- Department of Neurosurgery, Avicenne Military Hospital of Marrakech, Mohammed V University, Rabat, Morocco.
- Department of Radiology, Avicenne Military Hospital of Marrakech, Mohammed V University, Rabat, Morocco.
- Department of Ophthalmology, Avicenne Military Hospital of Marrakech, Mohammed V University, Rabat, Morocco.
Correspondence Address:
Ali Akhaddar
Department of Neurosurgery, Avicenne Military Hospital of Marrakech, Mohammed V University, Rabat, Morocco.
DOI:10.25259/SNI_505_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ali Akhaddar1, Hassan Baallal1, Nabil Hammoune2, Salaheddine Bouabbadi3, Amine Adraoui1, Hatim Belfquih1. Unilateral blindness following superior laryngeal nerve block for awake tracheal intubation in a case of posterior cervical spine surgery. 05-Sep-2020;11:277
How to cite this URL: Ali Akhaddar1, Hassan Baallal1, Nabil Hammoune2, Salaheddine Bouabbadi3, Amine Adraoui1, Hatim Belfquih1. Unilateral blindness following superior laryngeal nerve block for awake tracheal intubation in a case of posterior cervical spine surgery. 05-Sep-2020;11:277. Available from: https://surgicalneurologyint.com/surgicalint-articles/10240/
Abstract
Background: Superior laryngeal nerve block (SUPLANEB) is a popular airway anesthesia technique utilized for successful awake endotracheal intubation in patients with significant cervical spine instability. If not performed by an expert, it carries the risk of general/neurologic complications that are typically minimal/transient. However, permanent blindness and/or upper cranial nerve neuropathies may occur. Here, we describe a case in which a young patient underwent an atlantoaxial fusion for a C2 nonunion (e.g., following a fracture) complicated by unilateral blindness due to a SUPLANEB.
Case Description: A 25-year-old neurologically intact male underwent a C1-C2 posterior arthrodesis to address a nonunion of a C2 fracture. To perform the awake nasotracheal intubation, a SUPLANEB was performed using a video laryngoscope. Although the operation was uneventful, postoperatively, the patient reported left visual loss accompanied by left-sided facial numbness and hearing loss. On examination of the left eye, the anterior segment and fundus examinations were normal, but the OCT (optical coherence tomography) and retinal angiography demonstrated left-sided postischemic retinal edema with permeability of the intraocular vessels. Although the cranio-orbital computed tomography scan showed only mild pneumocephalus, the CT angiogram scan revealed abnormal air in the left carotid sheath accompanied by diffuse subcutaneous emphysema. Further, brain and orbital magnetic resonance imaging scans were normal. The patient was treated with pure oxygen, systemic steroid therapy, and nimodipine. The pneumocephalus and subcutaneous emphysema resolved on day 3. At 2 months follow-up, the patient remained blind on the left side, but had no further neurological deficits.
Conclusion: Blindness and upper cranial nerves neuropathies should be considered as potential complications of SUPLANEB. Notably, these deficits were not directly related to the operative positioning or neurosurgical spinal procedure.
Keywords: Anesthesia, Blindness, Complication, Pneumocephalus, Spinal surgery, Superior laryngeal block
INTRODUCTION
Superior laryngeal nerve block (SUPLANEB) is a popular airway anesthetic technique utilized to facilitate awake endotracheal intubation in patients with cervical spine instability.[
Here, we present a patient undergoing atlantoaxial fusion who required an awake endotracheal intubation for general anesthesia. Postoperatively, the patient was immediately blind in the left eye and also complained of complete trigeminal anesthesia and ipsilateral hearing loss. This case and the possible mechanisms for these deficits are reviewed.
