- Department of Neurosurgery, Memfys Hospital for Neurosurgery, Enugu, Nigeria, Japan.
- Department of Neurosurgery, Shinshu University School of Medicine, Matsumoto, Japan.
Correspondence Address:
Kohei Kanaya, Department of Neurosurgery, Shinshu University School of Medicine, Matsumoto, Japan.
DOI:10.25259/SNI_276_2023
Copyright: © 2023 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Campbell Chukwuebuka Francis1, Kohei Kanaya2, Hiromu Murase2, Ridzky Firmansyah Hardian2, Tetsuyoshi Horiuchi2, Samuel Chukwunonyerem Ohaegbulam1. Unexpected recovery from complete deafness to normal hearing post surgical excision of a cerebellopontine angle meningioma: A case report. 19-May-2023;14:174
How to cite this URL: Campbell Chukwuebuka Francis1, Kohei Kanaya2, Hiromu Murase2, Ridzky Firmansyah Hardian2, Tetsuyoshi Horiuchi2, Samuel Chukwunonyerem Ohaegbulam1. Unexpected recovery from complete deafness to normal hearing post surgical excision of a cerebellopontine angle meningioma: A case report. 19-May-2023;14:174. Available from: https://surgicalneurologyint.com/surgicalint-articles/12331/
Abstract
Background: Cerebellopontine angle (CPA) meningioma presents a significant management challenge due to its intricate relationship with the brainstem neurovascular bundles. The emphasis in the past has been on facial nerve preservation, but the current management standard is hearing preservation in patients with serviceable hearing; however, hearing restoration after complete loss is rare. We report an elderly man who had restoration of hearing in the right ear after complete loss following tumor resection through the retrosigmoid route.
Case Description: A 73-year-old male patient presented with progressive hearing impairment in the right ear, culminating in hearing loss for about 2 months (the American Academy of Otolaryngology-Head and Neck Surgery [AAO-HNS] class D). He also had mild cerebellar symptoms, but other cranial nerves and long tracts were normal. Brain magnetic resonance imaging confirmed a right CPA meningioma, and he had tumor resection through the retrosigmoid route using meticulous microsurgical technique with vestibulocochlear nerve preservation, facial nerve monitoring, and intraoperative video angiography. He had restoration of hearing on follow-up (the American Academy of Otolaryngology-Head and Neck Surgery class A). Histology confirmed World Health Organization central nervous system grade 1 meningioma.
Conclusion: This case illustrates that hearing restoration is possible after complete loss in patients with CPA meningioma. We advocate hearing preservation surgery even in patients with non-serviceable hearing, as the chance of hearing recovery is possible.
Keywords: Cerebellopontine angle meningioma, Hearing preservation, Hearing restoration, Retrosigmoid approach
INTRODUCTION
Meningioma is the second most common tumor in the cerebellopontine angle (CPA), accounting for 10–15% of mass lesions.[
The emphasis in the past has been tumor excision and facial nerve preservation; however, with improvement in microneurosurgery and neurophysiological monitoring, hearing preservation is achievable.[
We report a case of an elderly man who had loss of hearing (the American Academy of Otolaryngology-Head and Neck Surgery [AAO-HNS] class D) in the right ear caused by CPA meningioma and had hearing restoration to normal after tumor excision through the retrosigmoid approach. The current emphasis on managing CPA tumors should attempt hearing preservation in patients with CPA meningioma despite the preoperative hearing status.
CASE PRESENTATION
We report a 73-year-old man who presented to our outpatient department with a 3-year history of painless but progressive hearing impairment in the right ear, culminating in hearing loss about 2 months before the presentation. There were associated dizziness and mild gait disturbances. He has well-controlled diabetes and hypertension and is a gastric cancer survivor with no feature of recurrence for more than 20 years.
