- Department of Neurosurgery, General Hospital of Fortaleza, Fortaleza, Brazil.
- Department of Otorhinolaryngology, Leonardo da Vinci Hospital, Fortaleza, Brazil.
- Department of Medicine, Ceara State University, Fortaleza, Brazil.
Correspondence Address:
Tiago S. F. Holanda, Department of Neurosurgery, General Hospital of Fortaleza, Fortaleza, Brazil.
DOI:10.25259/SNI_979_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Tiago S. F. Holanda1, Isnara Mara Freitas Pimentel2, Paulo Victor Ferreira Gomes Araujo1, José Ítalo da Silva Damasceno Gomes3, Vinícius Chagas de Morais Moreira3, Tito Bastos Siqueira Soares3, Lucas Alverne Freitas de Albuquerque1. Unusual bifrontal cerebral infarction related to pituitary apoplexy. An uncommon presentation and literature review. 09-Dec-2022;13:577
How to cite this URL: Tiago S. F. Holanda1, Isnara Mara Freitas Pimentel2, Paulo Victor Ferreira Gomes Araujo1, José Ítalo da Silva Damasceno Gomes3, Vinícius Chagas de Morais Moreira3, Tito Bastos Siqueira Soares3, Lucas Alverne Freitas de Albuquerque1. Unusual bifrontal cerebral infarction related to pituitary apoplexy. An uncommon presentation and literature review. 09-Dec-2022;13:577. Available from: https://surgicalneurologyint.com/surgicalint-articles/12047/
Abstract
Background: Pituitary apoplexy (PA) is a syndromic condition described in 1950. The main symptoms are headache, visual impairment, ophthalmoplegia, and hypopituitarism. The relationship between stroke and PA is uncommon and two mechanisms are described: vascular compression and vasospasm.
