- Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita Hospital, Narita City, Chiba, Japan.
Correspondence Address:
Yuhei Michiwaki, M.D., Ph.D., Department of Neurosurgery, International University of Health and Welfare, School of Medicine, Narita Hospital, Narita City, Chiba, Japan.
DOI:10.25259/SNI_607_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Yuhei Michiwaki, Masatou Kawashima, Tatsuya Tanaka, Ryohei Sashida, Yu Hirokawa, Tomihiro Wakamiya, Kazuaki Shimoji, Eiichi Suehiro, Keisuke Onoda, Fumitaka Yamane, Akira Matsuno. Unruptured aneurysm at bifurcation of super short middle cerebral artery mimicking duplicated middle cerebral artery aneurysm. 29-Jul-2022;13:329
How to cite this URL: Yuhei Michiwaki, Masatou Kawashima, Tatsuya Tanaka, Ryohei Sashida, Yu Hirokawa, Tomihiro Wakamiya, Kazuaki Shimoji, Eiichi Suehiro, Keisuke Onoda, Fumitaka Yamane, Akira Matsuno. Unruptured aneurysm at bifurcation of super short middle cerebral artery mimicking duplicated middle cerebral artery aneurysm. 29-Jul-2022;13:329. Available from: https://surgicalneurologyint.com/surgicalint-articles/11749/
Abstract
Background: Duplicated middle cerebral artery (DMCA) is a normal variation of the middle cerebral artery (MCA), and distinguishing DMCA from other arteries based only on the angiographical findings is sometimes difficult.
Case Description: Preoperative angiography of a 60-year-old woman revealed two MCAs originating near the top of the right internal carotid artery and a 6-mm-sized aneurysm located between these two MCAs. The ipsilateral A1 segment of the anterior cerebral artery was not visualized due to hypoplasia. The patient was diagnosed with an unruptured aneurysm at the bifurcation between MCA and DMCA, preoperatively. However, during clipping surgery, the hypoplastic A1 segment was observed at approximately 2 mm proximal to the bifurcation of the MCA, indicating that these two MCAs were not “true” MCA and DMCA, but rather two normal MCA trunks bifurcated from the very short prebifurcation segment of M1. This difference in interpretation was due to the fact that the hypoplastic A1 was not visualized on preoperative examinations. The patient was discharged following the surgery without any neurological deficits.
Conclusion: The distinction between DMCA and MCA trunks from the very short prebifurcation segment of MCA might be difficult, especially when the ipsilateral A1 segment is hypoplastic. Such an M1 with a length of 2–3 mm might be named super short M1. Thus, it is necessary to confirm the anatomy during aneurysm surgery.
Keywords: Aneurysm, Clipping, Duplicated middle cerebral artery, Short middle cerebral artery
A 60-year-old woman diagnosed with an unruptured intracranial aneurysm was admitted to our hospital for surgery. The patient presented no neurological symptoms and had a history of hypertension and surgery for oral cancer.
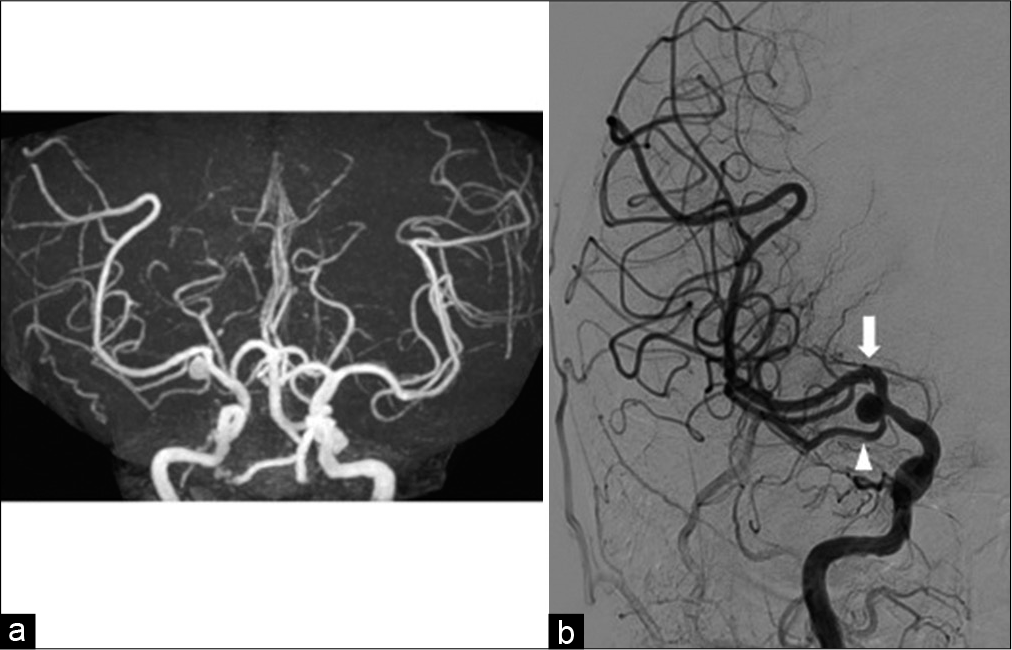
Magnetic resonance angiography revealed an aneurysm located near the top of the right internal carotid artery (ICA) between two middle cerebral arteries (MCAs) [
Figure 1:
(a) Magnetic resonance angiography revealing the aneurysm located near the top of the right internal carotid artery (ICA) between two middle cerebral arteries (MCAs). (b) Cerebral angiography demonstrating two MCAs originating from the top of the right ICA and revealing a 6-mm-sized aneurysm located between these two MCAs. These MCAs appeared to be the “true” MCA (arrow) and duplicated MCA (arrowhead). The ipsilateral A1 segment of the anterior cerebral artery was not visualized due to hypoplasia.
