- Departments of Neurosurgery, Nagasaki Medical Center, Omura, Nagasaki, Japan.
DOI:10.25259/SNI_216_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ichiro Kawahara, Eri Shiozaki, Kosuke Soejima, Yuka Ogawa, Yoichi Morofuji, Tomonori Ono, Wataru Haraguchi, Keisuke Tsutsumi. Unusual course of the vagus nerve passing anterior to the internal carotid artery during carotid endarterectomy. 14-Jun-2021;12:278
How to cite this URL: Ichiro Kawahara, Eri Shiozaki, Kosuke Soejima, Yuka Ogawa, Yoichi Morofuji, Tomonori Ono, Wataru Haraguchi, Keisuke Tsutsumi. Unusual course of the vagus nerve passing anterior to the internal carotid artery during carotid endarterectomy. 14-Jun-2021;12:278. Available from: https://surgicalneurologyint.com/surgicalint-articles/10889/
Abstract
Background: Carotid endarterectomy (CEA) is a conventional surgical technique to prevent ischemic stroke and the effectiveness for advanced lesions is established in many large studies. The vagus nerve is one of the cranial nerves that we usually encounter during CEA manipulation, which is identified as located posterior to the vessels in a position posterolateral to the carotid artery and posteromedial to the internal jugular vein.
Case Description: We experienced an extremely rare case of the vagus nerve passing anterior to the internal carotid artery during CEA.
Conclusion: We should be careful not to accidentally cut off because the variation of the vagus nerve can be mistaken for an ansa cervicalis. A delicate and complete dissection to understand the variation of the vagus nerve is crucial to minimize the risk of cranial nerve injury during CEA.
Keywords: Anterior course, Carotid endarterectomy, Internal carotid artery, Vagus nerve
INTRODUCTION
Carotid endarterectomy (CEA) is a conventional surgical technique to prevent ischemic stroke and the effectiveness for advanced lesions is established in many large studies. Complications following CEA involve stroke, myocardial infarction, death, and cranial nerve injury. It is important to understand the anatomy of the vessels and cranial nerves. The vagus nerve is one of the cranial nerves that we usually encounter during CEA manipulation, which is identified as located posterior to the vessels in a position posterolateral to the carotid artery and posteromedial to the internal jugular vein (IJV).[
