- Department of Spine Disorders, Hospital Español, Mendoza, Argentina
- Clínica La Pequeña Familia, Junín, Buenos Aires, Argentina
- Neurosurgery Department, Universidad de Caxias do Sul, Brasil
Correspondence Address:
Guiroy Alfredo
Neurosurgery Department, Universidad de Caxias do Sul, Brasil
DOI:10.4103/sni.sni_390_17
Copyright: © 2018 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Guiroy Alfredo, Zanardi Carlos, Picard Nelson, Sícoli Alfredo, Morales C. Alejandro, Falavigna Asdrúbal. Using the “ligamentum flavum gap” to identify originally missed type B vertebral fractures. 10-Jan-2018;9:5
How to cite this URL: Guiroy Alfredo, Zanardi Carlos, Picard Nelson, Sícoli Alfredo, Morales C. Alejandro, Falavigna Asdrúbal. Using the “ligamentum flavum gap” to identify originally missed type B vertebral fractures. 10-Jan-2018;9:5. Available from: http://surgicalneurologyint.com/surgicalint-articles/using-the-ligamentum-flavum-gap-to-identify-originally-missed-type-b-vertebral-fractures/
Abstract
Background:Spine fractures may involve the ligamentum flavum (LF). Here, we utilized the “ligamentum flavum gap,” defined by the discontinuity of the LF at the level of a vertebral fracture, to document a vertebral fracture.
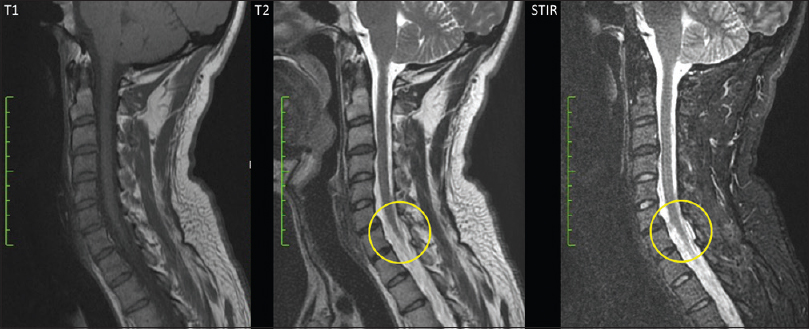
Methods:Utilizing X-rays, computed tomography (CT), and magnetic resonance (MR) studies, 10 patients with type B vertebral fractures were diagnosed with the ligamentum flavum gap (LFG: discontinuity of the LF) at the fracture levels. The fractures were located in 2 patients in the cervical and 8 in the thoracolumbar spine.
Results:All 10 patients with vertebral fractures had complained of axial pain. Four also showed progressive thoracic kyphosis. Notably, all demonstrated a loss of continuity in the LF at the level of fracture “ligamentum flavum gap.” T2-weighted and short tau inversion recovery (STIR) MR sagittal studies were best at locating LFG at the level of a fracture.
Conclusion:Here, we identified best on sagittal T2 and STIR-weighted MR studies 10 patients for whom discontinuity of the ligamentum flavum (LFG) correlated with the location of type B vertebral fractures.
Keywords: Magnetic resonance, posterior ligament complex, spine, thoracolumbar trauma, vertebral fracture
INTRODUCTION
Spine lesions are common in trauma patients, and most of these lesions (75–90%) involve the thoracolumbar junction (T10-L2).[
Fracture morphology is typically divided into three types – compression (type A), distraction (type B), and rotation or dislocation (type C). Subgroups B2 and B3 of type B lesions include ligament damage which makes them highly unstable. When diagnosed early on, unstable lesions may be managed successfully and deformities can be prevented. In some cases, ligament and joint disruption is evident as there is distraction of spinous processes. Hyperintensity on T2-weighted and short tau inversion recovery (STIR) magnetic resonance (MR) images significantly contribute to diagnosing ligamentous rupture.[
Weeks after the trauma, however, both edema and inflammation originally present on the MRI may resolve. At this point, delayed evidence of instability may develop, and kyphosis (angle ≥10°), loss of vertebral height (≥50%), translation (X-rays >3.5 mm), and further fixed kyphosis can be found.[
Here, we analyzed the appearance of “gaps” in the ligamentum flavum to diagnose fractures that were originally missed.