CASE REPORT
A 25-year-old neurologically intact male was admitted for elective fusion of a nonunion C2 fracture attributed to a diving accident 9 months earlier. Four months later, when neck pain appeared and worsened, both CT and MR studies demonstrated a type II odontoid fracture with a chronic nonunion accompanied by C1-C2 subluxation but without cord compression [
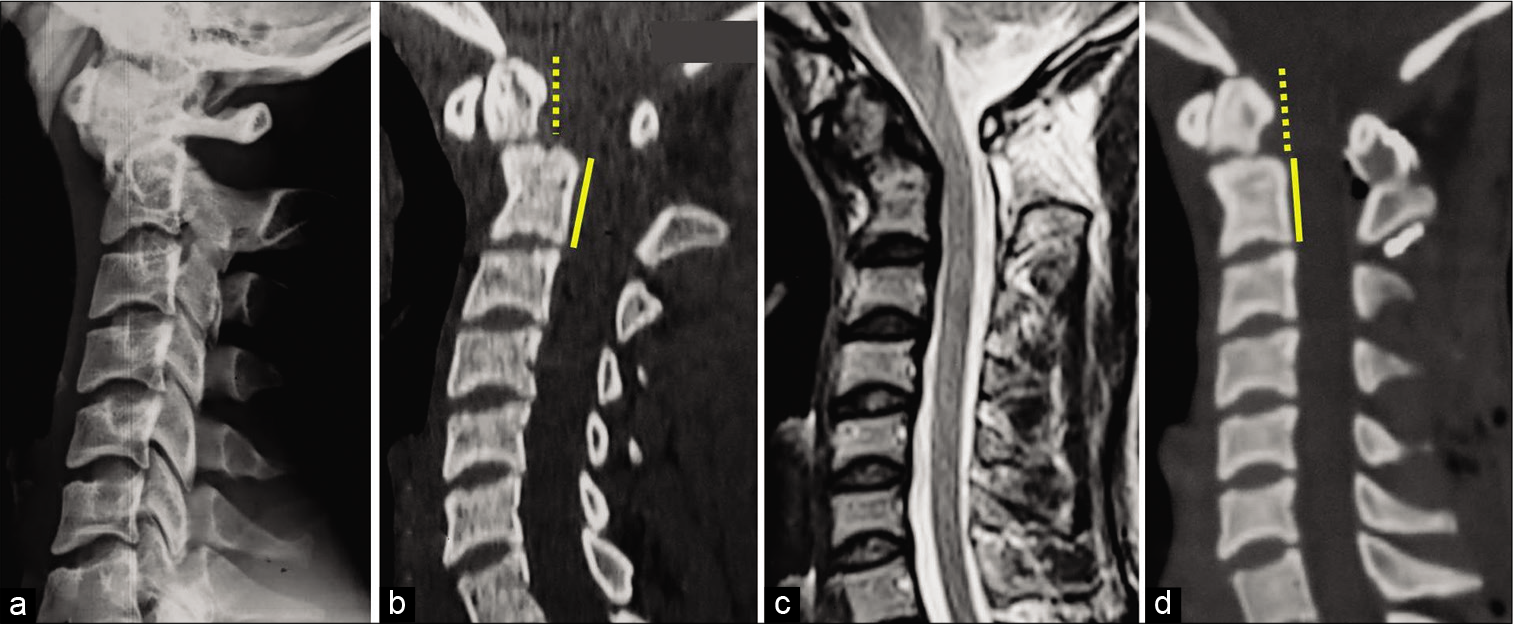
Figure 1:
Spinal cervical lateral plain radiography (a), sagittal computed tomography scan (CT scan) (b), and sagittal magnetic resonance imaging on T2-weighted image (c) showing type II nonunion odontoid fracture and C1-C2 subluxation without bulbomedullary compression. Postoperative sagittal CT scan following C1-C2 posterior cervical spine fusion (bicortical iliac crest allograft with laminar wiring were used).
Surgery
Before the C1-C2 posterior arthrodesis, the patient underwent an awake endotracheal intubation requiring SUPLANEB. The patient received hydroxyzine 50 mg orally, and the anesthesiologist performed a superior laryngeal nerve block. A 21-gauge needle (1 ½ inch) attached to a syringe containing 5 mL of 1% lidocaine was used once on each side (total injection of no more 10 mL of lidocaine), following which the patient was intubated using a video laryngoscope. The posterior cervical C1-C2 fusion was uneventful.