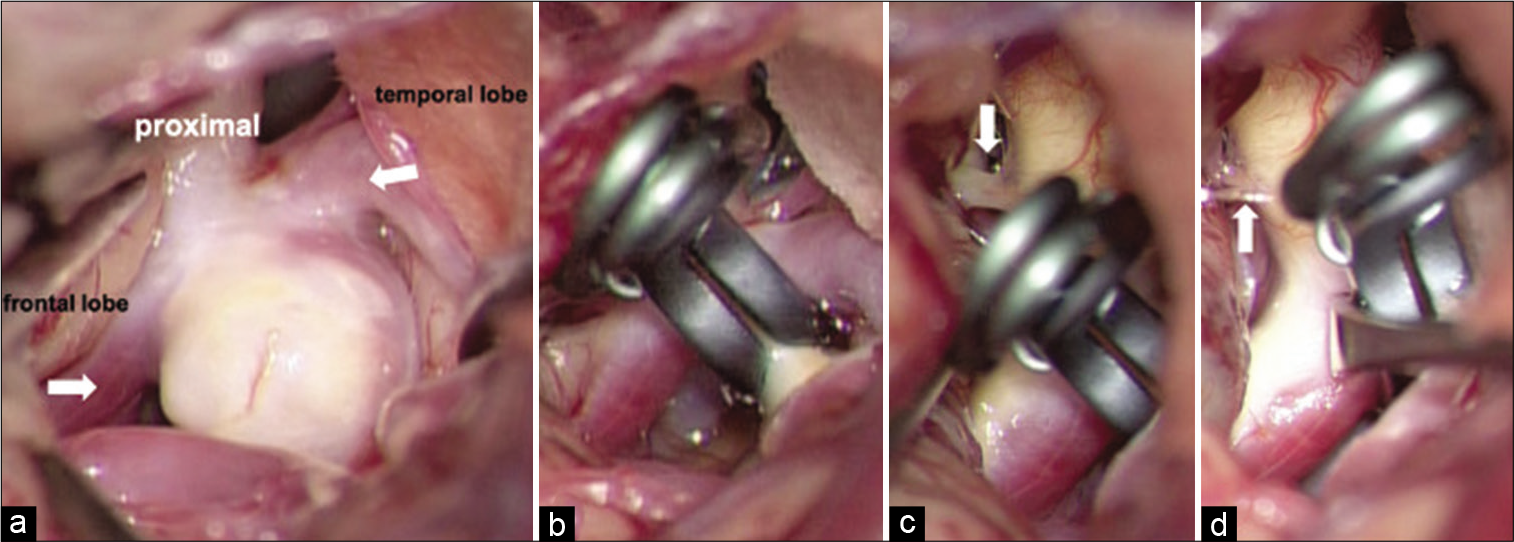
Surgical clipping of the aneurysm was performed through a transsylvian approach. The aneurysm was observed at the bifurcation of the two MCAs [
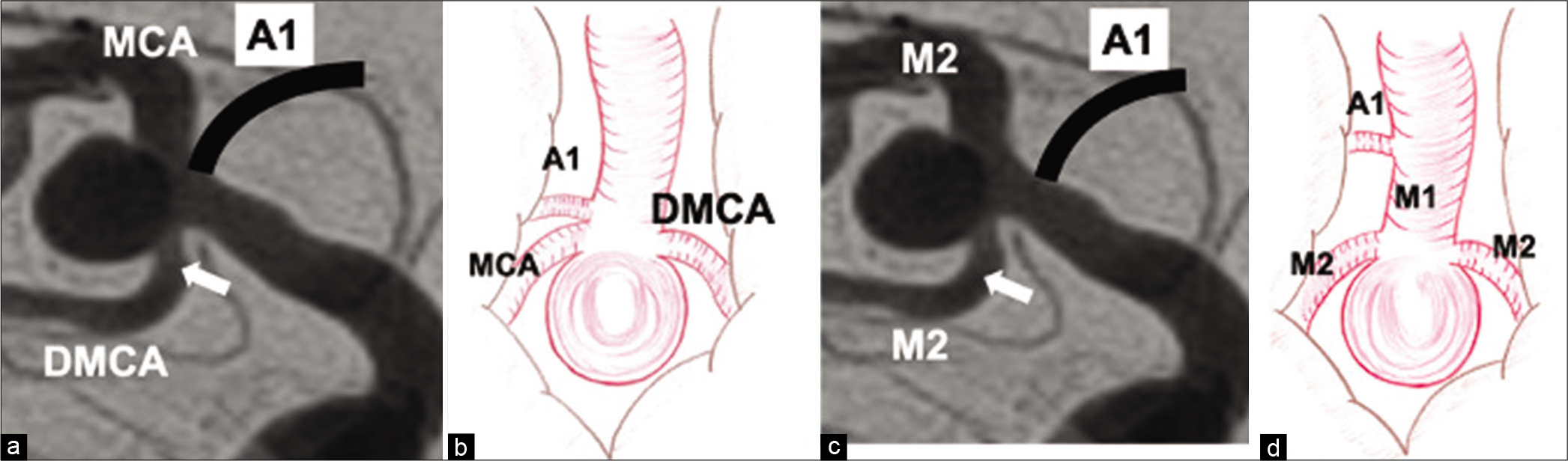
In the present case, based on the preoperative neuroimaging findings, the aneurysm was assumed to be located at the bifurcation of MCA and DMCA. However, during the surgery, the hypoplastic A1 segment, which was not visualized by angiography, was observed at approximately 2 mm proximal to the bifurcation of the MCAs. Thus, a very short prebifurcation segment of M1 segment of MCA existed on the distal side of the site, where the ICA branched into the ACA. Such an M1 with a length of 2–3 mm might be named super short M1. Considering these anatomical findings, these two MCAs were not “true” MCA and DMCA, but rather two normal MCA trunks that bifurcated from the super short prebifurcation segment of M1. This difference in interpretation was due to the fact that the hypoplastic A1 segment was not visualized on preoperative examinations. In cases wherein the position of the “second” MCA branches at the same as or proximal to the position where the ACA branches, the “second” MCA can be referred to as DMCA [
Figure 3:
When the position of the “second” middle cerebral artery (MCA) (arrow) branches at the same as or proximal to the position where the A1 segment of the anterior cerebral artery branches, the second MCA can be called duplicated MCA (a and b). When it (arrow) branches distal to where the A1 branches, it means that the M2 trunk originates from the prebifurcation segment of M1 (c and d).
The frequency with which ipsilateral ACA is not imaged by internal carotid angiography has been reported to be 1.3%.[