Case Report: A 65-old-year man presented with severe headache, vomiting, ophthalmoplegia, and somnolence. Radiological examinations showed an expansive sellar and suprasellar lesion with a heterogeneous signal, besides Diffusion-weighted imaging (DWI) restriction in the bifrontal area was present. The findings were compatible with PA and stroke.
Conclusion: PA leading to cerebral infarction is a rare condition that presents high morbidity and mortality levels. There are two main mechanisms related: direct arterial compression and arterial vasospasm. The cases must be conducted as neuroendocrinological emergencies and surgical management is a key point to better the prognosis of patients.
Keywords: Anterior cerebral artery, Neuroendoscopy, Skull base, Stroke, Pituitary apoplexy
INTRODUCTION
Pituitary apoplexy (PA) is a syndromic condition characterized by the sudden onset of symptoms.[
The main symptoms are severe headache, visual impairment, nausea, ophthalmoplegia, hypopituitarism, and altered mental status including coma.[
Despite ischemic stroke being a common cause of disability, the relationship with PA is rare with few cases reported in the literature.[
Only a few cases of bifrontal infarction related to PA were reported. Inside these manuscripts, only five patients with both anterior cerebral arteries stroke.[
CASE REPORT
A previous hypertense 65-old-year man was admitted to the emergency department of our institution with a history of severe headache, vomiting, and somnolence that started 5 days before admission. Associated with these symptoms, a progressive visual impairment and a comma occurred.
