- Department of Neurosurgery, Helsinki University Hospital, Helsinki, Finland
- Department of Neurosurgery, Umberto I General Hospital, Università Politecnica delle Marche, Ancona, Italy
- Department of Anesthesiology, Intensive Care and Pain Medicine, University of Helsinki and Helsinki University Hospital, Helsinki, Finland
- Department of Neurosurgery, Ospedali Riuniti Marche Nord, Pesaro, Italy
Correspondence Address:
Joham Choque-Velasquez
Department of Neurosurgery, Helsinki University Hospital, Helsinki, Finland
DOI:10.4103/sni.sni_128_18
Copyright: © 2018 Surgical Neurology International This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.How to cite this article: Joham Choque-Velasquez, Roberto Colasanti, Julio C. Resendiz-Nieves, Rahul Raj, Ann-Christine Lindroos, Behnam Rezai Jahromi, Juha Hernesniemi. Venous air embolisms and sitting position in Helsinki pineal region surgery. 10-Aug-2018;9:160
How to cite this URL: Joham Choque-Velasquez, Roberto Colasanti, Julio C. Resendiz-Nieves, Rahul Raj, Ann-Christine Lindroos, Behnam Rezai Jahromi, Juha Hernesniemi. Venous air embolisms and sitting position in Helsinki pineal region surgery. 10-Aug-2018;9:160. Available from: http://surgicalneurologyint.com/surgicalint-articles/test/
Abstract
Background:Nowadays, the sitting position has lost favor among neurosurgeons partly due to assumptions of increased complications, such as venous air embolisms (VAEs) and hemodynamic disturbances. The aim of our study is to describe the importance of some anesthetic considerations and the utility of antigravity trousers as well, together with a skillful neurosurgery and an imperative proper teamwork, in order to prevent the risk of severe VAE during pineal region surgery. We routinely use them for the variant of the sitting position we developed, the “praying position.”
Methods:A retrospective review of 51 pineal lesions operated on in the “praying position” using antigravity trousers was carried out. In the “praying position” the legs of the patient are kept parallel to the floor. Hence, antigravity trousers are used to generate an adequate cardiac preload.
Results:VAE associated to persistent hemodinamic changes was nonexistent in our series. The rate of VAE was 35.3%. VAEs were diagnosed mainly by monitoring of the end-tidal CO2 (83.33%). A venous system lesion was the cause in most of the cases. When VAE was suspected, an inmediate reaction based on a good teamwork was imperative. No cervical spine cord injury nor peripheral nerve damage were reported. The average microsurgical time was 48 ± 33 min.
Conclusions:The risks of severe VAE during pineal region surgery in the “praying-sitting position” may be effectively prevented by some essential anesthetic considerations and the use of antigravity trousers together with a skillful neurosurgery, and an imperative proper teamwork.
Keywords: Air embolism, antigravity trousers, hemodynamics, microneurosurgery, pineal region lesions, sitting position
INTRODUCTION
Pineal lesions are challenging because of their location deep inside the intracranial space and their proximity to critical neurovascular brain structures. Several advantages may be offered by the use of the sitting position for pineal region surgery such as: lower intracranial pressure, good venous outflow, gravitational retraction, and straight anatomical orientation.[
A variant of the classic sitting position, the praying position, was developed in our department with the aim to reduce the rate of severe complications, while allowing an ergonomic posture for the surgeon. In the praying position, remarkably, it is not required to elevate the legs of the patient above the level of the heart. Conversely, we routinely use antigravity (G-suit) trousers in order to reduce the risk of complications due to a decreased cardiac preload.[
The objective of this paper is to describe the importance of some anesthetic considerations and the utility of antigravity trousers as well, together with a skillful neurosurgery and an imperative proper teamwork, to prevent the risk of severe VAE during pineal region surgery, while offering an ergonomic surgical positioning.
MATERIAL AND METHODS
Study design and ethics
This is a single-center retrospective study regarding the evaluation of VAE during the surgical treatment of consecutive pineal region lesions operated on in sitting position. Following the Institutional Review Board approval, data were collected from hospital records, and neuroradiological imaging was reviewed. The patients consent was not required as this is a retrospective study, and the research data analysis had no effect on the participants or their medical care.
Participants and study size
Patients with pineal lesions that were operated on in the “praying position” using G-suit trousers by the senior author (JH) between January 2008 and October 2015. Patients with missing information were excluded.
During the study period, 64 patients with pineal lesions were treated. Of these, 51 met the study inclusion criteria (25 men and 26 women). Mean patient age was 37.2 years (range, 8–79 years).
