- Department of Neurosurgery, Clinical Neurosciences Center, University of Utah, Salt Lake City, Utah 84132, USA
- Department of Radiology, University of Utah, Salt Lake City, Utah 84132, USA
Correspondence Address:
Andrew T. Dailey
Department of Neurosurgery, Clinical Neurosciences Center, University of Utah, Salt Lake City, Utah 84132, USA
DOI:10.4103/2152-7806.174889
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Krisht KM, Karsy M, Shah LM, Schmidt MH, Dailey AT. Unusual brachial plexus lesion: Hematoma masquerading as a peripheral nerve sheath tumor. Surg Neurol Int 25-Jan-2016;7:
How to cite this URL: Krisht KM, Karsy M, Shah LM, Schmidt MH, Dailey AT. Unusual brachial plexus lesion: Hematoma masquerading as a peripheral nerve sheath tumor. Surg Neurol Int 25-Jan-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/unusual-brachial-plexus-lesion-hematoma-masquerading-as-a-peripheral-nerve-sheath-tumor/
Abstract
Background:Malignant peripheral nerve sheath tumors (MPNSTs) of the brachial plexus have unique radiographic and clinical findings. Patients often present with progressive upper extremity paresthesias, weakness, and pain. On magnetic resonance (MR) imaging, lesions are isointense on T1-weighted and hyperintense on T2-weighted sequences, while also demonstrating marked enhancement on MR studies with gadolinium diethylenetriamine pentaacetic acid. On the basis of their characteristic MR imaging features and rapid clinical progression, two brachial plexus lesions proved to be organizing hematomas rather than MPNST.
Methods:A 51-year-old male and a 31-year-old female were both assessed for persistent and worsened left-sided upper extremity pain, paresthesias, and weakness. In both cases, the MR imaging of the brachial plexus demonstrated an extraspinal enhancing lesion located within the left C7–T1 neuroforamina.
Results:Although the clinical and radiographic MR features for these 2 patients were consistent with MPNSTs, both lesions proved to be benign organizing hematomas.
Conclusions:These two case studies emphasize that brachial plexus hematomas may mimic MPNSTs on MR studies. Accurate diagnosis of these lesions is critical for determining the appropriate management options and treatment plans. Delaying the treatment of a highly aggressive nerve sheath tumor can have devastating consequences, whereas many hematomas resolve without surgery. Therefore, if the patient has stable findings on neurological examination and a history of trauma, surgical intervention may be delayed in favor of repeat MR imaging in 2–3 months to re-evaluate the size of the mass.
Keywords: Brachial plexus, hematoma, malignant peripheral nerve sheath tumor, nerve sheath tumor, schwannoma
INTRODUCTION
Malignant peripheral nerve sheath tumors (MPNSTs) carry a poor prognosis; the 5-year survival rates of 16–50% (e.g., depending on neurofibromin 1 [NF1] status) necessitate rapid diagnosis and treatment.[
CLINICAL PRESENTATION
Case 1
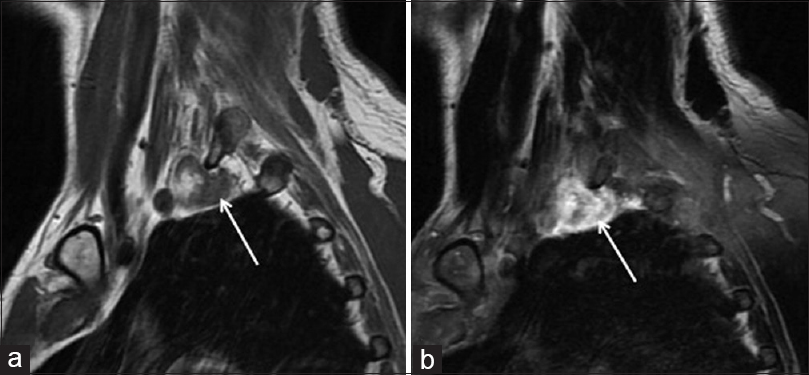
A 51-year-old male presented with several months of progressively worsening left arm and clavicle pain, accompanied by hyperesthesias (e.g., from the third digit laterally to the axilla), and diffuse 3-4/5 weakness. Four months prior to his presentation, he had fallen off a ladder and had hung suspended from his left arm. At that time, he had received a selective left C8 nerve root and interlaminar steroid injection for pain relief. MR imaging of his left posterior brachial plexus demonstrated a T1-weighted, heterogeneously enhancing, well-circumscribed lesion suggestive of a MPNST [
Case 2
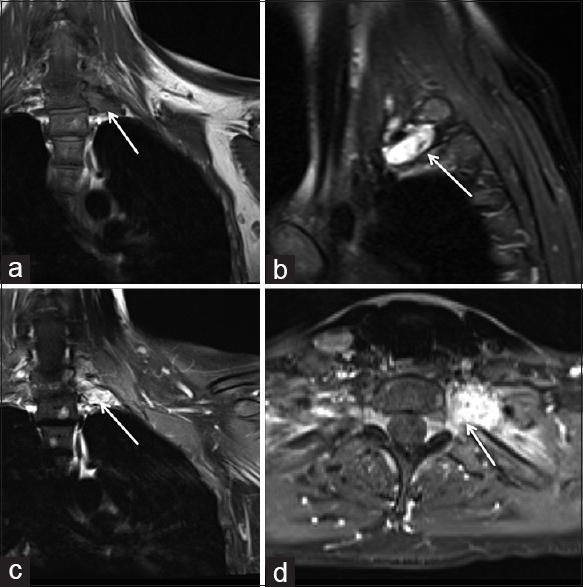