Nevertheless, after recovering from the general anesthesia, the patient complained of the left eye blindness without ocular pain, periorbital swelling, or oculomotor paresis; he also demonstrated left-sided hearing loss and facial numbness (all trigeminal territories). The direct eye examination revealed the left side anterior segment and fundus was normal, but confirmed complete left-sided visual loss, isolated direct mydriasis, and intact consensual light reflex.
Diagnostic studies
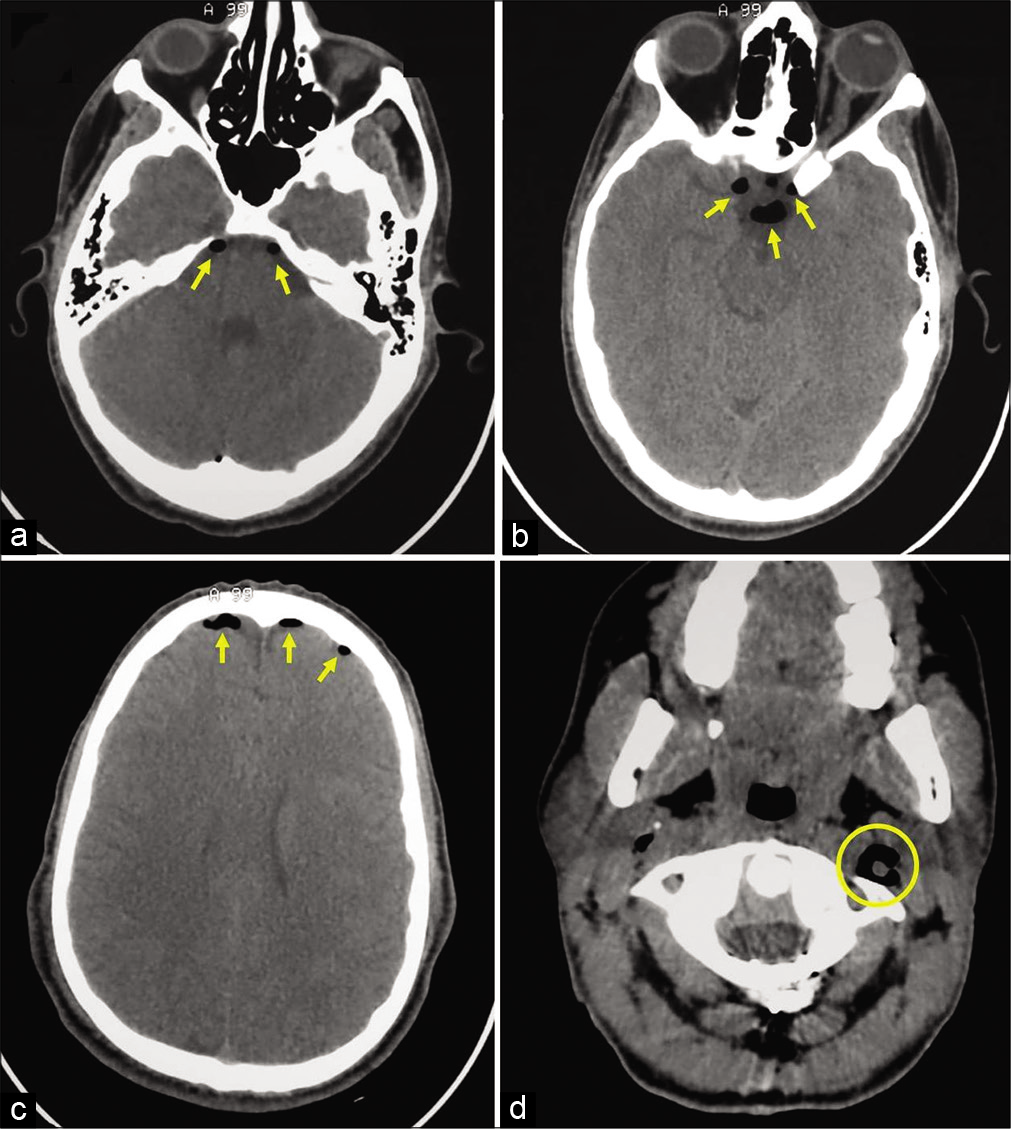
The STAT cranio-orbital computed tomography scan showed no acute intracranial or oculo-orbital lesions, but demonstrated mild bifrontal, interhemispheric, parasellar, sellar, and prepontic pneumocephalus; there was no skull base lesion [
Figure 2:
Axial cranial (a-c) and cervical C1 (d) computed tomography scan revealing mild pneumocephalus (arrows) at the prepontic cisterns (a), the sellar and laterosellar areas (especially next to the left optical channel) (b), and the bifrontal convexity (c). There is also a bilateral deep cervical emphysema and abnormal air in the left carotid sheath (d) (circle).