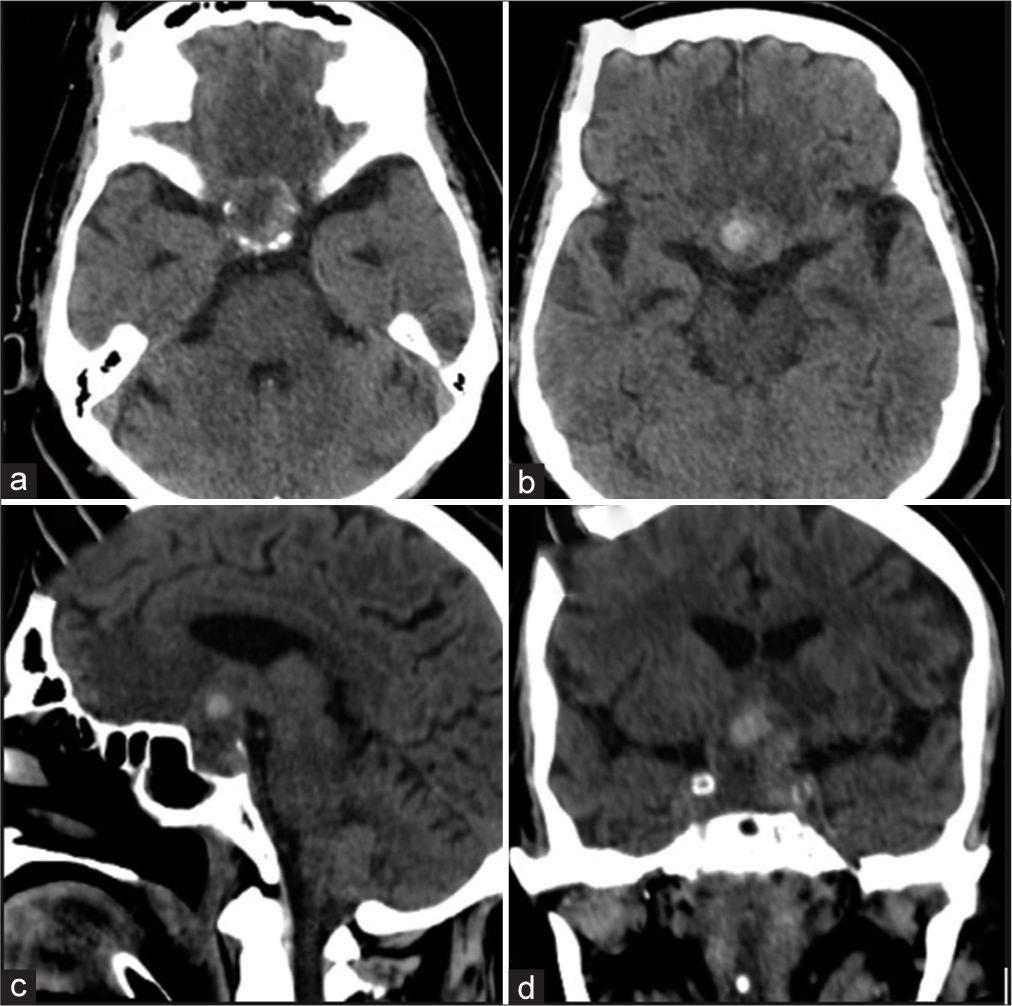
The patient presented anisocoria (with the left mydriasis) and divergent squint on clinical examination. Bradycardia and hypotension were continuous and the use of dopamine was necessary. An emergency CT scan was performed which showed a sellar and suprasellar hemorrhagic expansive lesion associated with a bifrontal hypodensity area [
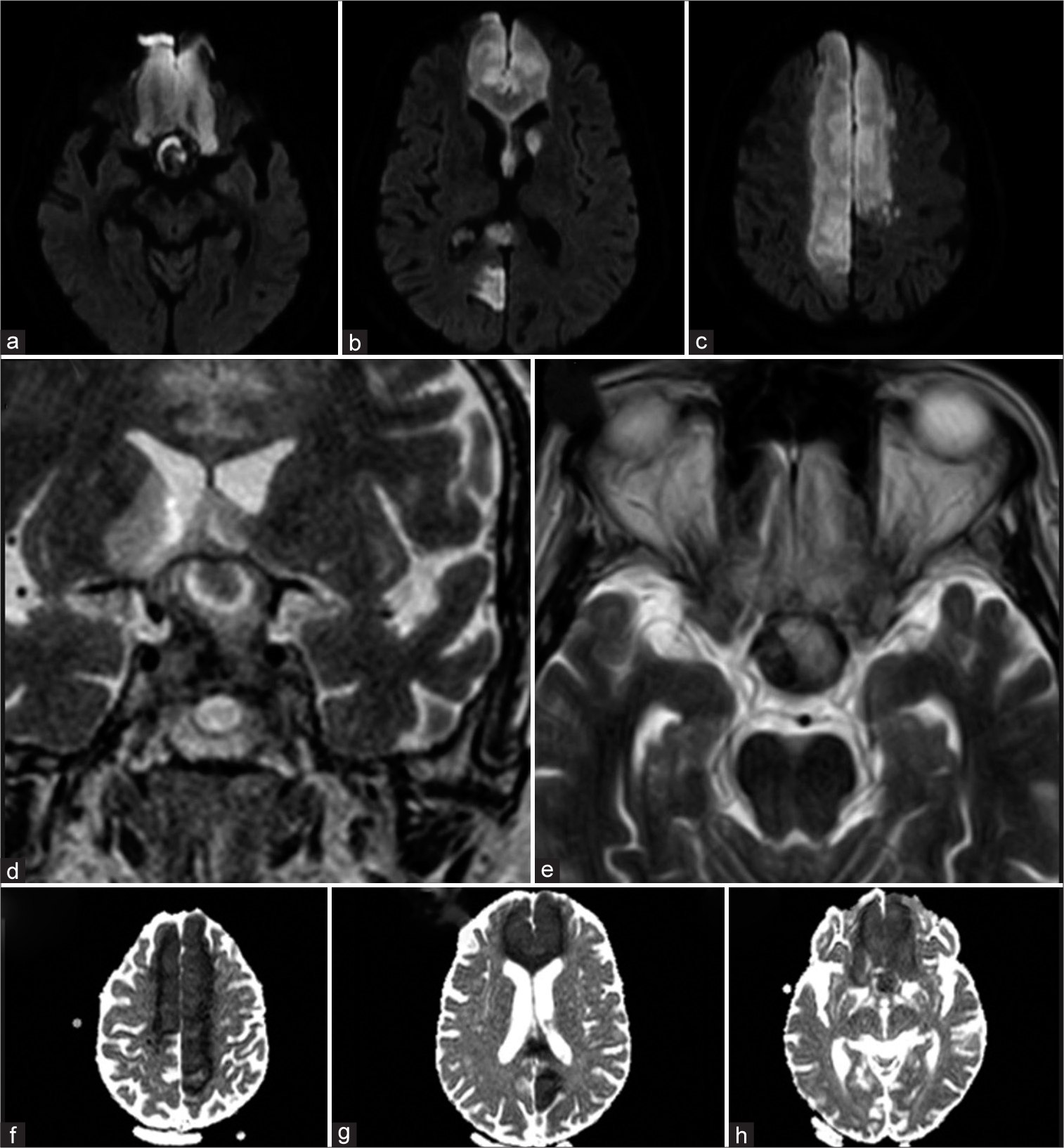
MRI showed a large sella turcica with an expansive sellar and suprasellar lesion with a heterogeneous signal. The lesion’s size was 3.1 × 3.0 × 1.5 cm and compression of the optic chiasm and anterior cerebral arteries was observed bilaterally. Besides the lesion, DWI restriction in the bifrontal area was present. These findings were consistent with PA and bifrontal ischemia [
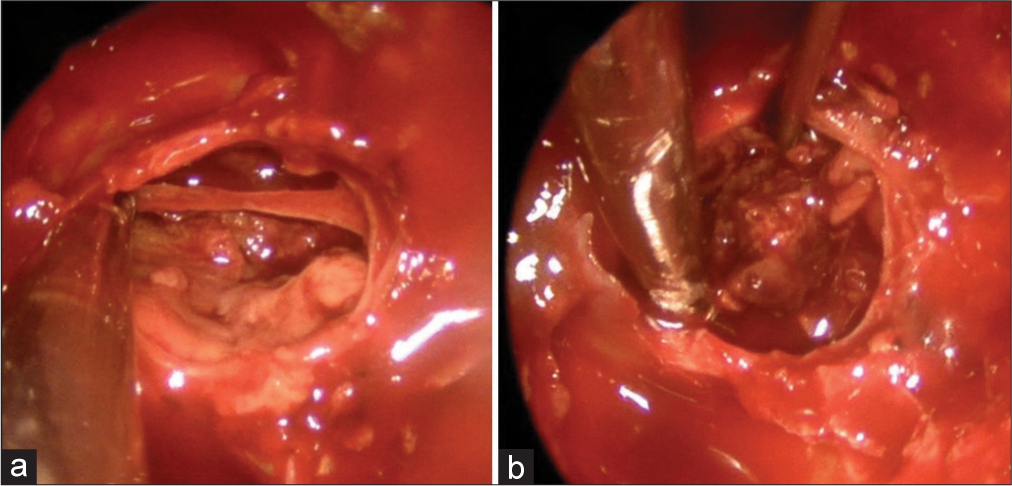
The endocrinological evaluation showed hypopituitarism and was necessary to start hormone replacement therapy with levothyroxine and prednisone. Because of the emergency, the patient was submitted to an endoscopic transnasal transsphenoidal approach. During the surgery, a red color lesion with a hemorrhagic area was observed inside it. After tumor removal, observed decompression of optic chiasm with arachnoid fall of the suprasellar cistern [
After surgery, the cardiac output improved, without the need for vasoactive drugs as in the preoperative period. The patient had a regular recovery with isochoric pupils and slowed but continuous alertness. Apathy was diagnosed and related to the ischemic area.
