- Department of Neurosurgery, The Aga Khan University Hospital, Karachi, Pakistan.
Correspondence Address:
Hafiza Fatima Aziz, Department of Neurosurgery, The Aga Khan University Hospital, Karachi, Pakistan.
DOI:10.25259/SNI_988_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hafiza Fatima Aziz, Muhammad Waqas Saeed Baqai, Rashid Jooma. Unusual presentation in syndrome of trephined – A unique case observation. 02-Dec-2022;13:562
How to cite this URL: Hafiza Fatima Aziz, Muhammad Waqas Saeed Baqai, Rashid Jooma. Unusual presentation in syndrome of trephined – A unique case observation. 02-Dec-2022;13:562. Available from: https://surgicalneurologyint.com/surgicalint-articles/12038/
Abstract
Background: Syndrome of trephined (SoT) is a well-recognized complication of decompressive craniectomy (DC). The understanding of SoT has improved more recently with the increasing utilization of DC for severely raised intracranial pressure. It usually presents after a period of weeks or months with a cluster of adverse neurological symptoms, most commonly with worsening of motor strength.
Case Description: An elderly gentleman with traumatic brain injury underwent DC. He later developed a sinking flap and unexplained agitation which responded to cranioplasty by returning to a state of calm. His cognitive function further improved over a period of 6 months. This is an unusual observation reported in this case.
Conclusion: Timely recognition of the cognitive complications of craniectomy that may respond to early cranioplasty promises to decrease the length of hospital stay and enhance rehabilitation in such patients.
Keywords: Cognitive dysfunction, Cranioplasty, Decompressive craniectomy, Sinking flap syndrome, Syndrome of trephined
INTRODUCTION
Syndrome of trephined (SoT) is a delayed sequel of decompressive craniectomy (DC), or any other neurosurgical procedure involving removal of a part of the cranium, leaving the brain without adequate bony coverage, and presents with a symptomatic deterioration of clinical features that are independent of the location and improve after cranioplasty.[
Appreciation of SoT has increased over time and its reported frequency has increased from an uncommon entity to up to 26% of decompressive craniectomies.[
Cognition includes language, memory, perception, recognition, reasoning, problem-solving, conceptualization, learning, and many other overlapping processes that define our knowledge and judgment.[
