- Department of Neurosurgery, Nanavati Superspeciality and Navneet Hi Tech Hospitals, Mumbai, Maharashtra, India
- King Edward Memorial Hospital and Seth G. S. Medical College, Mumbai, Maharashtra, India
- Navneet Hi Tech Hospitals, Mumbai, Maharashtra, India
Correspondence Address:
Mrudul M. Bhatjiwale
Navneet Hi Tech Hospitals, Mumbai, Maharashtra, India
DOI:10.4103/2152-7806.194062
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohinish G. Bhatjiwale, Mrudul M. Bhatjiwale, Ami Bhagat. Ultra-extended euthermic pulsed radiofrequency for the treatment of ophthalmic neuralgia: A case report with elaboration of a new technique. 14-Nov-2016;7:
How to cite this URL: Mohinish G. Bhatjiwale, Mrudul M. Bhatjiwale, Ami Bhagat. Ultra-extended euthermic pulsed radiofrequency for the treatment of ophthalmic neuralgia: A case report with elaboration of a new technique. 14-Nov-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/ultra%e2%80%91extended-euthermic-pulsed-radiofrequency-treatment-ophthalmic-neuralgia-case-report-elaboration-new-technique/
Abstract
Background:Pulsed radiofrequency although present for many years has been used little compared to ablative procedures for pain relief. Its use in trigeminal neuralgia is sparse and unreported in the ophthalmic division, where the possibility of sensory loss can lead to high morbidity. We wished to explore the potential of this reportedly safe modality for a prolonged duration in a highly sensitive anatomic neural location, however, in a very secure, structured, and staged manner.
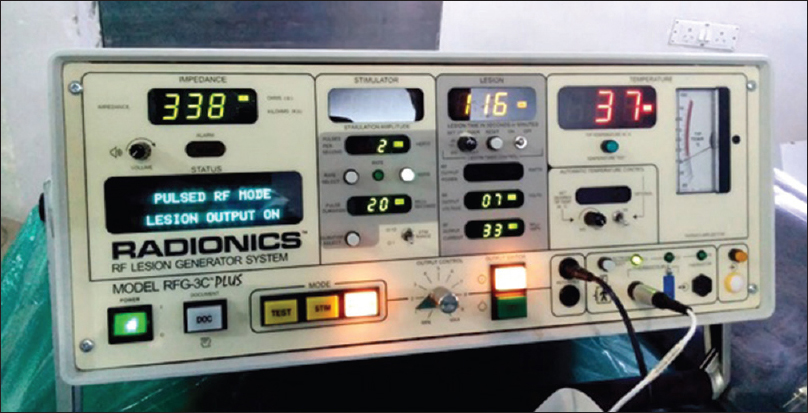
Case Description:A patient suffering from ophthalmic division (V1) medically uncontrolled neuralgia with a preoperative visual analog scale (VAS) score of 9/10 was subjected to a percutaneous pain relief procedure. The patient was treated with prolonged duration pulsed radiofrequency (PRF) for 40 min, with corneal sensation monitoring under conscious sedation keeping a low voltage (7 V) and tip temperature at 37°C. The patient obtained immediate relief, which was verified on the operation table itself. Postoperative VAS score of 0/10 was recorded. More than 6 months after the procedure, the patient is completely free from neuralgic pain and continues to have a VAS score of 0/10.
Conclusion:As opposed to conventional PRF where mostly a tip temperature of 42°C and high voltage have been used for 2 to a maximum of 8 min, PRF with a tip temperature of 37°C and a safe voltage of 7 V over an ultra-extended duration of 40 min can give a more distinct and effective but equally safe result. Although our case verified the safety and efficacy of prolonged duration PRF in sensitive anatomic locations, more studies are warranted for establishing this as a standard line of treatment. The specific use of PRF in ophthalmic division neuralgia in the manner described in our case report has hitherto not been reported in medical literature and will open a new vista in the minimally invasive treatment of this disease.