DISCUSSION
Brougham et al. described in 1950 a condition related to inexplicable deaths which had presented sudden severe headaches, visual impairment, and coma.[
PA is an atypical condition. The incidence varies from 2% to 10% of all pituitary adenomas/pituitary neuroendocrinological tumor (PITNET).[
The characteristics syndrome is sudden often severe headache, visual impairment, cranial nerve paresis with ophthalmoplegia, hypopituitarism, and mental status involvement including coma. Physiopathology is multifactorial; however, the low blood input, size of the tumor, and internal pressure are directly involved. Neurosurgical treatment is necessary and emergencies.[
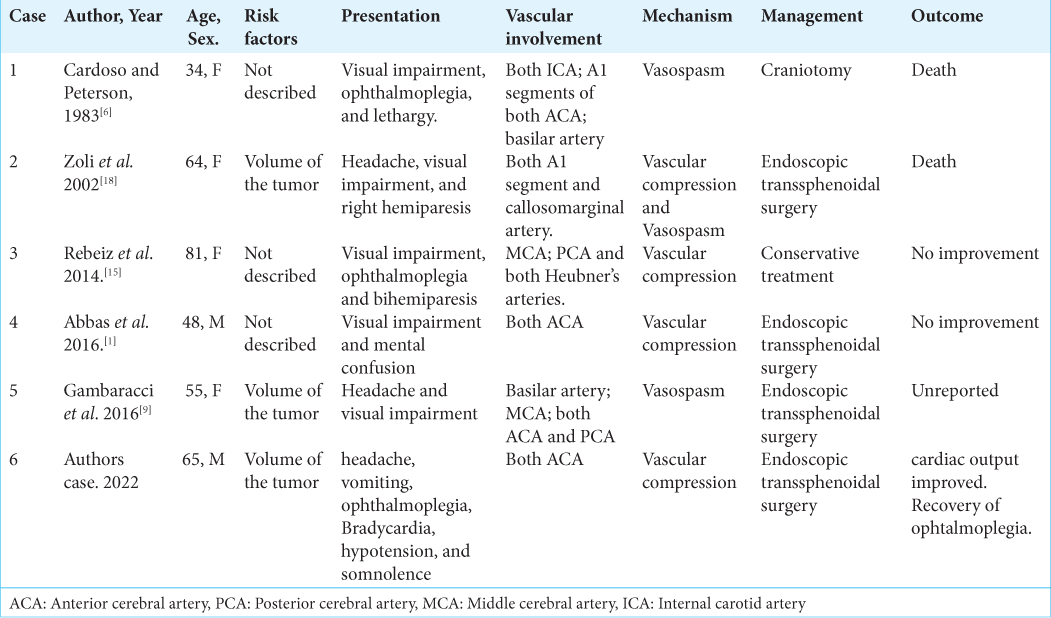
Ischemic infarction related to PA is uncommon in the literature. Few cases were reported, the first manuscript was published in 1952 with a 62-year-old man who presented the left hemiparesis because of the direct compression of the right middle cerebral artery (MCA). Since then, only five cases of bilateral anterior cerebral arteries stroke were reported [
There are two main mechanisms studied that are related to these both conditions. Directly arterial compression and arterial vasospasm could participate alone or mismatch. The vasospasm can be a response to subarachnoid hemorrhage.[
Because the PA is the initial cause, the above PA syndrome could be present, nevertheless, other major symptoms and signs were described as hemiparesis/hemiplegia, facial paresis, dysarthria, and other focal neurological deficits; however, all these presentations are unspecific because depends on the arterial specific area, but internal carotid artery is more commonly affected with 58.7% of cases, keep by anterior cerebral artery (ACA) (32.6%) and MCA (25%). The basilar artery was reported only in three cases.[
Radiologic examinations are necessary to take sure of the diagnosis. CT scan and MRI are the initial choices. A vascular search is necessary and could be realized for MRI, CT angiography, or conventional angiography. In general, the stroke occurs unilaterally.[
However, the medical staff must remember that ischemic stroke has more common mechanisms. The initial research about stroke causes must be realized with the current investigation. With the relationship between PA and ischemic infarction confirmed, the treatment must be applied.[
Because the cause is PA, neurosurgical emergency surgery is mandatory. Surgery must be performed early. When associated with a stroke, the maximum time to perform it is a factor not yet defined, but early intervention modifies morbidity and mortality.
During previous reports, the clinical management had present 50–75% of mortality.[
Despite the better outcomes, surgical treatment could lead to a hemorrhagic transformation of stroke.[
Postoperative management is important because transient or permanent endocrinological dysfunctions could be present. The principal complication is adrenal insufficiency.
Because of this complication, low vascular pressure could lead to worsening cerebral perfusion and a higher infarction area. Other possible complications are insipidus diabetes and hypopituitarism, so a trained team of neurosurgeons, endocrinologists, otorhinolaryngologists, anesthesiologists, and critical care team should be prepared and could change the natural history of these complications.[
Since 1952, few cases were reported; however, only five cases with both anterior cerebral artery (ACA) ischemic infarctions are shown in [
CONCLUSION
PA leading to cerebral infarction is a rare condition that presents high morbidity and mortality levels. There are two main mechanisms related: direct arterial compression and arterial vasospasm. The syndrome presentation is a mismatch between PA symptoms and stroke.
