- Department of Spine surgery, Spine Clinic “Dr. Manuel Dufoo Olvera,” Specialty Hospital- National Medical Center “La Raza”, Mexico City, Mexico.
- Department of Neuroanesthesiology, Specialty Hospital- National Medical Center “La Raza”, Mexico City, Mexico.
- Department of Neurosurgery, Specialty Hospital- National Medical Center “La Raza”, Mexico City, Mexico.
Correspondence Address:
Oscar Josue Montes Aguilar, Department of Spine Surgery, Spine Clinic “Dr. Manuel Dufoo Olvera,” México City, Mexico.
DOI:10.25259/SNI_872_2022
Copyright: © 2022 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Oscar Josue Montes Aguilar1, Karmen Karina Alaniz Sida2, Leonardo Álvarez Betancourt3, Manuel Dufoo Olvera1, Guillermo Ivan Ladewig Bernaldez1, Ramón López López3, Edith Oropeza Oropeza1, Héctor Alonso Tirado Ornelas3. Variability in wound closure technique in midline posterior lumbar fusion surgery. International survey and standardized closure technique proposal. 18-Nov-2022;13:534
How to cite this URL: Oscar Josue Montes Aguilar1, Karmen Karina Alaniz Sida2, Leonardo Álvarez Betancourt3, Manuel Dufoo Olvera1, Guillermo Ivan Ladewig Bernaldez1, Ramón López López3, Edith Oropeza Oropeza1, Héctor Alonso Tirado Ornelas3. Variability in wound closure technique in midline posterior lumbar fusion surgery. International survey and standardized closure technique proposal. 18-Nov-2022;13:534. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=12012
Abstract
Background: Surgical wound complications represent an important risk factor, particularly in multilevel lumbar fusions. However, the literature regarding optimal wound closure techniques for these procedures is limited.
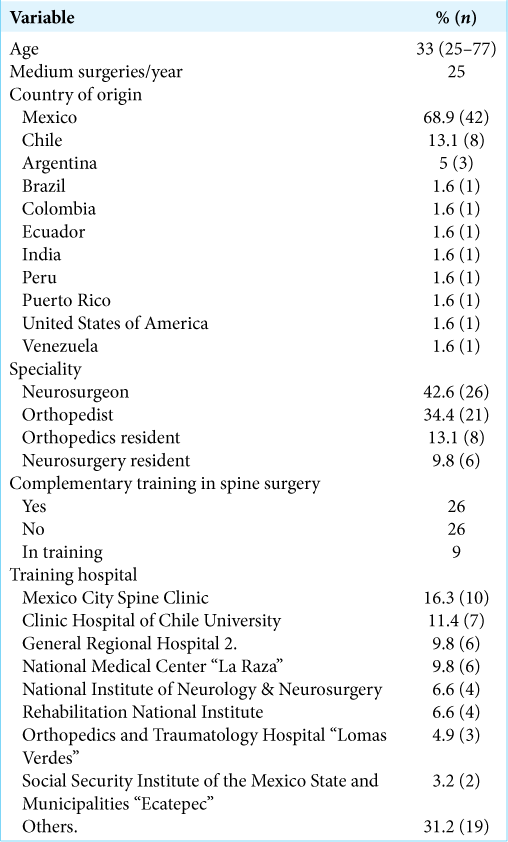
Methods: We performed an online survey of 61 spinal surgeons from 11 countries, involving 25 different hospitals. The study included 26 neurosurgeons, 21 orthopedists, and 14 residents (Neurosurgery – 6 and orthopedics 8). The survey contained 17 questions on demographic information, closure techniques, and the use of drainage in posterior lumbar fusion surgery. We then developed a “consensus technique.”
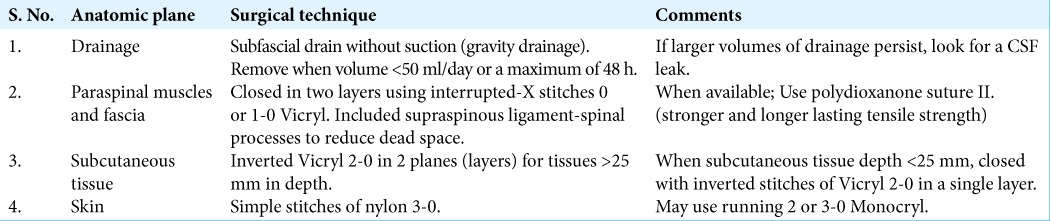
Results: The proposed standardized closure techniques included: (1) using subfascial gravity drainage (i.e., without suction) with drain removal for 25 mm in depth, and (4) skin closure with simple interrupted nylon 3-0 sutures.