Keywords: Low voltage, ophthalmic, prolonged, pulsed-radiofrequency, trigeminal neuralgia
INTRODUCTION
Pulsed radiofrequency (PRF) is a technique used for creating a carefully controlled electrical field around an electrode. First used as a pain treatment option in the mid 1990's the technique involves application of discrete bursts of energy to the electrode intermittently. PRF is delivered in short (20 ms) bursts twice per second followed by a quiet phase (lasting 480 ms) in which no current is applied. This keeps the temperature very low, unlike the higher temperatures required for a radiofrequency ablation. Literature describes the use of short duration PRF for cervical and lumbar Z-joint pain, orchialgia, spinoradicular pain, and post-thoracotomy and inguinorraphy pain.[
CASE REPORT
A 56-year-old chemical worker suffered from severe paroxysms of pain in the left eye radiating to the forehead and above since 6 years. These attacks were triggered by exposure to wind during a bike ride or in an auto rickshaw when outdoors, or on exposure to the fan or a blast of cold air-conditioned air when indoors. They were also provoked by touching the eyelid and the forehead. The paroxysms of pain lasted for 3–4 s, causing watering in the eye, and made him stop his work. He used to have 15–20 such attacks per day. Subsequently, he was well controlled on carbamazepine 200 mg tds for 3 years, and later had moderate relief for the next 18 months despite the addition of pregabalin 75 mg bid and baclofen 30 mg OD extended release tablets. His pain was completely uncontrolled for the last 18 months, and the attacks had increased in duration and frequency. He could not tolerate any increase in the dosage of neuropathic medications and felt giddy with any such attempt. The visual analog score (VAS) score was calculated on a 10-point scale between 0 (no pain) and 10 (maximum tolerable pain). The preoperative score in our patient was 9/10.
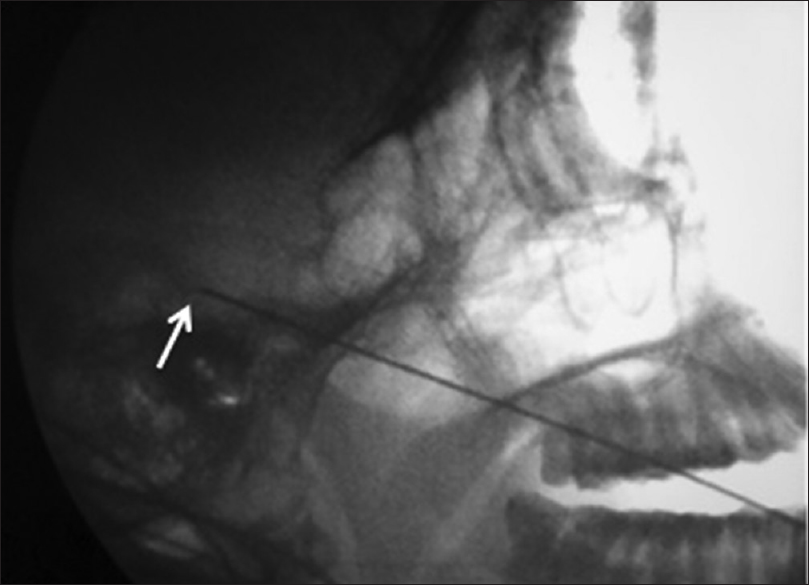
On examination, facial sensations, corneal sensations, motor examination of the face, and the rest of the neurological, systemic and vital parameter examinations were normal. His magnetic resonance imaging (MRI) showed no cerebellopontine angle lesion or vascular loop abutment at the root entry zone (REZ) of the trigeminal nerve. The patient was hence offered the options of a time-tested supraorbital neurectomy or long available but yet untested percutaneous procedure of PRF for V1 ophthalmic division with its possible uncertainties. The patient opted for a sensation sparing percutaneous day care procedure with its likely pros and cons. A new plan with minimum possible temperature (euthermia) and low voltage settings but prolonged duration was designed to obtain an optimum result with minimized chances of complications. Permission was obtained from the local institutional body for the same. Local anesthesia was administered at the site of introduction of the RF needle (5 mm bare tip, straight, Radionics). Using Hartel's technique and the Dr. G. M. Khan guideline, under C arm guidance the needle was introduced through the foramen ovale.[
DISCUSSION
Continuous radiofrequency (CRF) or radiofrequency thermocoagulation (RFTC) is a popular procedure being practiced for nearly four decades.[
There are few reports of the use of PRF for idiopathic trigeminal neuralgia.[
Mandibular (V3) and maxillary (V2) divisions are much more frequently affected by neuralgia than the ophthalmic division (V1).[
The patient was comfortable under dexmedetomidine conscious sedation. This lent a unique opportunity to have regular quick and effective monitoring of neural integrity intraoperatively in the form of intact corneal sensations and consciousness. As the patient continued to be well preserved, we proceeded to our set goal of raising the pain threshold to double its initial value to ensure long-term relief and could achieve it safely. Our case, thus, demonstrates that pain relief can be immediate as well as complete in PRF just as in RFTC but without its associated sensory and motor deficits. This, however, needed application of PRF for an extended duration keeping the tip temperature of RF needle as well as voltage low. The case also demonstrates for the first time in medical literature the safety of the application of PRF for a prolonged duration of 40 min without any disturbance of heart rate, blood pressure, consciousness, or corneal sensations. It opens way for further use of PRF in the application of ophthalmic neuralgia where RFTC has been a contraindication for nearly four decades. PRF may involve a temperature-independent pathway mediated by a rapidly changing electrical field, as our case demonstrated, because it was conducted at normal body temperature of 37°C. Chua et al. suggested that one of the main reasons for unsatisfactory results with PRF is the insufficient PRF dose applied in some of the studies.[
Other percutaneous techniques developed to overcome the limitations of RF ablation include glycerol rhizolysis and percutaneous microballoon compression (PMC). Gamma knife radiosurgery (GKR) is also known to be a minimally invasive and effective treatment for trigeminal neuralgia. However, potential eye complications including dry eye and corneal numbness have been reported.[
Although surgeons were initially optimistic about the procedure, glycerol rhizolysis is a destructive procedure, and its success rate is not high.[
PMC is a simple and effective treatment for trigeminal neuralgia. Sean Mullan introduced the technique of percutaneous balloon compression for trigeminal neuralgia in 1983 based upon the concept that intraoperative manipulation of the trigeminal ganglion gives pain relief.[
RF systems facilitate fully controlled, selective lesioning. There is no way to predict or to control the degree and extent of lesioning in methods such as peripheral alcohol blocks, glycerol rhizolysis, balloon microcompression,[
These preliminary findings from a single patient need to be validated by well-designed studies. An ideal cure for trigeminal neuralgia would mean reversal of the demyelination process in the sensory root by remyelination, if need be, by direct injection of stem cells.[
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest.