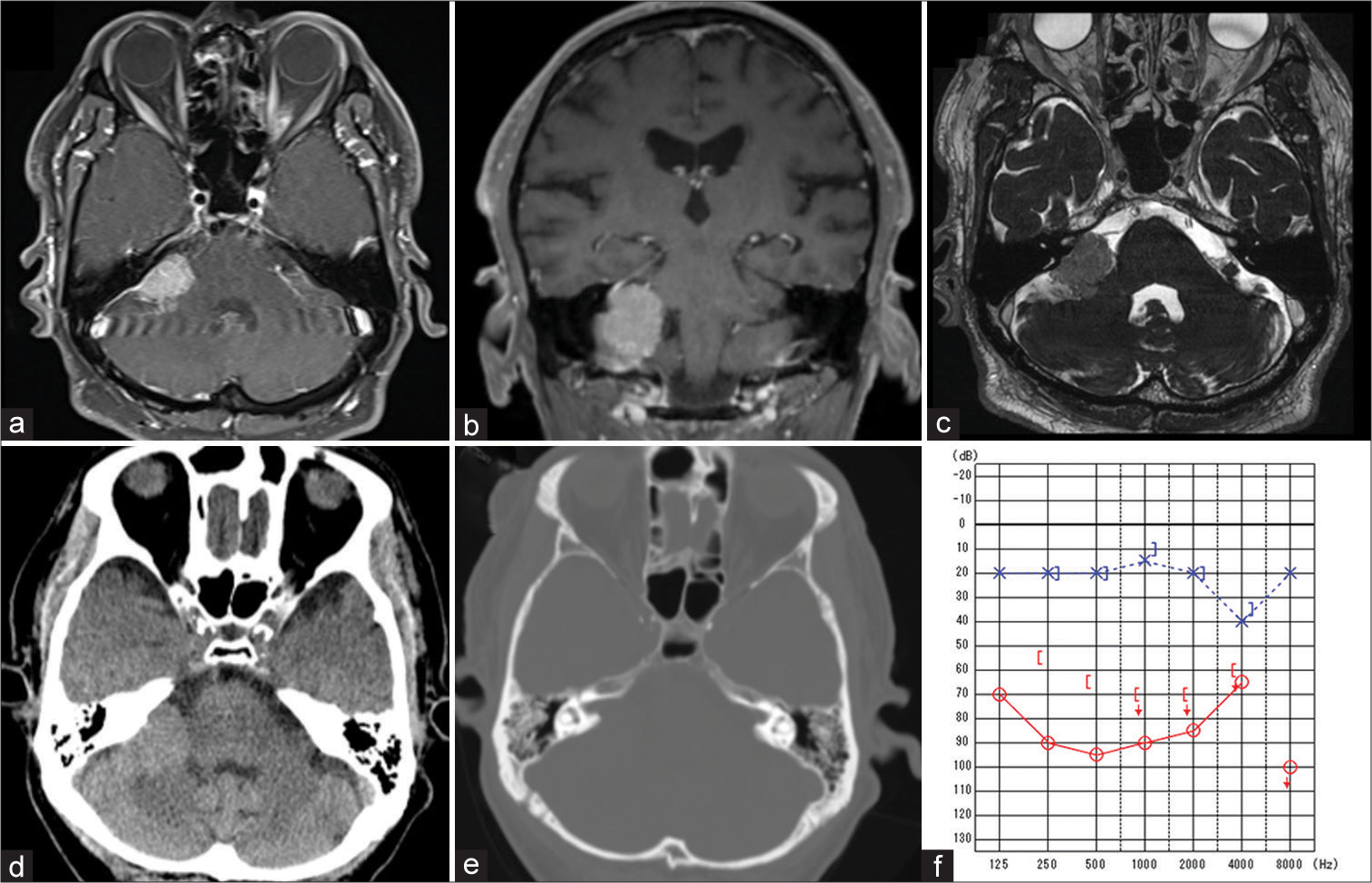
Brain magnetic resonance imaging (MRI) showed a right-sided CPA meningioma measuring 26 × 15 × 30 mm filling the cistern and significant cerebellar peduncular compression [
Figure 1:
Preoperative brain magnetic resonance imaging showing a right-sided cerebellopontine angle (CPA) meningioma with associated effacement of the ipsilateral CPA cistern and cerebellar compression on gadolinium-enhanced T1-weighted image (a and b) and constructive interference in steady state (c). Brain computed tomography scan showing no calcification in the tumor and normalsized and symmetrical internal acoustic meatus (d and e). Preoperative pure-tone audiometry showing 90 decibels in the right ear (f).