In conclusion, the present case suggests that the distinction between the DMCA and MCA trunks from the super short M1 is difficult, especially when the ipsilateral A1 is hypoplastic. Therefore, it is necessary to confirm the anatomy during aneurysm surgery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We would like to thank Enago (www.enago.jp) for English language editing.
References
1. Fujimoto K, Hashimoto H, Uchiyama Y, Maekawa H, Shida Y, Nakagawa I. Duplicated middle cerebral artery aneurysms treated by coil embolization: A report of two cases and literature review. J Stroke Cerebrovasc Dis. 2021. 30: 105773
2. Gibo H, Carver CC, Rhoton AL, Lenkey C, Mitchell RJ. Microsurgical anatomy of the middle cerebral artery. J Neurosurg. 1981. 54: 151-69
3. Heros RC, Fritsch MJ. Surgical management of middle cerebral artery aneurysm. Neurosurgery. 2001. 48: 780-5
4. Iida Y, Tamase A, Kamide T, Mori K, Seki S, Nomura M. Aneurysm at origin of duplicated middle cerebral artery associated with another aneurysm. Surg Neruol Int. 2015. 6: S549-52
5. Komiyama M, Nakajima H, Nishikawa M, Yasui T. Middle cerebral artery variations: Duplicated and accessory arteries. AJNR Am J Neuroradiol. 1998. 19: 45-9
6. Krayenbuhl HA, Yasargil MG.editors. Cerebral Angiography. London: Butterworths; 1968. p.
7. Nomura M, Yamashima T, Kita D, Kida S, Kajinami K, Yamashita J. Duplication of the middle cerebral artery associated with an unruptured aneurysm. Acta Neurochir (Wien). 2000. 142: 221-2
8. Teal JS, Rumbaugh CL, Bergeron RT, Segall HD. Anomalies of the middle cerebral artery: Accessory artery, duplication, and early bifurcation. Am J Roentgenol Radium Ther Nucl Med. 1973. 118: 567-75
9. Toyota S, Kumagai T, Sugano H, Yamamoto S, Mori K, Taki T. Unruptured aneurysm at the origin of the duplicated middle cerebral artery treated by coil embolization: A case report. Open J Mod Neurosurg. 2015. 5: 27-33