MATERIALS AND METHODS
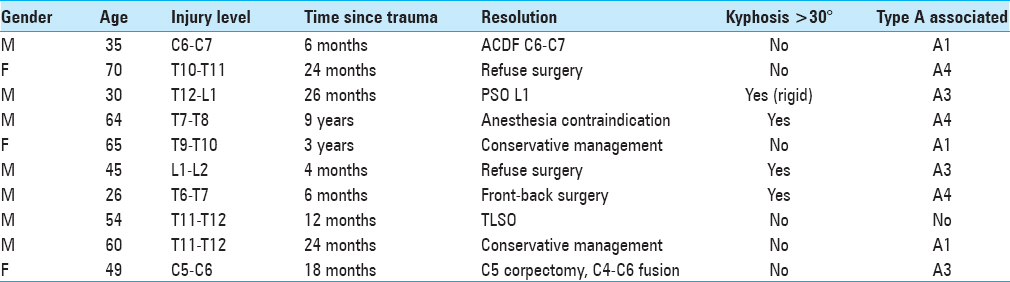
Clinical files of 10 patients with type B spine fractures between 2013 and 2016 correlating with ligamentum flavum “gap” lesions were identified from 2 centers. There were 7 males and 3 females with an average age of 49.8 years (26–70 years). All the patients had high energy trauma (9 motor vehicle accidents, 1 patient had a fall from 5 m height). The average delay between the traumatic event and the diagnosis of the type B vertebral fractures was 26.4 months (4–108 months) [
The study included an analysis of digital AP standing full spine X-rays, flexion-extension X-rays, X-rays in the prone position, and MRI studies (1.5 T). The Cobb angle was used to measure spinal curvatures using Surgimap® (version 2.2.9.9.4). Five spine surgeons with experience in trauma were asked to identify “gap” lesions of the LF at levels of vertebral fractures.
RESULTS
All patients following their traumatic events complained of persistent axial pain (8 in the thoracolumbar region and 2 in the cervical region). Notably, this pain improved in the supine position and worsened with either sitting or standing. In 4 cases, kyphosis of the thoracolumbar junction >30° was confirmed, and 1 patient presented a rigid thoracic kyphosis [
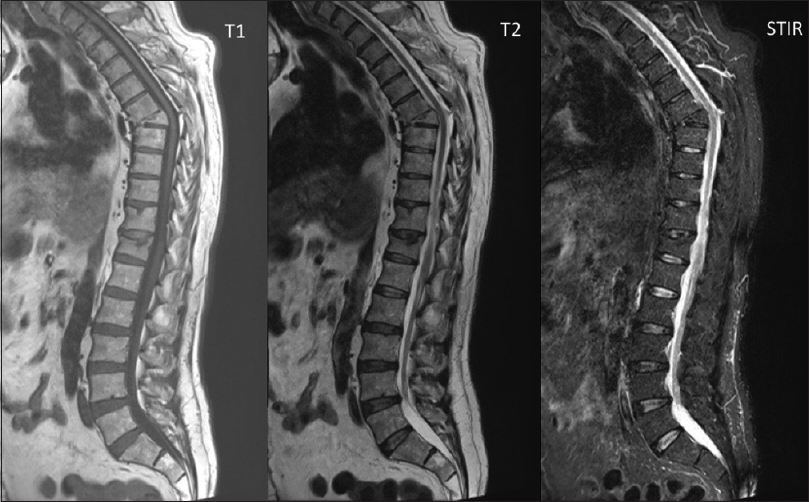
Figure 1
Case report 1. 64-year old male with a history of motor vehicle accident 9 years prior to consultation. This figures shows the sagittal T1 weighted, T2 weighted and STIR MRI images of the thoraco-lumbo-sacral spine. See the regional kyphosis at the level of T7-T8 with wedging of the T7 vertebral body
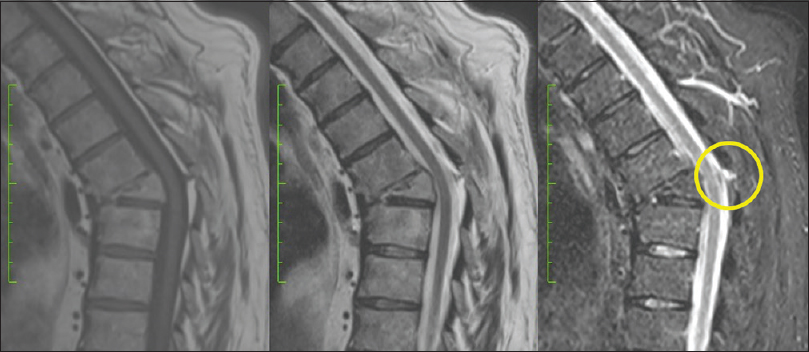
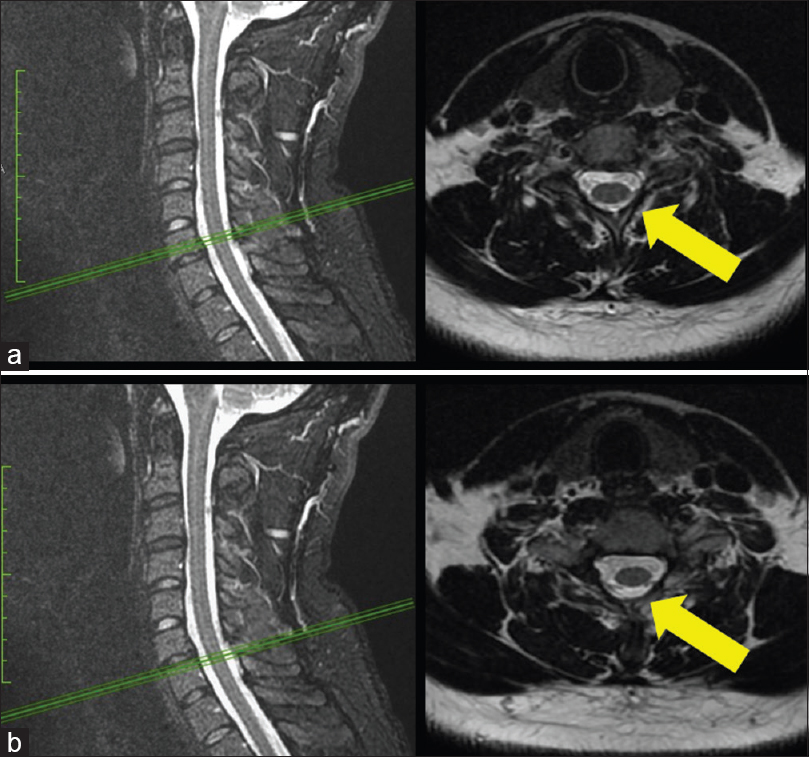