Significant examination findings were a conscious man with intact higher cerebral function (Mini-mental state examination 30). He had sensorineural hearing loss in the right ear, pure-tone audiometry (PTA) was 90 decibels (dB), and the speech discrimination test was 0 (AAO-HNS class D) [
The routine workup was done, and he had a right retrosigmoid craniotomy in the supine-lateral position. Facial nerve monitoring was done using motor-evoked potential and electromyography; however, auditory brainstem response was not performed due to the profound hearing loss. The tumor was firm and occupied the right CPA cistern with attachment to the dura anterior to the internal acoustic meatus and adjacent parts of the petrous bone and extending posteriorly. It displaced the facial-vestibulocochlear nerve complex superolateral and the lower cranial nerves inferiorly. About 95% of tumor resection was achieved with an operating microscope and cavitron ultrasonic aspirator; however, a minute segment of the lesion that was morbidly adherent to the right facial and vestibulocochlear nerves was left in situ. Internal acoustic meatus was not drilled because the tumor did not invade it. Intraoperative video indocyanine green fluorescent angiography and micro-Doppler ultrasound were used to confirm the patency of regional vessels during tumor resection and before wound closure. Hemostasis was secured, and the wound was closed without drainage.
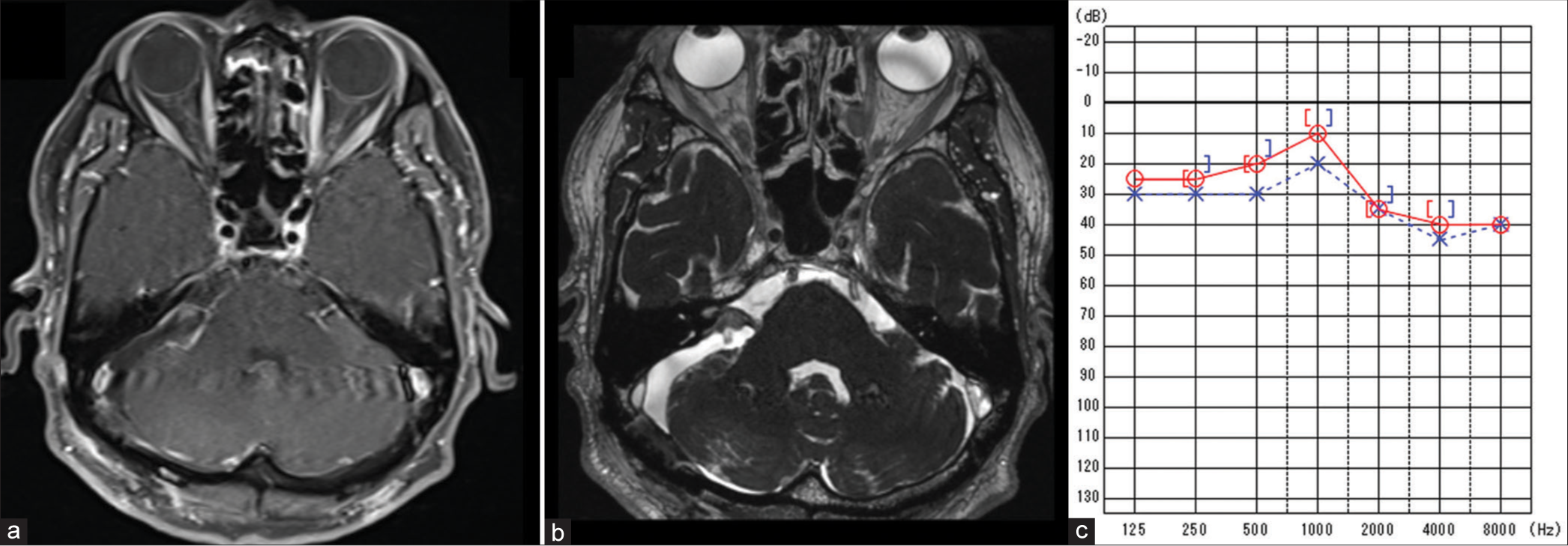
Postoperative recovery was uneventful, and he was discharged home after about 1 week of admission. Postoperative MRI showed satisfactory tumor excision with small remnant of the tumor around the rihgt facial-vestibulocochlear nerve complex [
DISCUSSION
CPA meningioma poses a significant surgical challenge due to its anatomic complexity and arborization with the middle and lower neurovascular complex.[
This index patient had profound hearing impairment, which was non-serviceable by definition (AAO-HNS class D) before surgical intervention and had hearing restoration to normal (AAO-HNS class A) within 2 months after surgery. We opted for the retrosigmoid route, a versatile operative corridor that affords a panoramic view of the CPA cistern and enables early identification of the facial nerve close to the brainstem and other surrounding neurovascular structures in the CPA cistern.[
The pathoanatomic characteristics of the tumor suggest a premeatal type since it originates from the petrous dura anterior to and involves the internal auditory canal (IAC), and further extends inferolateral toward the lower neurovascular complex. It displaced the facial and vestibulocochlear nerve complex anterosuperiorly and the lower cranial nerve inferiorly. The premeatal tumors are generally challenging due to their intimate relationship with the IAC and its associated neurovascular structures and often present early with hearing disturbances,[
Schaller et al. found that premeatal tumors become symptomatic earlier when compared to retromeatal types and have worse postoperative functional outcomes.[
Gross total resection should be attempted in CPA meningioma if possible to achieve cure nevertheless, due to their intimate relationship to the brainstem middle and lower neurovascular complex, subtotal or near-total resection are options for tumors morbidly adherent to critical neurovascular structures.[