We experienced an extremely rare case of the vagus nerve passing anterior to the internal carotid artery (ICA) during CEA.
CASE REPORT
A 74-year-old man, right-handed with hyperlipidemia had a carotid ultrasonography at a rural clinic and bilateral carotid artery stenosis was pointed out. The patient underwent CEA on the left side 6 months ago, and he was hospitalized to our hospital again for the purpose of CEA on the right side. The carotid artery stenosis was asymptomatic and he had no neurological deficit. Magnetic resonance angiography (MRA) revealed mild stenosis with white plaque at the origin of the right ICA [
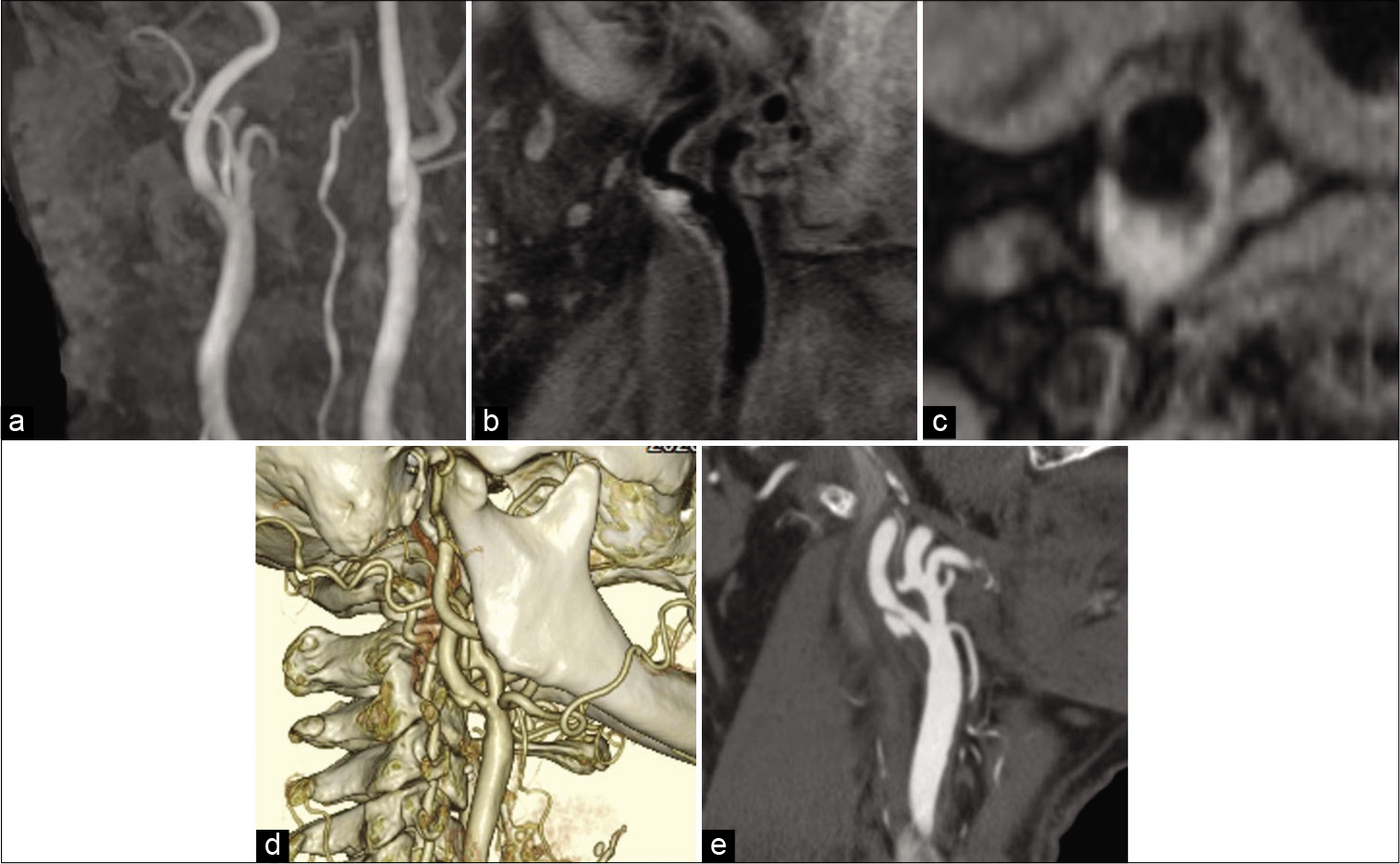
Figure 1:
(a) Magnetic resonance (MR) angiography revealing mild stenosis with white plaque at the origin of the right internal carotid artery (ICA). (b and c) MR plaque imaging (T1-weighted fat suppression black blood) revealing a high-intense (b; sagittal, c; axial). (d) Three-dimensional computed tomographic angiography (CTA) revealing mild stenosis with ulcer formation at the origin of the ICA. (e) A sagittal CTA maximum intensity projection image demonstrating a carotid web lesion.
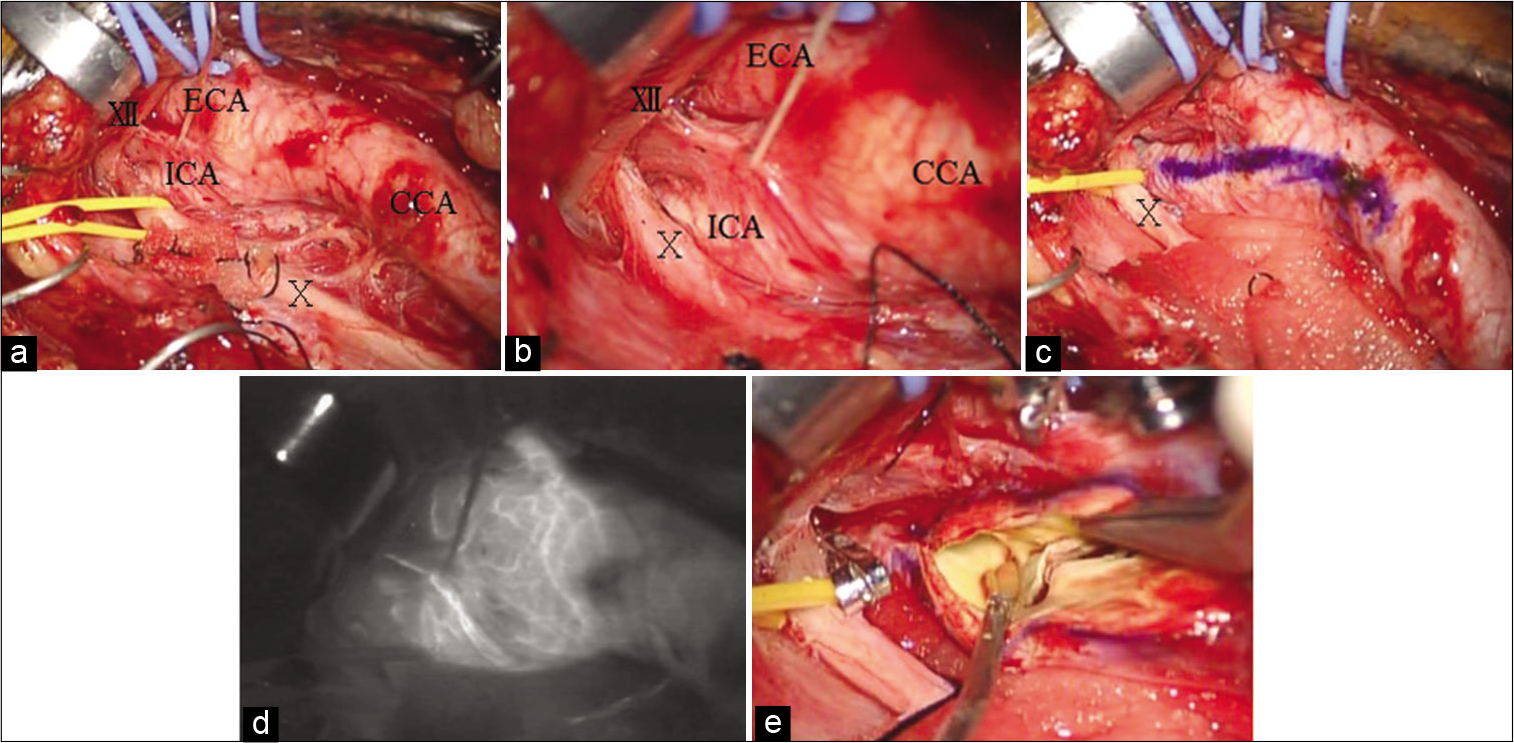
Figure 2:
(a and b) An operative photography demonstrating an unusual course of the vagus nerve passing anterior to the ICA. The internal jugular vein is retracted laterally. (c) The vagus nerve is moderately towed laterally with yellow silicone tape. An arteriotomy line is marked with Pyoktanin Blue. (d) The indocyanine green video angiography revealing vasa vasorum. (e) Lateral towing the vagus nerve with silicon tape has made the clamp of distal ICA and arteriotomy easier. X: Vagus nerve, XII; Hypoglossal nerve, CCA: Common carotid artery, ICA: Internal carotid artery, ECA: External carotid artery.
DISCUSSION
The effectiveness of CEA for advanced carotid stenosis has been established in many large studies, and CEA is the gold standard in surgical treatment. Avoidance of perioperative complications in CEA is very important to maintain the effectiveness. The major complication rates of CEA examined usually involve stroke, myocardial infarction, and