Conclusion: There is great variability between closure techniques utilized for multilevel posterior lumbar fusion surgery. Here, we have described various standardized/evidence-based proven techniques for the closure of these wounds.
Keywords: Midline posterior lumbar fusion, Spine surgery, Standardized closure, Wound closure
INTRODUCTION
Surgical wound complications (incidence: 0.2–20%) for patients undergoing multilevel lumbar fusion surgery represent major risk factors that increase morbidity, mortality, and hospital costs.[
MATERIALS AND METHODS
We conducted an online survey of 61 participants: 26 neurosurgeons (+6 residents), 21 orthopedists (+8 residents) from 11 countries, to 25 different hospitals [
RESULTS
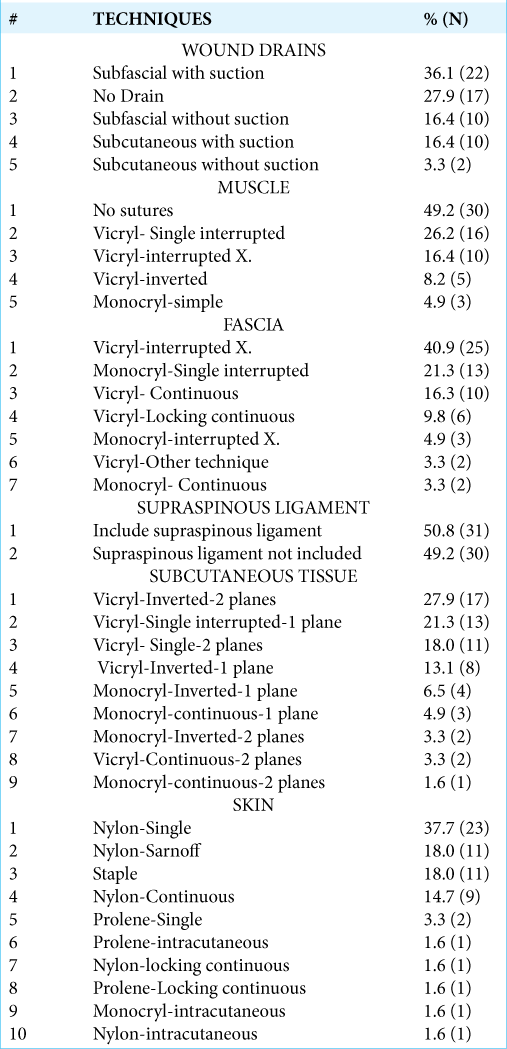
Although 50.8% (31) of surgeons reported using a standardized closure method, they utilized different techniques for each of the planes of closure. In all, we encountered 61 different closure combinations for the 61 participants [
DISCUSSION
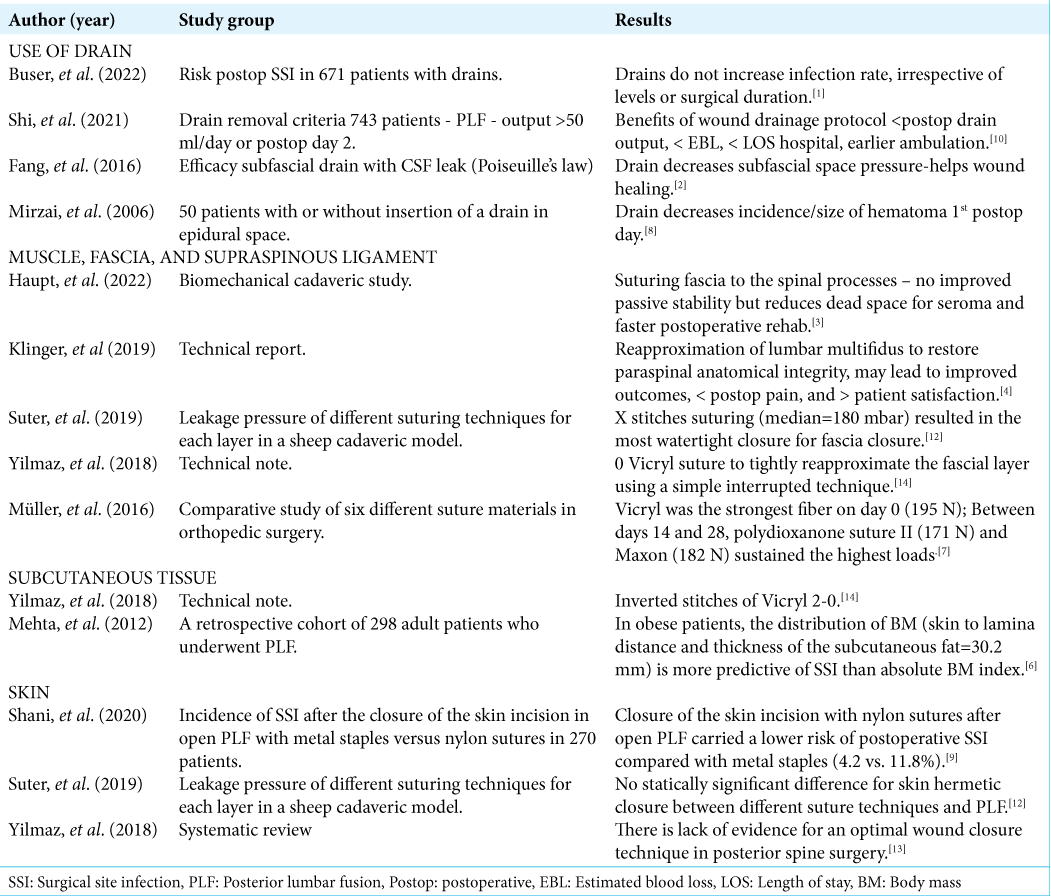