Unlike CPA meningioma, vestibular schwannoma (VS) is of intraneural origin and has a more intimate relationship with the cochlear nerve with which it shares similar vascular feeders and may be disrupted during tumor extirpation.[
We advocate an attempt at hearing preservation for all CPA meningioma irrespective of lesion size, topographic type, and preoperative hearing status, as seen in this index case who had both anatomic and unfavourable clinical factors yet had hearing restoration (AAO-HNO class A). Utilizing hearing-saving approaches and preserving the cochlear nerve should be the goal in all cases of CPA meningioma, irrespective of the serviceability of the hearing status.
CONCLUSION
This case illustrates that hearing restoration is possible after complete loss in patients with CPA meningioma. Utilizing the retrosigmoid approach and meticulous microsurgical techniques to preserve the vestibulocochlear nerve and its associated neurovascular bundles and neurophysiological monitoring are veritable to ensure success. We advocate hearing preservation surgery even in patients with non-serviceable hearing, as the chance of hearing recovery is possible.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Agarwal V, Babu R, Grier J, Adogwa O, Back A, Friedman AH. Cerebellopontine angle meningiomas: Postoperative outcomes in a modern cohort. Neurosurg Focus. 2013. 35: E10
2. Batra PS, Dutra JC, Wiet RJ. Auditory and facial nerve function following surgery for cerebellopontine angle meningiomas. Arch Otolaryngol Head Neck Surg. 2002. 128: 369-74
3. Cohen NL, Lewis WS, Ransohoff J. Hearing preservation in cerebellopontine angle tumor surgery: TheNYU experience 1974-1991. Am J Otol. 1993. 14: 423-33
4. Ito T, Kasuya M. Classification of meningiomas. Gan. 1950. 41: 61-2
5. Katsuta T, Inoue T, Uda K, Masuda A. Hearing restoration from deafness after resection of a large cerebellopontine angle meningioma--case report. Neurol Med Chir (Tokyo). 2001. 41: 352-5
6. Kiyomizu K. Hearing improvement after conservative approach for large C-P angle meningioma. Otolaryngol Head Neck Surg. 2004. 76: 765-9
7. Nakamura M, Roser F, Dormiani M, Matthies C, Vorkapic P, Samii M. Facial and cochlear nerve function after surgery of cerebellopontine angle meningiomas. Neurosurgery. 2005. 57: 77-89
8. Okwunodulu O, Campbell FC, Inojie MO, Ndubuisi CA, Hart IT. Obstructive hydrocephalus with impaired ventricular compliance resulting in visual deterioration in an adult with vestibular schwannoma. IOSR-JDMS. 2020. 19: 8-11
9. Sanna M, Karmarkar S, Landolfi M. Hearing preservation in vestibular schwannoma surgery: Fact or fantasy?. J Laryngol Otol. 1995. 109: 374-80
10. Schaller B, Merlo A, Gratzl O, Probst R. Premeatal and retromeatal cerebellopontine angle meningioma. Two distinct clinical entities. Acta Neurochir (Wien). 1999. 141: 465-71
11. Sweeney AD, Carlson ML, Ehtesham M, Thompson RC, Haynes DS. Surgical approaches for vestibular schwannoma. Curr Otorhinolaryngol Rep. 2014. 2: 25664
12. Trevisi G, Beggio G, Raneri F. Hearing preservation in vestibular schwannoma surgery. Acta Neurochir (Wien). 2020. 162: 71
13. Voss NF, Vrionis FD, Heilman CB, Robertson JH. Meningiomas of the cerebellopontine angle. Surg Neurol. 2000. 53: 439-46