- Department of Neurosurgery, Tokuda Neurosurgical Hospital, Kanoya, Kagoshima, Japan.
DOI:10.25259/SNI_612_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hirotaka Inoue, Akihito Hashiguchi, Koichi Moroki, Hajime Tokuda. Unruptured internal carotid-posterior communicating artery aneurysm splitting the oculomotor nerve: A case report and literature review. 21-Oct-2020;11:353
How to cite this URL: Hirotaka Inoue, Akihito Hashiguchi, Koichi Moroki, Hajime Tokuda. Unruptured internal carotid-posterior communicating artery aneurysm splitting the oculomotor nerve: A case report and literature review. 21-Oct-2020;11:353. Available from: https://surgicalneurologyint.com/surgicalint-articles/10342/
Abstract
Background: Although it is well known that internal carotid-posterior communicating artery (ICA-PcomA) aneurysms compress the oculomotor nerve and cause nerve palsy, cases of ICA-PcomA aneurysms splitting the oculomotor nerve are extremely rare.
Case Description: We present the rare case of an asymptomatic, growing, left-sided ICA-PcomA aneurysm that was confirmed to split the oculomotor nerve. We report the clinical course and discuss the underlying mechanism. The oculomotor nerve, which is an aggregate of multiple fibers, exhibits age-related loss of compactness in the arrangement of its nerve fibers.
Conclusion: We speculate that injury to the nerve fibers by aneurysmal compression was avoided because of the rare phenomenon of splitting of the oculomotor nerve.