The cases must be conducted as neuroendocrinological emergencies and surgical management is a key point to better the prognosis of patients. The postoperative period is also important because of complications related to hypopituitarism that need adequate control to reduce the impact on prognosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Abbas MS, AlBerawi MN, Bozom IA, Shaikh NF, Salem KY. Unusual complication of pituitary macroadenoma: A case report and review. Am J Case Rep. 2016. 17: 707-11
2. Ahn JM, Oh HJ, Oh JS, Yoon SM. Pituitary apoplexy causing acute ischemic stroke: Which treatment should be given priority. Surg Neurol Int. 2020. 11: 113
3. Barnejee C, Snelling B, Hanft S, Kotomar RJ. Bilateral cerebral infarction in the setting of pituitary apoplexy: A case presentation and literature review. Pituitary. 2014. 18: 352-8
4. Bettag C, Strasilla C, Steinbrecher A, Gerlach R. Unilateral tuberothalamic artery ischemia caused by pituitary apoplexy. J Neurol Surg A Cent Eur Neurosurg. 2018. 79: 550-4
5. Brougham M, Heusner P, Adams RD. Acute degenerative changes in adenomas of the pituitary body-with special reference to pituitary apoplexy. J Neurosurg. 1950. 7: 421-39
6. Cardoso ER, Peterson EW. Pituitary apoplexy and vasospasm. Surg Neurol. 1983. 20: 391-5
7. Chokyu I, Tsuyuguchi N, Goto T, Chokyu K, Chokyu M, Ohata K. Pituitary apoplexy causing internal carotid artery occlusion-case report. Neurol Med Chir. 2011. 51: 48-51
8. Erlajani T, Chen S, Cajigas I, Saway B, Sur S, Morcos JJ. Pituitary apoplexy and cerebral infarction: Case report and literature review. World Neurosurg. 2020. 141: 73-80
9. Gambaracci G, Rondoni V, Guercini G, Floridi P. Pituitary apoplexy complicated by vasospasm and bilateral cerebral infarction. Br Med J Case Rep. 2016. 2016: bcr2016216186
10. Garcia RS, Amo JM, Pena PR, Buezas LP, Gómez LG, Allut AG. Stroke secundary Pituitary Apoplexy: Case report and literature review. Neurocirugía. 2016. 27: 310-4
11. Jiang Q, Xiao S, Shu L, Huang X, Chen X, Hong H. Pituitary apoplexy leading to cerebral infarction: A systematic review. Eur Neurol. 2020. 83: 121-30
12. Pasha SA, Ranganthan LN, Setty VK, Reddy R, Ponnuru DA. Acute ischemic stroke as a manifestation of a pituitary apoplexy in a young lady. J Clin Diagn Res. 2017. 11: OD03-5
13. Pokhrel B, Khanal S, Chapagain P, Sedain G. Pituitary apoplexy complicated by cerebral infarction: A case report. J Nepal Med Assoc. 2021. 59: 723-6
14. Pozzati E, Frank G, Nasi MT, Giuliani G. Pituitary apoplexy, bilateral carotid vasospasm, and cerebral infarction in a 15-year-old boy. Neurosurgery. 1987. 20: 56-9
15. Rebeiz T, Cueva W, Ardelt A. Unusual case of bilateral caudate infarcts following pituitary apoplexy. JAMA Neurol. 2014. 71: 226-7
16. Sussman ES, Ho AL, Pendharkar AV, Achrol AS, Harsh GR 4th. Pituitary apoplexy associated with carotid compression and large ischemic penumbra. World Neurosurg. 2016. 92: 581-7
17. Zhangi C, Feng F, Zhu Y, Wang R, Xing B. Cerebral infarction caused by pituitary apoplexy: Case report and literature review. Turk Neurosurg. 2014. 24: 782-7
18. Zoli M, Guaraldi F, Rustici A, Cirillo L, Asioli S, Mazzatenta D. Bilateral anterior circulation stroke: A rare but threatening consequence of pituitary apoplexy. Case report and systematic literature review. Neuroradiol J. 2022. 22: 1-6
19. Zou Z, Liu C, Sun B, Chen C, Xiong W, Che W. Surgical treatment of pituitary apoplexy in association with hemispheric infarction. J Clin Neurosci. 2015. 22: 1550-4