Here, we present a patient who developed severe agitation 5 weeks after DC and markedly improved immediately after cranioplasty.
CASE
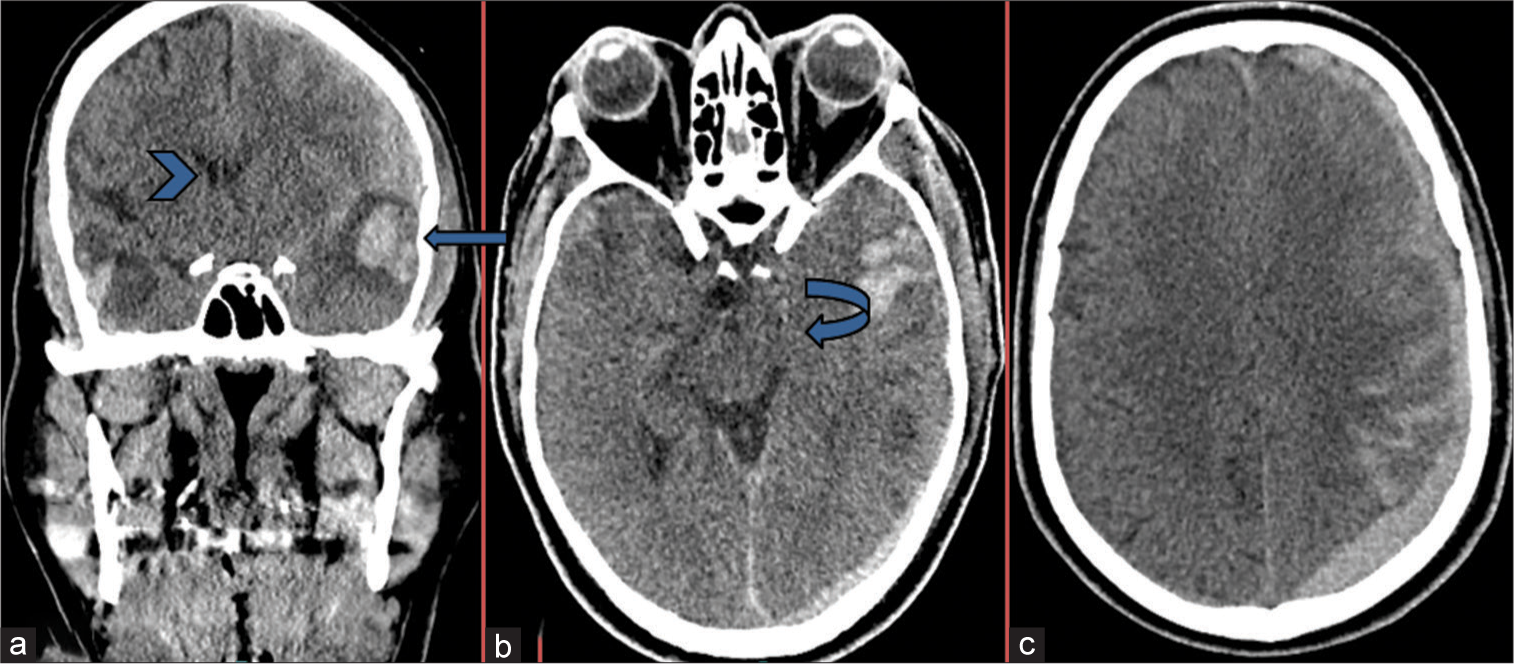
A 69-year-old hypertensive male was transferred to us with traumatic brain injury after sustaining a ground-level fall. On admission, his Glasgow Coma Scale was 12/15 (E4V2M6). CT scan depicted a left temporal hematoma with extensive acute subdural hematoma, diffuse edema and mass effect, and midline shift of 6.6 mm [
Figure 1:
(a-c) Coronal and axial images from unenhanced computed tomography scan brain reveal a large left temporal hemorrhagic contusion (blue arrow) with associated surrounding edema, resulting in mass affect and midline shift to right (Arrow head). There is accompanying effacement of the left-sided perimesencephalic basal cisterns raising the possibility of impending uncal herniation (curved). Extensive left acute subdural hematoma and subarachnoid hemorrhage.
One week later, the patient returned to the hospital with progressively worsening agitation without a decline in consciousness. CT scan showed interval development of the right chronic subdural hematoma with interval resolution of the previous acute hematoma. The hematoma was evacuated through burr-hole craniotomy and drain placement. The procedure was uneventful but after the surgery, his agitation increased (RASS + 3) and cognitive dysfunction did not improve. Mini-Mental Score could not be assessed as his comprehension was not intact. At this point, patient was extensively evaluated for other causes of agitation such as electrolytes disturbances, endocrine abnormalities, infection, sepsis, drug intoxication, or alcohol withdrawal, all workup was within normal limits.
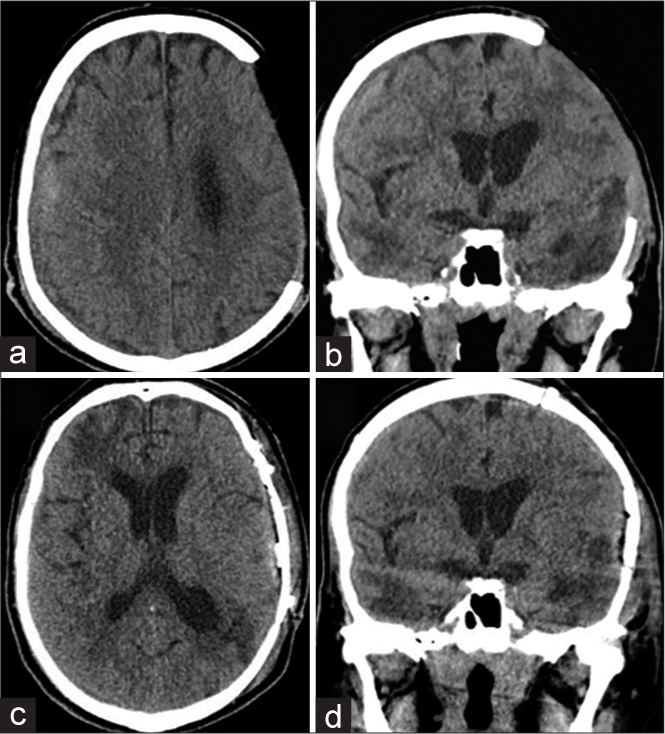
On serial CT scans, the right subdural collections decreased and his craniotomy skin flap started to sink. Suspecting “syndrome of trephined” and in view of his persistently unexplained behavioral dysfunction, we planned for early cranioplasty which was performed 6 weeks after the primary procedure [
At 6-month follow-up, the patient was found able to walk unattended and only required minimal assistance with his activities of daily living (ADL) (MRS 3). His comprehension had also improved considerably and he was able to follow two-step commands with consistency.