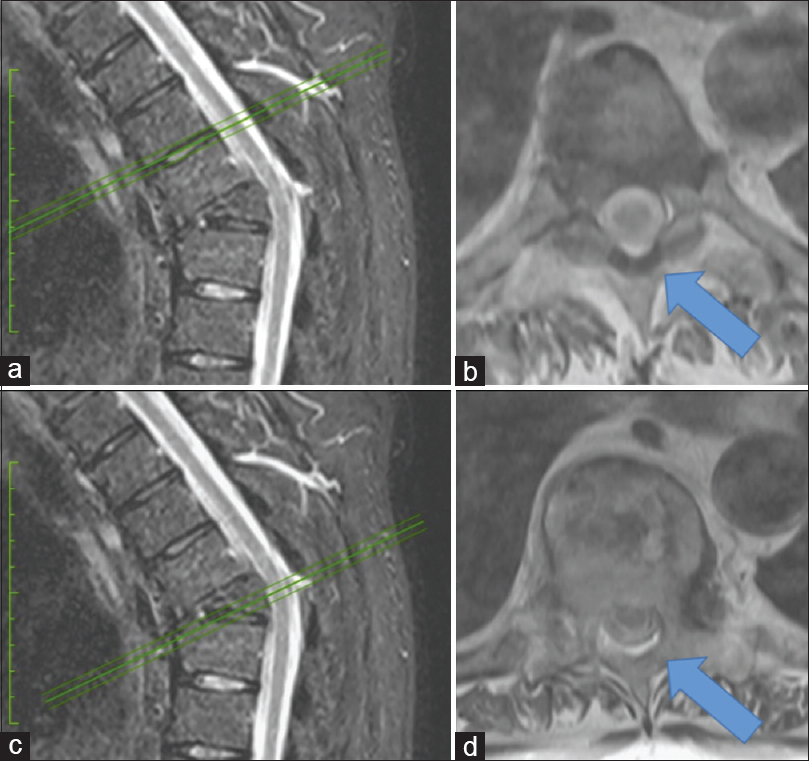
All 10 patients had signs of a “gap” LF injury (discontinuity) that correlated with fracture levels. This was better visualized in sagittal T2-weighted and STIR MRI sequences. A retrospective analysis of the early posttraumatic MR images showed that 5 of the 10 patients had original MRI signs of edema involving the soft tissues, suggestions that original type B vertebral fractures were missed [Figures
The sign of LFG was more evident in the sagittal slices than in the axial slices. In this series, only 4 patients of 10 developed posttraumatic deformities [
DISCUSSION
Fractures of the spine are common, and 75–90% occur at the level of the thoracolumbar junction.[
In the acute setting of trauma, the diagnosis of a “gap” LF lesion is simpler, as there is typically an increase in the interspinous distance accompanied by facet dislocation, increased periarticular fluid, and/or hyperintensity in the adjacent dorsal muscles in T2-weighted and STIR MRI images.[
After some weeks, however, acute ligament edema and inflammation resolve, and the diagnosis of ligament damage becomes difficult. In the chronic setting, type B lesions are diagnosed indirectly based on the finding of segment kyphosis progression (≥30°) or instability in this location (change of 10° or more when standing in relation to the supine position in the region of the fracture).[
Early diagnosis of fractures with ligament rupture might help decrease the rate of posttraumatic deformities, which in general requires more complex surgical management. In this report, we describe an MRI sign of discontinuity of the ligamentum flavum as a direct indicator of PLC damage in the chronic setting.