References
1. Abdennebi B, Bouatta F, Chitti M, Bougatene B. Percutaneous balloon compression of the gasserian ganglion in trigeminal neuralgia. Long-term results in 150 cases. Acta Neurochir. 1995. 36: 72-4
2. Asplund P, Blomstedt P, Bergenheim AT. Percutaneous Balloon Compression vs Percutaneous Retrogasserian Glycerol Rhizotomy for the Primary Treatment of Trigeminal Neuralgia. Neurosurgery. 2016. 78: 421-8
3. Bangash T. Trigeminal Neuralgia: Frequency of Occurrence in Different Nerve Branches. Anesth Pain Med. 2011. 1: 70-2
4. Blomstedt PC, Bergenheim AT. Technical difficulties and perioperative complications of retrogasserian glycerol rhizotomy for trigeminal neuralgia. Stereotact Funct Neurosurg. 2002. 79: 168-81
5. Bogduk N. Pulsed radiofrequency. Pain Med. 2006. 7: 396-407
6. Brown JA. Percutaneous Balloon Compression for Trigeminal Neuralgia. Clin Neurosurg. 2009. 56: 73-8
7. Brown JA, Gouda JJ. Percutaneous balloon compression of the trigeminal nerve. Neurosurg Clin N Am. 1997. 8: 53-62
8. Brown JA, Pilitsis JG. Percutaneous balloon compression for the treatment of trigeminal neuralgia: Results in 56 patients based on balloon compression pressure monitoring. Neurosurg Focus. 2005. 18: E10-
9. Brown JA, Preul MC. Percutaneous microcompression of the trigeminal ganglion. Neurosurgery. 1988. 23: 270-
10. Byrd D, Mackey S. Pulsed radiofrequency for chronic pain. Curr Pain Headache Rep. 2008. 12: 37-41
11. Chua N, Vissers K, Sluijter M. Pulsed radiofrequency treatment in interventional pain management: Mechanisms and potential indications—A review. Acta Neurochir. 2011. 153: 763-71
12. Cohen SP, Sireci A, Wu CL, Larkin TM, Williams KA, Hurley RW. Pulsed Radiofrequency of the Dorsal Root Ganglia is Superior to Pharmacotherapy or Pulsed Radiofrequency of the Intercostal Nerves in the Treatment of Chronic Postsurgical Thoracic Pain. Pain Physician. 2006. 9: 227-36
13. Cohen SP, Zundert J. Pulsed radiofrequency: Rebel without cause. Reg Anesth Pain Med. 2010. 35: 8-10
14. Erdine S, Bilir A, Cosman ER, Cosman ER. Ultrastructural changes in axons following exposure to pulsed radiofrequency fields. Pain Pract. 2009. 9: 407-17
15. Erdine S, Ozyalcin NS, Cimen A, Celik M, Talu GK, Disci R. Comparison of Pulsed Radiofrequency with conventional radiofrequency in treatment of idiopathic trigeminal neuralgia. Eur J Pain. 2007. 11: 309-13
16. Fransen P. Cost-effectiveness in the surgical treatments for trigeminal neuralgia. Acta Neurol Belg. 2012. 112: 245-7
17. Kanpolat Y, Savas A, Bekar A, Berk C. Percutaneous Controlled Radiofrequency Trigeminal Rhizotomy for the Treatment of Idiopathic Trigeminal Neuralgia: 25-year Experience with 1600 Patients. Neurosurgery. 2001. 48: 524-34
18. Kaplan M, Erol FS, Ozveren MF, Topsakal C, Sam B, Tekdemir I. Review of complications due to foramen ovale puncture. J Clin Neurosci. 2007. 14: 563-8
19. Khan I, Nadeem M. Percutaneous Retrogasserian Glycerol Rhizolysis in the Management of Trigeminal Neuralgia. RMJ. 2008. 33: 225-7
20. Lopez BC, Hamlyn PJ, Zakrzewska JM. Stereotactic radiosurgery for primary trigeminal neuralgia: State of the evidence and recommendations for future reports. J Neurol Neurosurg Psychiatry. 2004. 75: 1019-24
21. Lopez BC, Hamlyn PJ, Zakrzewska JM. Systematic review of ablative neurosurgical techniques for the treatment of trigeminal neuralgia. Neurosurgery. 2004. 54: 973-83