Keywords: Clipping, Internal carotid-posterior communicating artery aneurysm, Nerve fibers, Oculomotor nerve, Splitting
INTRODUCTION
It is well known that internal carotid-posterior communicating artery (ICA-PcomA) aneurysms compress the oculomotor nerve and cause nerve palsy, which is one of the important clinical signs of an ICA-PcomA aneurysm.[
CASE REPORT
The patient was a 78-year-old woman who first presented with a mild decrease in cognitive function at the age of 75 years. She did not exhibit signs of neurological deficits such as anisocoria or diplopia. However, magnetic resonance imaging revealed a left-sided ICA-PcomA aneurysm. Three-dimensional computed tomography (CT) angiography revealed an irregularly shaped aneurysm measuring 7 mm [
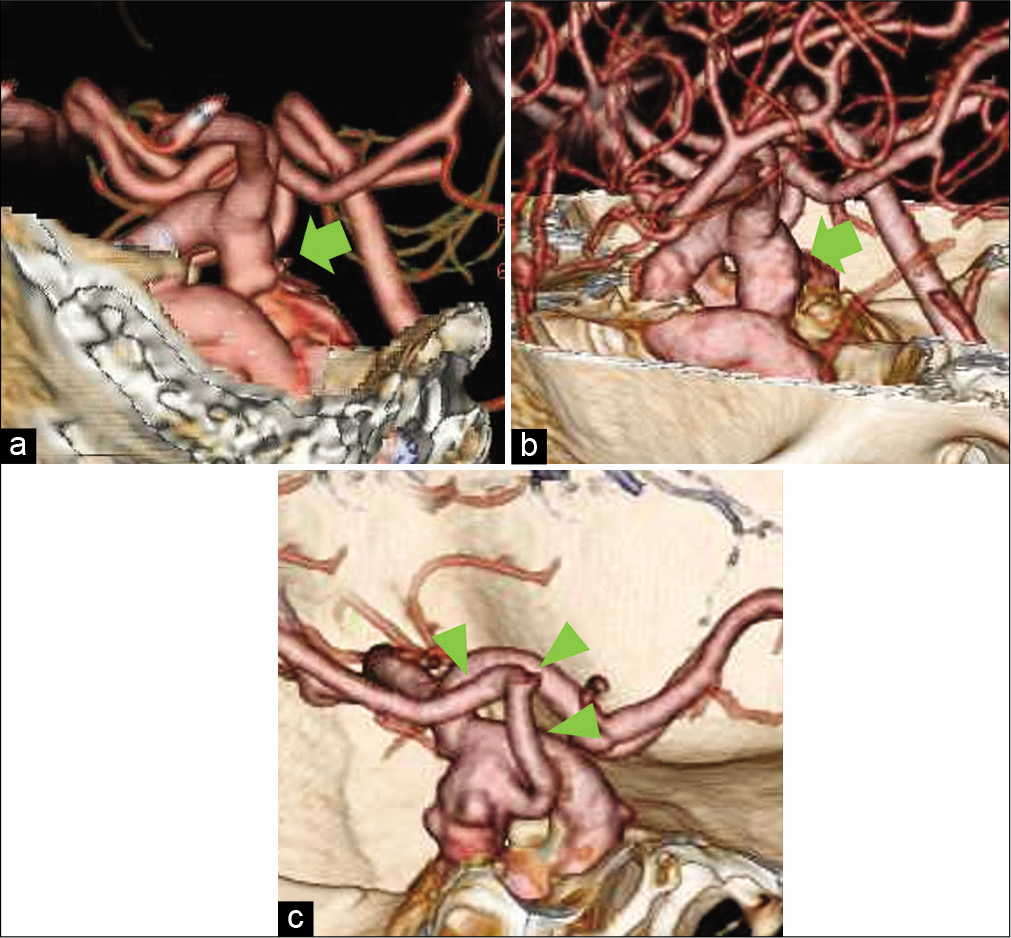
Figure 1:
(a) Three-dimensional CT angiography showing the aneurysm (7 mm, arrow) when the patient was 75 years old. The aneurysm originated from the distal side of the bifurcation of the left internal carotid artery and posterior communicating artery. (b) The aneurysm enlarged to 10 mm at the age of 78 years (arrow). (c) CT showing the posterior communicating artery appearing to arise from the aneurysmal body (arrow heads)
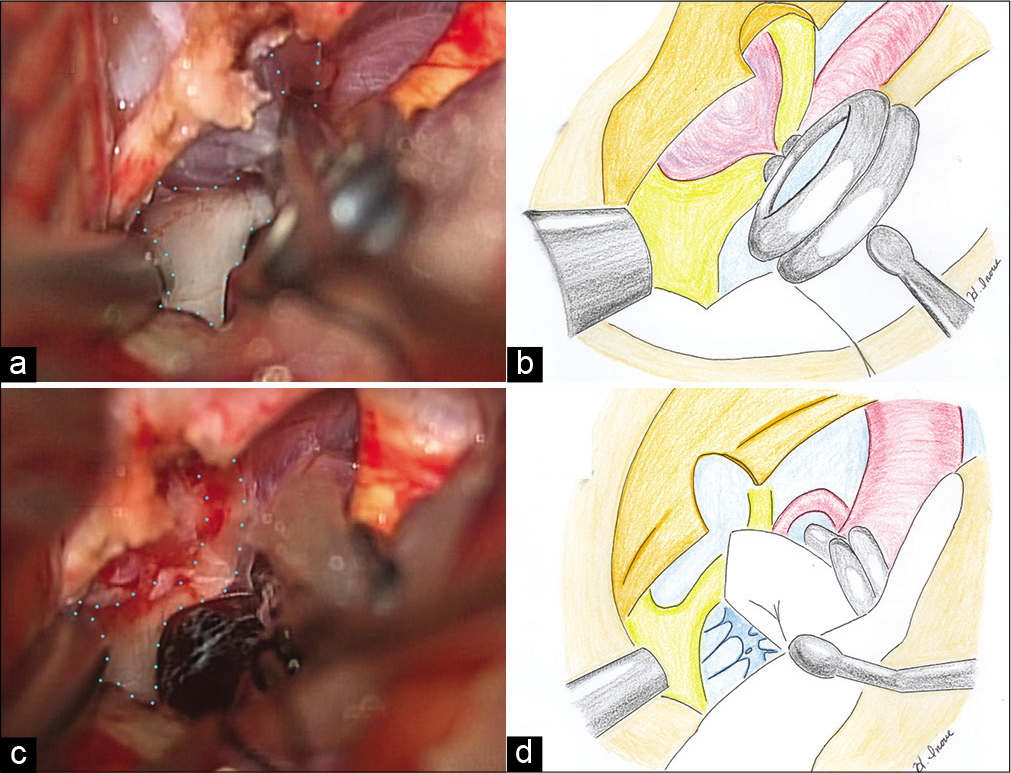
Figure 2:
(a) Intraoperative photograph of the left pterional approach. Splitting of the oculomotor nerve by the aneurysm (dotted line). (b) Schematic illustration depicting the aneurysm splitting the oculomotor nerve. (c) The aneurysm is resected. (d) Schematic illustration of the resected aneurysm.