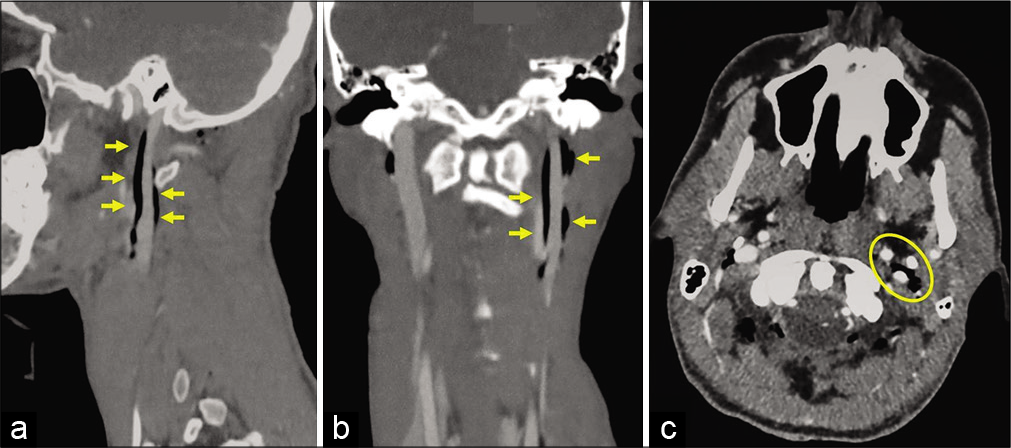
Figure 3:
Craniocervical angiographic on sagittal (a), coronal (b), and axial (c) views demonstrating abnormal air in the left carotid sheath: the air is present nearby and along the carotid bifurcation, the internal carotid artery, and all around the internal jugular vein (arrows). The yellow circle represents these last three vessels on axial view (c).
Treatment
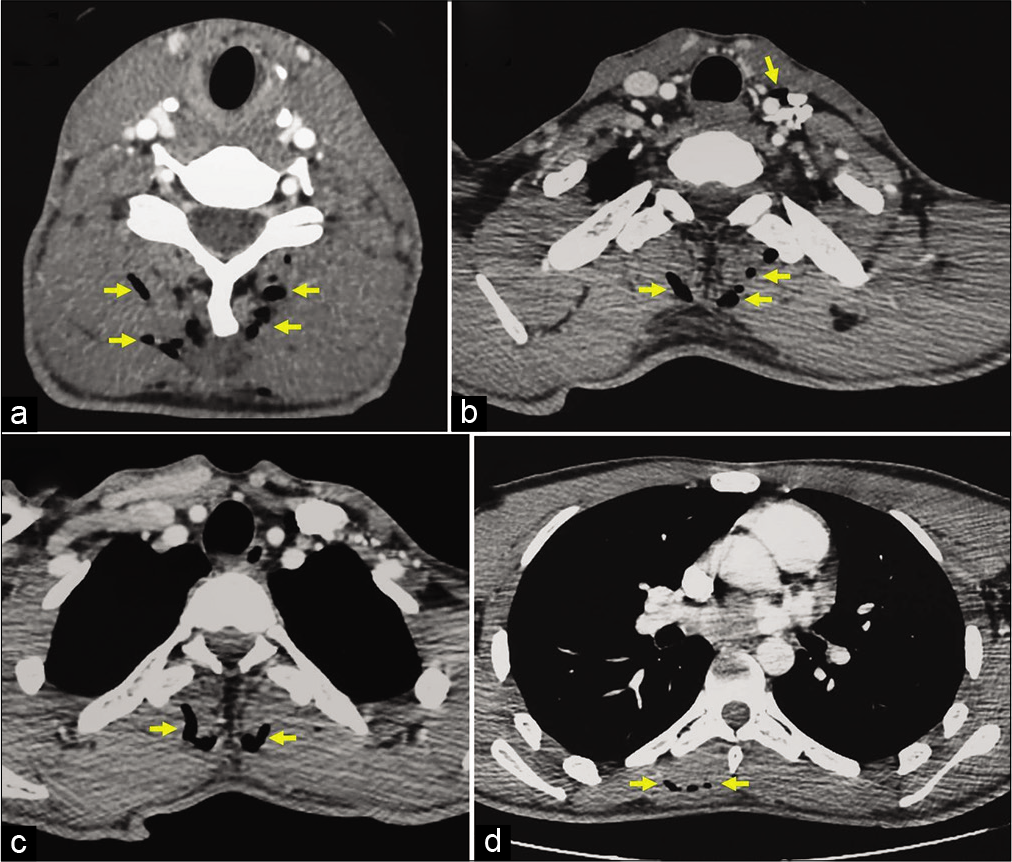
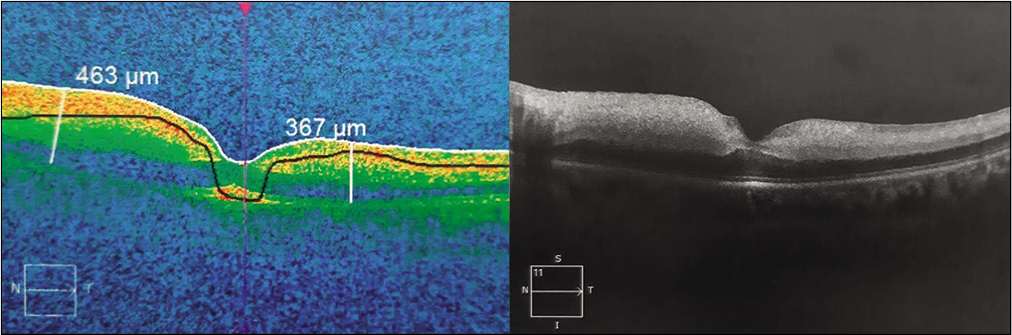
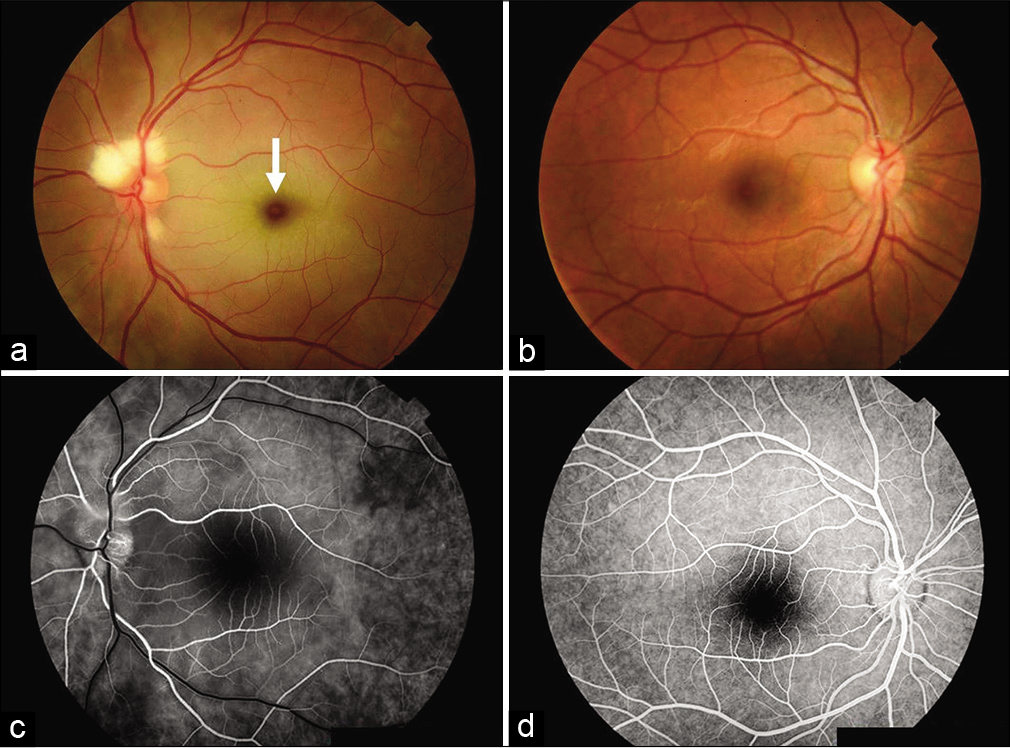
The patient was placed in strict horizontal position and treated with inspired pure oxygen plus systemic steroid pulse therapy (120 mg of methylprednisolone each 6 h) and nimodipine (30 mg each 6 h). The 1st postoperative day, the visual acuity remained unchanged, but nearly completely recovered the left hearing loss and facial hypoesthesia in the V2 distribution. Brain and orbital MR studies were normal. Optical coherence tomography (OCT) demonstrated postischemic retinal edema [
Figure 6:
Retinography (fundus photography on the 2nd postoperative day) of both eyes (left a and right b) revealing permeability of the intraocular blood vessels (especially the central retinal artery) and diffuse retinal edema on the left eye. Note the “Cherry-red spot” at the fovea (arrow) with white edematous macula around. OCT angiography features of the left eye (c) and right eye (d). There is a delayed choroidal filling in the left eye.