CONCLUSION
Here, we could establish “late” type B vertebral fractures in 10 patients utilizing a “gap” sign reflecting disruption of the LF.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Chen JX, Goswami A, Xu DL, Xuan J, Jin HM, Xu HM. The radiologic assessment of posterior ligamentous complex injury in patients with thoracolumbar fracture. Eur Spine J. 2017. 26: 1454-62
2. Pizones J, Sanchez-Mariscal F, Zúñiga L, Alvarez P, Izquierdo E. Prospective analysis of Magnetic resonance imaging accuracy in diagnosing traumatic injuries of the posterior ligamentous complex of the thoracolumbar spine. Spine. 2013. 38: 745-51
3. Radcliff K, Su B, Kepler C, Rubin T, Shimer AL, Rihn JA. Correlation of posterior ligamentous complex injury and neurological injury to loss of vertebral body height, kyphosis and canal compromise. Spine. 2016. 37: 1142-50
4. Rajasekaran S, Maheswaran A, Aiyer S, Kanna R, Dumpa S, Shetty A. Prediction of posterior ligamentous complex injury in thoracolumbar fractures using non-MRI imaging techniques. Int Orthop. 2016. 40: 1075-81
5. Rihn JA, Yang N, Fisher C, Saravanja D, Smith H, Morrison WB. Using magnetic resonance imaging to accurately assess injury to the posterior ligamentous complex of the spine: A prospective comparison of the surgeon and radiologist. J Neurosurg Spine. 2010. 12: 391-6
6. Vaccaro A, Rihn J, Saravanja D, Anderson D, Hilibrand AS, Albert TJ. Injury of the Posterior Ligamentous Complex of the Thoracolumbar Spine. A Prospective Evaluation of the Diagnostic Accuracy of Magnetic Resonance Imaging. Spine. 2009. 34: E841-7
7. Wolf M, Weber M. Neuroimaging of the traumatic spine. Magn Reson Imaging Clin N Am. 2016. 24: 541-61