The patient provided written informed consent for the publication of this report.
DISCUSSION
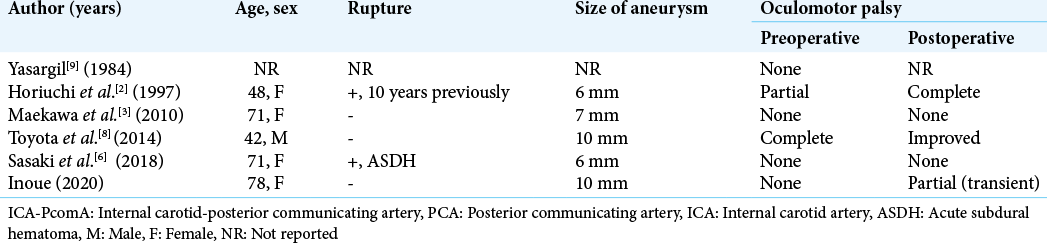
Oculomotor nerve palsy is a well-known and important clinical sign of growing ICA-PcomA aneurysms. Thinning of the oculomotor nerve due to aneurysmal compression is often observed during direct clipping. The oculomotor nerve is susceptible to compression by the ICA-PcomA just before it enters the cavernous sinus, which has low mobility.[
CONCLUSION
We reported the unique case of an unruptured left-sided ICA-PcomA aneurysm splitting the oculomotor nerve. Oculomotor palsy was not observed preoperatively in this patient. We speculated that nerve fiber injury by aneurysmal compression may have been avoided, because the oculomotor nerve was split (before the aneurysm could have caused compressive injury).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos available on:
www.surgicalneurologyint.com
References
1. Cahill M, Bannigan J, Eustace P. Anatomy of the extraneural blood supply to the intracranial oculomotor nerve. Br J Ophthalmol. 1996. 80: 177-81
2. Horiuchi T, Kyoshima K, Oya F, Kobayashi S. Fenestrated oculomotor nerve caused by internal carotid-posterior communicating artery aneurysm: Case report. Neurosurgery. 1997. 40: 397-8
3. Maekawa H, Hadeishi H, Tanaka M. Unruptured internal carotid-posterior communicating artery aneurysm splitting the oculomotor nerve: Case report. J Stroke. 2010. 32: 163-6
4. Park HK, Rha HK, Lee KJ, Chough CK, Joo W. Microsurgical anatomy of the oculomotor nerve. Clin Anat. 2017. 30: 21-31
5. Rhoton AL Jr. Aneurysms. Neurosurgery. 2002. 51: S121-58
6. Sasaki R, Motoyama Y, Nakagawa I, Park YS, Nakase H. Asymptomatic penetration of oculomotor nerve by internal carotid-posterior communicating artery aneurysm presenting pure acute subdural hematoma: A case report. Neurol Med Chir (Tokyo). 2018. 58: 173-7
7. Sharma S, Ray B, Bhardwaj D, Dwivedi AK, Roy TS. Age changes in the human oculomotor nerve-a stereological study. Ann Anat. 2009. 191: 260-6
8. Toyota S, Taki T, Wakayama A, Yoshimine T. Unruptured internal carotid-posterior communicating artery aneurysm splitting the oculomotor nerve: A case report and literature review. J Neurol Surg Rep. 2014. 75: e180-2
9. Yasargil MG.editors. Internal carotid artery aneurysms. Microneurosurgery. Stuttgart, Germany: Thieme; 1984. 2: 76-7