The pneumocephalus and subcutaneous emphysema completely resolved on postoperative day 3. At the time of discharge on the 4th postoperative day, there was a complete resolution of symptoms excepting for the left blindness and the V1 trigeminal hypoesthesia; the patient was sent home on nimodipine (120 mg/day) and oral steroid therapy (60 mg prednisolone) with a tapering dose over the next 4 weeks. Two months later, he remained blind in the left eye without any return of function.
DISCUSSION
Postoperative visual loss following prone spinal surgery is rare.[
Left-sided blindness
After an extensive ophthalmological exploration, it seems that our patient had postoperative ischemic retinal edema secondary to central retinal artery occlusion.
The iatrogenic intravascular infusion was likely the cause of pneumocephalus.[
Subcutaneous emphysema following a translaryngeal injection of local anesthetic has only rarely been reported in literature.[
Upper cranial neuropathies
The upper cranial neuropathies (II, V1, V2, V3, and VIII cranial nerves) were likely attributed to pneumocephalus in the sellar and laterosellar regions, the abnormal extracranial air into the left carotid sheath, and the extensive cervicothoracic subcutaneous emphysema. They were also likely due to the accidental injection of the local anesthetic inside/around the ICA and/or the IJV (e.g., extending into the left cavernous sinus). This would explain the partial cavernous sinus syndrome presented by the patient. Another hypothesis is that the SUPLANEB resulted in transient vasospasm, emboli, or hypoperfusion of the ICA, thus directly resulting in occlusion of the blood supply to the left optic nerve.[
Future recommendations
When SUPLANEB is performed, the anesthesiologist should take care not to push the needle too far or too lateral to avoid reaching the carotid sheath.[
CONCLUSION
Blindness and upper cranial nerve neuropathies must be considered as potential complications of the SUPLANEB utilized for endotracheal awake intubation for spinal neurosurgical/other procedures.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Publication of this article was made possible by the James I. and Carolyn R. Ausman Educational Foundation.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors thank Pr. Youssef Qamous (Department of Anesthesiology) and Pr. Younes Aissaoui (Department of Intensive Care Medicine) for their valuable suggestions in the management of this patient.