death. Cranial nerve injuries are usually considered minor complications. Cranial nerve injury can be usually caused by direct trauma to the nerve by retraction, stretch, dissecting, excessive manipulation of the carotid sheath, the clamp, or bipolar coagulation. The most common cranial nerve injury following CEA was reported to involve hypoglossal nerve and the second is variably reported in the literature as facial nerve or vagus nerve.[
The vagus nerve exits the skull through the jugular foramen and it has a relatively straight course up to the thorax. It can be identified within the carotid sheath between the ICA and the CCA and the IJV in the neck, which is described as located posterior the vessels in a position posterolateral to the artery and posteromedial to the vein.[
Delicate dissection and prompt knowledge of cranial nerve tracts, their relations with surrounding structures and anatomical variations are fundamental steps for preventing cranial nerve injury during CEA.[
CONCLUSION
We experienced an extremely rare case of the vagus nerve passing anterior to the ICA during CEA. A delicate and complete dissection to understand the variation of the vagus nerve is crucial to minimize the risk of cranial nerve injury during CEA.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors thanks Takehiro Ito, Kazuya Honda, Nurse Practitioner, Our institution, for his invaluable comment on this article.
References
1. AbuRahma AF, Choueiri MA. Cranial and cervical nerve injuries after repeat carotid endarterectomy. J Vasc Surg. 2000. 32: 649-54
2. Giovagnorio F, Martinoli C. Sonography of the cervical vagus nerve: Normal appearance and abnormal findings. AJR Am J Roentgenol. 2001. 176: 745-9
3. Gradev A, Angelov AK, Dragolov M, Shahin TI, Jelev L. Unusual course of the vagus nerve in the neck passing anterior to the common carotid artery. Int J Anat Var. 2020. 13: 15-6
4. Hojaij F, Rebelo G, Akamatsu F, Andrade M, Camargo C, Cernea C. Syntopy of vagus nerve in the carotid sheath: A dissectional study of 50 cadavers. Laryngoscope Investig Otolaryngol. 2019. 4: 319-22
5. Park JK, Jeong SY, Lee JH, Lim GC, Chang JW. Variations in the course of the cervical vagus nerve on thyroid ultrasonography. AJNR Am J Neuroradiol. 2011. 32: 1178-81