22. Mathieu D, Effendi K, Blanchard J, Séguin M. Comparative study of Gamma Knife surgery and percutaneous retrogasserian glycerol rhizotomy for trigeminal neuralgia in patients with multiple sclerosis. J Neurosurg. 2012. 117: 175-80
23. Matsuda S, Serizawa T, Sato M, Ono J. Gamma knife radiosurgery for trigeminal neuralgia: The dry-eye complication. J Neurosurg. 2002. 97: 525-8
24. Naseri A, Patel N. Vision loss as a complication of gamma knife radiosurgery for trigeminal neuralgia. Br J Ophthalmol. 2004. 88: 1225-6
25. Pollock BE, Phuong LK, Foote RL, Stafford SL, Gorman DA. High-dose trigeminal neuralgia radiosurgery associated with increased risk of trigeminal nerve dysfunction. Neurosurgery. 2001. 49: 58-64
26. ReaWilliam R, Kapur S, Mutagi H. Radiofrequency therapies in chronic pain. Contin Educ Anaesth Crit Care Pain. 2011. 11: 35-8
27. Serrano-Rubio AA, Martinez-Manrique JJ, Revuelta-Gutierrez R, Gomez-Amador JL, Martinez-Anda JJ, Ponce-Gomez JA. Linear accelerator-based stereotactic radiosurgery for the treatment of trigeminal neuralgia. Nine years’ experience in a single institution, Rev Neurol. 2014. 59: 249-54
28. Sluijter ME, Cosman ER, Rittmann WB, VanKleef M. The effect of pulsed radiofrequency fields applied to the dorsal root ganglion. Pain Clin. 1998. 11: 109-17
29. Strojnik T, Smigoc T. Percutaneous Trigeminal Ganglion Balloon Compression Rhizotomy: Experience in 27 Patients. Scientific World Journal 2012. 2012. p. 328936-
30. Spaziante R, Cappabianca P, Peca C, de Divitiis E. Subarachnoid hemorrhage and “normal pressure hydrocephalus”: Fatal complication of percutaneous microcompression of the gasserian ganglion. Case report. Neurosurgery. 1988. 22: 148-51
31. Sweet WH, Poletti CE. Problems with Retrogasserian Glycerol in the Treatment of Trigeminal Neuralgia. Appl Neurophysiol. 1985. 48: 252-7
32. Taha JM, Tew JM. Comparison of surgical treatments for trigeminal neuralgia: Reevaluation of radiofrequency rhizotomy. Neurosurgery. 1996. 38: 865-71
33. Tanaka N, Yamaga M, Tateyama S, Uno T, Tsuneyoshi I, Takasaki M. The effect of pulsed radiofrequency current on mechanical allodynia induced with resiniferatoxin in rats. Anesth Analg. 2010. 111: 784-90
34. Thapa D, Ahuja V1, Dass C, Verma P. Management of Refractory trigeminal neuralgia using extended duration pulsed radiofrequency application. Pain Physician. 2015. 18: E433-5
35. Urculo E, Alfaro R, Arrazola M, Astudillo E, Rejas G. Trochlear nerve palsy after repeated percutaneous balloon compression for recurrent trigeminal neuralgia: Case report and pathogenic considerations. Neurosurgery. 2004. 54: 505-8
36. Van Zundert J, Brabant S, Van de Kelft E, Vercruyssen A, Van Buyten JP. Pulsed radiofrequency treatment of the Gasserian ganglion in patients with idiopathic trigeminal neuralgia. Pain. 2003. 104: 449-52
37. Vengsarkar U.editorsSelective Radiofrequency Thermocoagulation of the Trigeminal Root for the relief of Trigeminal Neuralgia. A personal experience with 2000 cases over twenty years. Mumbai: Bhalani Publishing House; 2006. p. 1-16
38. Zahra H, Teh BS, Paulino AC, Yoshor D, Trask T, Baskin D. Stereotactic radiosurgery for trigeminal neuralgia utilizing the BrainLAB Novalis system. Technol Cancer Res Treat. 2009. 8: 407-12