References
1. Akhaddar A, Boucetta M. Subconjunctival hemorrhage as a complication of intraoperative positioning for lumbar spinal surgery. Spine J. 2012. 12: 274
2. Bekar A, Türeyen K, Aksoy K. Unilateral blindness due to patient positioning during cervical syringomyelia surgery: Unilateral blindness after prone position. J Neurosurg Anesthesiol. 1996. 8: 227-9
3. Burger SK, Saul RF, Selhorst JB, Thurston SE. Transient monocular blindness caused by vasospasm. N Engl J Med. 1991. 325: 870-3
4. Choi YY, Hyun DK, Park HC, Park CO. Pneumocephalus in the absence of craniofacial skull base fracture. J Trauma. 2009. 66: E24-7
5. Cunqueiro A, Scheinfeld MH. Causes of pneumocephalus and when to be concerned about it. Emerg Radiol. 2018. 25: 331-40
6. Doyle DJ. Airway anesthesia: Theory and practice. Anesthesiol Clin. 2015. 33: 291-304
7. Epstein NE. Perioperative visual loss following prone spinal surgery: A review. Surg Neurol Int. 2016. 7: S347-60
8. Giordano D, Panini A, Pernice C, Raso MG, Barbieri V. Neurologic toxicity of lidocaine during awake intubation in a patient with tongue base abscess. Case report. Am J Otolaryngol. 2014. 35: 62-5
9. Han SS, Kim SS, Hong HP, Lee SY, Lee SJ, Lee BK. Massive paradoxical air embolism in brain occurring after central venous catheterization: A case report. J Korean Med Sci. 2010. 25: 1536-8
10. Hsu CH, Lin TC, Yeh CC, Ho ST, Wong CS. Convulsions during superior laryngeal nerve block-a case report. Acta Anaesthesiol Sin. 2000. 38: 93-6
11. Laurent PE, Coulange M, Bartoli C, Louis G, Souteyrand P, Gorincour G. Retrograde cerebral venous air embolism: A rare cause of intracranial gas. Diagn Interv Imaging. 2014. 95: 1113-5
12. Levinson B, Reddy S. Posterior ischemic optic neuropathy after extensive spine surgery: A case report and review of the literature. AANA J. 2019. 87: 37-42
13. Manikandan S, Neema PK, Rathod RC. Ultrasound-guided bilateral superior laryngeal nerve block to aid awake endotracheal intubation in a patient with cervical spine disease for emergency surgery. Anaesth Intensive Care. 2010. 38: 946-8
14. Mione G, Pische G, Wolff V, Tonnelet R, Humbertjean L, Richard S. Perioperative bioccipital watershed strokes in bilateral fetal posterior cerebral arteries during spinal surgery. World Neurosurg. 2016. 85: 367.e17-21
15. Ono Y, Okubo Y, Hashimoto K, Inokuchi R, Odajima H, Tase C. Massive subcutaneous emphysema, bilateral pneumothorax, pneumomediastinum, pneumoperitoneum, pneumoretroperitoneum, and pneumoscrotum after multiple direct laryngoscopies: An autopsy case report. J Anesth. 2015. 29: 622-6
16. Petridis AK, Maslehaty H, Doukas A, Mahvash M, Mehdorn HM. How did air get into the brain? A case of intracranial air in a patient without skull fracture. Acta Neurochir (Wien). 2011. 153: 1825-6
17. Pintaric TS. Upper airway blocks for awake difficult airway management. Acta Clin Croat. 2016. 55: 85-9
18. Thompson TP, Levy E, Kanal E, Lunsford LD. Iatrogenic pneumocephalus secondary to intravenous catheterization. Case report. J Neurosurg. 1999. 91: 878-80
19. Tran P, Reed EJ, Hahn F, Lambrecht JE, McClay JC, Omojola MF. Incidence, radiographical features, and proposed mechanism for pneumocephalus from intravenous injection of air. West J Emerg Med. 2010. 11: 180-5
20. Wong DT, McGuire GP. Subcutaneous emphysema following trans-cricothyroid membrane injection of local anesthetic. Can J Anaesth. 2000. 47: 165-8