare, while only seven cases (including ours) having been reported.
The seven reported patients (five females and two males) ranged in age from 1.4 to 90 years.
Two patients presented with occipitalgia, two patients presented with torticollis and three patients developed neurologic signs. Two patients had underlying medical conditions: One reported a history of dialysis and one had Creaste Syndrome. The level affected by the lesion was the upper cervical region in all patients, and the site of the lesion was posterior in six of the seven patients. The locations of the soft tissue around the spine, such as the nuchal ligament, interspinous ligament, and yellow ligament were all posterior.
Neuroradiology
TC presents with lobulated, calcified, expansible masses on CT scans.[
Methods of treatment
The natural history of idiopathic TC is not well understood. The present case suggests that calcified masses may progress and that the bone around the mass may become involved within several years. The treatment of choice for TC, if the lesions cause progressive symptoms, is surgical removal of the mass.
At the time of an operation we adapted laminotomy, because this procedure seemed to be less invasive for the present elderly patient. The calcified mass extending into the spinal canal through the interlaminar space could be resected and the spinal cord was decompressed.
References
1. Durant DM, Riley LH, Burger PC, McCarthy EF. Tumoral calcinosis of the spine a study of 21 cases. Spine. 2001. 26: 1673-9
2. Kokubun S, Ozawa H, Sakurai M, Tanaka Y. Tumoral calcinosis in the upper cervical spine: A case report. Spine. 1996. 21: 249-52
3. Miyakoshi N, Shimada Y, Kasukawa Y, Ando S. Progressive myelopathy due to idiopathic intraspinal tumoral calcinosis of the cervical spine. J Neurosurg Spine. 2007. 7: 362-5
4. Mooney JF, Glazier SS. Tumoral calcinosis of the cervical spine in an infant. J Neurosurg. 1997. 86: 162-
5. Ohashi K, Yamada T, Ishikawa T, Yamaguchi S, Nakajima H, Takagi M. Idiopathic tumoral calcinosis involving the cervical spine. Skeletal Radiol. 1996. 25: 388-90
6. Teng AL, Robbin MR, Furey CG, Easley SE, Abdu-Karim FW, Bohlman H. Tumoral calcinosis in the cervical spine in a patient with Crest syndrome. J Bone Joint Surg Am. 2006. 88: 193-7
7. Tuy BE, John TK, Uglialoro AD, Beebe KS, Vives MJ, Patterson FR. Tumoral calcinosis presenting as neck pain and lesion of the cervical spine. An J Orthop. 2008. 37: E191-5