A 31-year-old female presented with a 3-month history, following a motor vehicle accident, of persistent pain along the left medial elbow, accompanied by tingling and numbness in her left fourth and fifth digits and left hand abduction weakness. The neurological findings were suggestive of a C8/T1 radiculopathy or a brachial plexopathy. The brachial plexus MR imaging demonstrated a T1 hypointense, T2 hyperintense, and markedly enhancing soft tissue mass on the T1/gadolinium diethylenetriamine pentaacetic acid study within and beyond the left C7/T1 and T1/T2 neuroforamina. The immediate concern was for a MPNST [
DISCUSSION
Differential diagnosis of benign brachial plexus schwannoma or neurofibroma
Brachial plexus lesions are most commonly benign schwannomas or neurofibromas and only more rarely MPNSTs. Benign schwannomas and neurofibromas commonly show T2 hyperintensity and T1 isointensity; schwannomas grow at the periphery of nerves, while neurofibromas grow within the neural tissue and entrap nerve fibers. In addition, schwannomas are frequently encapsulated, showing a rim of low intensity along the tumor margin, while neurofibromas are not.[
Concern for malignant peripheral nerve sheath tumors
In a large series by Wasa et al.[
Large brachial plexus tumor series
In the largest brachial plexus tumor series published to date, involving 111 tumors in 107 patients, the most common presenting symptoms were numbness/paresthesias, pain, weakness, and a palpable mass.[
Evolving T1 and T2 magnetic resonance images of brachial plexus hematoma
The T2- and T1-weighted MR imaging characteristics typical of nerve sheath tumors may also be characteristic of evolving hematomas. During the acute stage, a hematoma is isointense relative to the spinal cord on T1-weighted images and hyperintense relative to the spinal cord on T2-weighted images. In the subacute stage, approximately 30 h after the initial hemorrhage, the hematoma usually has a heterogenous hyperintensity on both T1- and T2-weighted images attributed to the degradation products of hemoglobin. In addition, neovascularization of the granulation tissue within the organized chronic hematoma accounts for the uptake of gadolinium; however, this tends to occur peripherally unlike the homogenous enhancement seen in our cases. This latter feature, along with the clinical scenario, makes the diagnosis of hematoma less likely versus a MPNST. Conversely, two cases of soft tissue sarcomas initially mimicked large hematomas.[
CONCLUSION
Brachial plexus hematomas are rare and can mimic MPNSTs both radiographically and clinically. Careful probing into the patient's history, including recent traumatic events, history of NF, and intake of antithrombotic medications, may help shed light on whether these lesions are benign hematomas or MPNSTs.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We thank Gregory Jost, MD, for assistance with this case and Kristin Kraus, MSc, for editorial help.
References
1. Ducatman BS, Scheithauer BW, Piepgras DG, Reiman HM, Ilstrup DM. Malignant peripheral nerve sheath tumors. A clinicopathologic study of 120 cases. Cancer. 1986. 57: 2006-21
2. Enzinger F, Weiss S.editors. Soft Tissue Tumors. St. Louis, MO: CV Mosby; 1983. p.
3. Ganju A, Roosen N, Kline DG, Tiel RL. Outcomes in a consecutive series of 111 surgically treated plexal tumors: A review of the experience at the Louisiana State University Health Sciences Center. J Neurosurg. 2001. 95: 51-60
4. Niimi R, Matsumine A, Kusuzaki K, Okamura A, Matsubara T, Uchida A. Soft-tissue sarcoma mimicking large haematoma: A report of two cases and review of the literature. J Orthop Surg (Hong Kong). 2006. 14: 90-5
5. Wasa J, Nishida Y, Tsukushi S, Shido Y, Sugiura H, Nakashima H. MRI features in the differentiation of malignant peripheral nerve sheath tumors and neurofibromas. AJR Am J Roentgenol. 2010. 194: 1568-74