We analyzed the variability in the midline posterior closure techniques utilized by 26 neurosurgeons, 21 orthopedists, and 14 residents to perform multilevel lumbar spine fusion surgery. Different studies have individually evaluated closure techniques in multilevel lumbar fusion surgery [
Our standardized technique first included utilizing a subfascial drain without suction (i.e., gravity drainage) with drain removal either when the volume was < 50 ml/day or when the drain has been in place a maximum of 48 h. (note: if larger volumes of drainage persist look for a cerebrospinal fluid leak).[
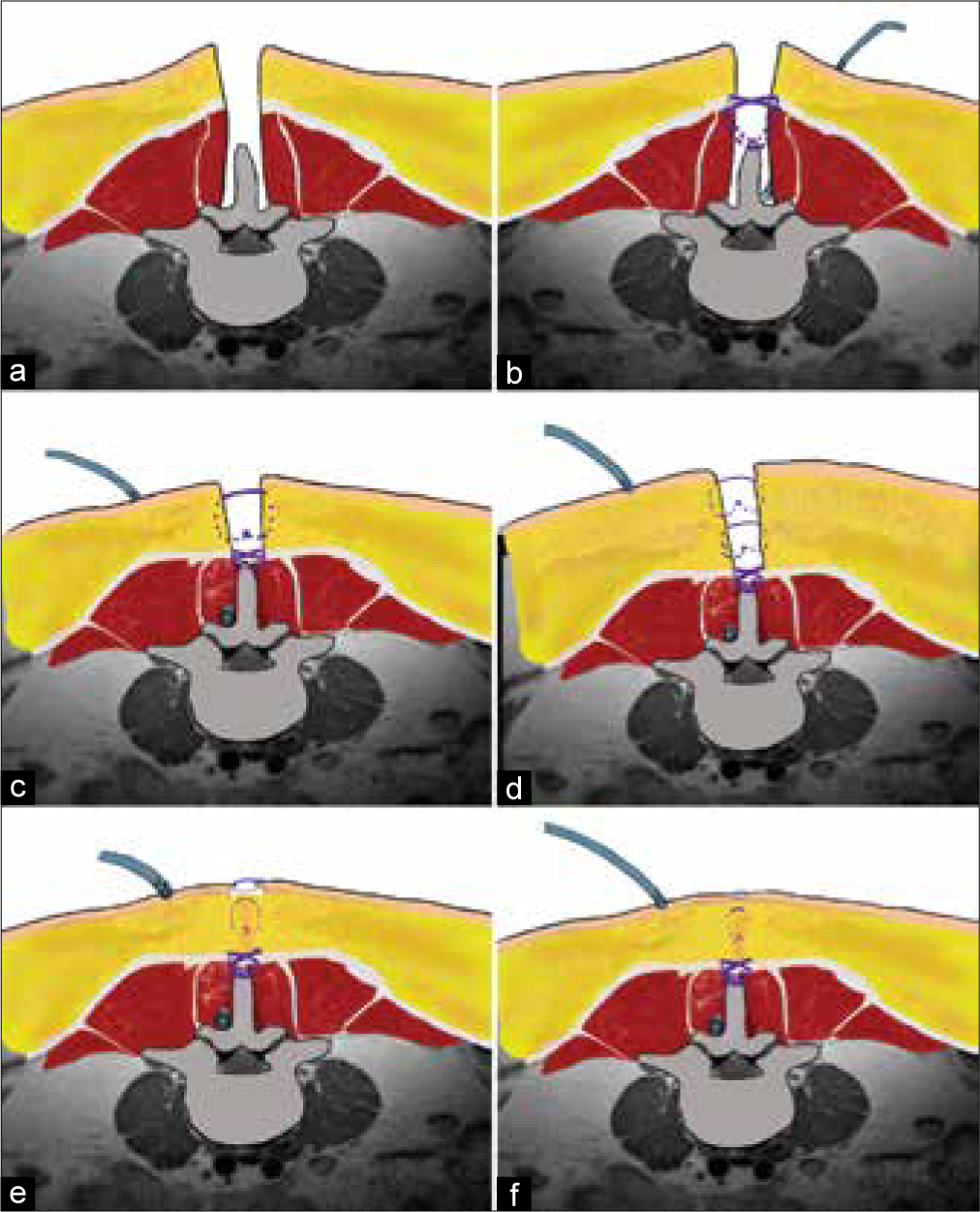
Figure 1:
(a) Midline posterior lumbar approach. (b) Using subfascial gravity drainage (i.e., without suction) with drain removal for <50 ml/day or a maximum duration of 48 h; paraspinal muscle and fascia closure with an interrupted-X technique of Vicryl 1 or other longer-lasting resorbable suture and include the supraspinous ligament. (c) Closure of subcutaneous tissue with interrupted inverted stitches of Vicryl 2-0 in 1 single plane when depth <25 mm. (d) Two planes for subcutaneous tissue greater > than 25 mm in depth. (e) Skin closure with simple interrupted nylon 3-0 sutures. (f) Standardized closure.