DISCUSSION
DC can be a life-saving procedure for certain neurosurgical emergencies such as traumatic brain injury and acute vascular occlusions. A recently published meta-analysis of RCTs for DC in traumatic brain injury found a mortality benefit over the best medical treatment.[
Di Rienzo et al. described SoT as a sunken scalp flap irrespective of posture with radiological evidence of depressed parenchyma and a new onset physical or cognitive deterioration.[
Data regarding the quantitative use of neuropsychological or cognition assessment tools before and after cranioplasty are not established in the literature so the extent of improvement is not clearly defined.[
Cranioplasty results in an improvement in 3–53% of cognitive symptoms as reported in different case series.[
CONCLUSION
With the wider use of cranial decompression in emergency neurosurgical practice, SoT is now being encountered more frequently. Combative and agitated behavior without a deteriorating level of alertness can be a rare manifestation of SoT and if recognized may respond well to early cranioplasty.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Agner C, Dujovny M, Gaviria M. Neurocognitive assessment before and after cranioplasty. Acta Neurochir (Wien). 2002. 144: 1033-40 discussion 1040
2. Ashayeri K, Jackson EM, Huang J, Brem H, Gordon CR. Syndrome of the trephined: A systematic review. Neurosurgery. 2016. 79: 525-34
3. Beez T, Munoz-Bendix C, Steiger HJ, Beseoglu K. Decompressive craniectomy for acute ischemic stroke. Crit Care. 2019. 23: 209
4. Carota A, Pintucci M, Zanchi F, D’ambrosio E, Calabrese P. ‘Cognitive’ sinking skin flap syndrome. Eur Neurol. 2011. 66: 227-8
5. Coelho F, Oliveira AM, Paiva WS, Freire FR, Calado VT, Amorim RL. Comprehensive cognitive and cerebral hemodynamic evaluation after cranioplasty. Neuropsychiatr Dis Treat. 2014. 10: 695-701
6. Corallo F, Calabro RS, Leo A, Bramanti P. Can cranioplasty be effective in improving cognitive and motor function in patients with chronic disorders of consciousness? A case report. Turk Neurosurg. 2015. 25: 193-6
7. Cummings J, Mintzer J, Brodaty H, Sano M, Banerjee S, Devanand DP. Agitation in cognitive disorders: International psychogeriatric association provisional consensus clinical and research definition. Int Psychogeriatr. 2015. 27: 7-17
8. Di Rienzo A, Colasanti R, Gladi M, Pompucci A, Costanza MD, Paracino R. Sinking flap syndrome revisited: The who, when and why. Neurosurg Rev. 2020. 43: 323-35
9. Di Stefano C, Sturiale C, Trentini P, Bonora R, Rossi D, Cervigni G. Unexpected neuropsychological improvement after cranioplasty: A case series study. Br J Neurosurg. 2012. 26: 827-31
10. Garg K, Singh PM, Singla R, Aggarwal A, Borle A, Singh M. Role of decompressive craniectomy in traumatic brain injury-a meta-analysis of randomized controlled trials. Neurol India. 2019. 67: 1225-32
11. Grant FC, Norcross NC. Repair of cranial defects by cranioplasty. Ann Surg. 1939. 110: 488-512
12. Honeybul S, Janzen C, Kruger K, Ho KM. The impact of cranioplasty on neurological function. Br J Neurosurg. 2013. 27: 636-41
13. Sedney CL, Dillen W, Julien T. Clinical spectrum and radiographic features of the syndrome of the trephined. J Neurosci Rural Pract. 2015. 6: 438-41
14. Semkovska M, McLoughlin DM. Objective cognitive performance associated with electroconvulsive therapy for depression: A systematic review and meta-analysis. Biol Psychiatry. 2010. 68: 568-77
15. Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O’Neal PV, Keane KA. The Richmond agitation-sedation scale: Validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002. 166: 1338-44
16. Smith M, Servadei F, Hutchinson PJ. What is new in decompressive craniectomy in neurological emergencies: The good, the bad and the ugly. Intensive Care Med. 2020. 46: 1023-6
17. Stiver SI. Complications of decompressive craniectomy for traumatic brain injury. Neurosurg Focus. 2009. 26: E7
18. Winkler PA, Stummer W, Linke R, Krishnan KG, Tatsch K. Influence of cranioplasty on postural blood flow regulation, cerebrovascular reserve capacity, and cerebral glucose metabolism. J Neurosurg. 2000. 93: 53-61