CONCLUSION
Process standardization enables evidence-based continual improvement by comparing different interventions on the same process.[
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Buser Z, Chang K, Kall R, Formanek B, Arakelyan A, Pak S. Lumbar surgical drains do not increase the risk of infections in patients undergoing spine surgery. Eur Spine J. 2022. 31: 1775-83
2. Fang Z, Jia Y, Tian R, Liu Y. Subfascial drainage for management of cerebrospinal fluid leakage after posterior spine surgery-a prospective study based on Poiseuille’s law. Chin J Traumatol. 2016. 19: 35-8
3. Haupt S, Cornaz F, Falkowski AL, Widmer J, Farshad M. Biomechanical considerations of the posterior surgical approach to the lumbar spine. Spine J. 2022. p.
4. Klinger N, Yilmaz E, Halalmeh DR, Tubbs RS, Moisi MD. Reattachment of the multifidus tendon in lumbar surgery to decrease postoperative back pain: A technical note. Cureus. 2019. 11: e6366
5. Lee N, Shin J, Kothari P, Kim J, Leven D, Steinberger J. Incidence, impact, and risk factors for 30-day wound complications following elective adult spinal deformity surgery. Global Spine J. 2017. 7: 417-24
6. Mehta A, Babu R, Karikari I, Grunch B, Agarwal V, Owens T. 2012 young investigator award winner: The distribution of body mass as a significant risk factor for lumbar spinal fusion postoperative infections. Spine (Phila Pa 1976). 2012. 37: 1652-6
7. Müller DA, Snedeker JG, Meyer DC. Two-month longitudinal study of mechanical properties of absorbable sutures used in orthopedic surgery. J Orthop Surg Res. 2016. 11: 111
8. Mirzai H, Eminoglu M, Orguc Ş. Are drains useful for lumbar disc surgery? A prospective randomized clinical study. J Spinal Disord Tech. 2006. 19: 171-7
9. Shani A, Poliansky V, Mulla H, Rahamimov N. Nylon skin sutures carry a lower risk of post-operative infection than metal staples in open posterior spine surgery: A retrospective case-control study of 270 patients. Surg Infect (Larchmt). 2020. 21: 440-4
10. Shi H, Huang ZH, Huang Y, Zhu L, Jiang ZL, Wang YT. Which criterion for wound drain removal is better following posterior 1-level or 2-level lumbar fusion with instrumentation: Time driven or output driven?. Global Spine J. 2021. p.
11. Skjold-Ødegaard B, Søreide K. Standardization in surgery: Friend or foe?. Br J Surg. 2020. 107: 1094-6
12. Suter A, Spirig J, Fornaciari P, Bachmann E, Götschi T, Klein K. Watertightness of wound closure in lumbar spine-a comparison of different techniques. J Spine Surg. 2019. 5: 358-64
13. Yilmaz E, Blecher R, Moisi M, Ankush C, O’Lynnger T, Abdul-Jabbar A. Is there an optimal wound closure technique for major posterior spine surgery? A systematic review. Global Spine J. 2018. 8: 535-44
14. Yilmaz E, Tawfik T, O’Lynnger T, Iwanaga J, Blecher R, Abdul-Jabbar A. Wound closure after posterior multilevel lumbar spine surgery: An anatomical cadaver study and technical note. Cureus. 2018. 10: e3595