Variables
Venous air embolism
We defined VAE as any of the following: 1) an embolic heart sound by precordial Doppler ultrasound; 2) a 0.7 kPa (5.25 mmHg) or greater decrease in the end-tidal PCO2; 3) identification of the air leak at the surgical site.[
Sitting position
In our department, the sitting positioning style for pineal region lesions, regardless of the surgical approach (supracerebellar infratentorial or occipital interhemispheric route), is a standardized protocol that ends in a somersault position (“praying-sitting position”) with the horizontal axis of the tentorium parallel to the floor, with less than 90° in relation to the axis of the surgeon [
In the classic sitting position as illustrated by Porter et al., both legs are raised as high as possible in order to prevent the risk of complications.[
Antigravity trousers
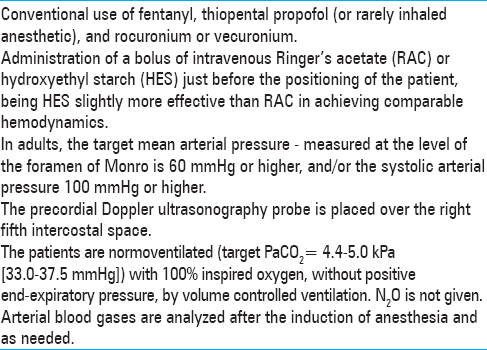
The G-suit trousers are applied at the lower limbs of the patient up to the level of his/her hips (the G-suit trousers are applied when the patient is in supine position, intubated, with peripheral venous access and with urinary catheter). Patients are dressed in antigravity trousers (Trousers ANTI-G, NATO No 8475-99-1300180, Beaufort, Belfast, UK), which are inflated with compressed air up to a pressure of about 40 mmHg. There is a potential risk for peripheral nerves and/or blood vessels injuries, but the shape of the trousers allows the positioning of the patient without intense compression of critical points. Flexible positioning of lower extremities joints is possible. Effective blood gas test, hemodynamic monitoring, and precordial Doppler ultrasound are mandatory [
Thanks to their side zippers, antigravity trousers can be applied in less than 5 min for normal weight adult patients. Their main physiological effect is to increase the peripheral resistance, thus redistributing the blood to body areas above the suit and improving the cardiac preload.[
Microneurosurgery
As previously described, microneurosurgery of the pineal region in Helsinki Neurosurgery is performed according to the following protocol.[
The surgical strategy is routinely planned based on MRI and CT. Digital subtraction angiography is occasionally used in highly vascularized lesions to determine the main feeders of the lesion. The study of the deep venous system is the most valuable factor in planning the surgical strategy. The paramedian supracerebellar suboccipital approach is the preferred route in our center, as described in a previous paper.[
Once the quadrigeminal cistern is opened and the lesion reached, at the beginning we use to take tumor samples for histopathological analysis, and then we endeavor to progressively accomplish a complete resection. In case of vascular pineal lesions, the analysis of their angioarchitecture is crucial in order to attempt their complete removal. During the intradural stage, it is essential to distinguish the deeply located veins from the dark blue-colored cisterns. Along the supracerebellar approach, the precentral vein is recognized and, if needed, it is coagulated and cut. The microsurgical dissection starts laterally following the cleavage plane between the lesion and its vicinity. An internal debulking is performed by using aspiration, as well as the mechanical and thermal effect of the bipolar forceps. Once the posterior third ventricle is reached, additional cerebrospinal fluid is released. The tumor is carefully dissected from the surrounding veins with the help of water dissection to complete the microsurgical excision. Ultrasonic aspirator is rarely used during this surgery in Helsinki.
The angle below the posterior commissure requires extreme care. The slightest bleeding could determine fatal consequences and small residual tumors as well. Microsurgical mirrors or endoscopes may help to visualize this area. After complete resection, careful hemostasis is imperative. In case of malignant and infiltrative tumors, radical decompression is mostly offered. However, if possible, we try to remove the lesion completely. In case of vascular malformations, a careful microsurgical dissection should take into consideration their anatomic features such as the feeding arteries arising from the vertebrobasilar system, and the tectal and superior cerebellar draining veins into the straight sinus.
Statistics
Correlations between independent variables and the occurrence of VAE were analyzed using the Fisher, Chi square, and Mann-Whitney U test. P values <0.05 were considered significant. SPSS version 22 (SPSS Inc., Chicago, IL, USA) was used.
RESULTS
Participants and descriptive data
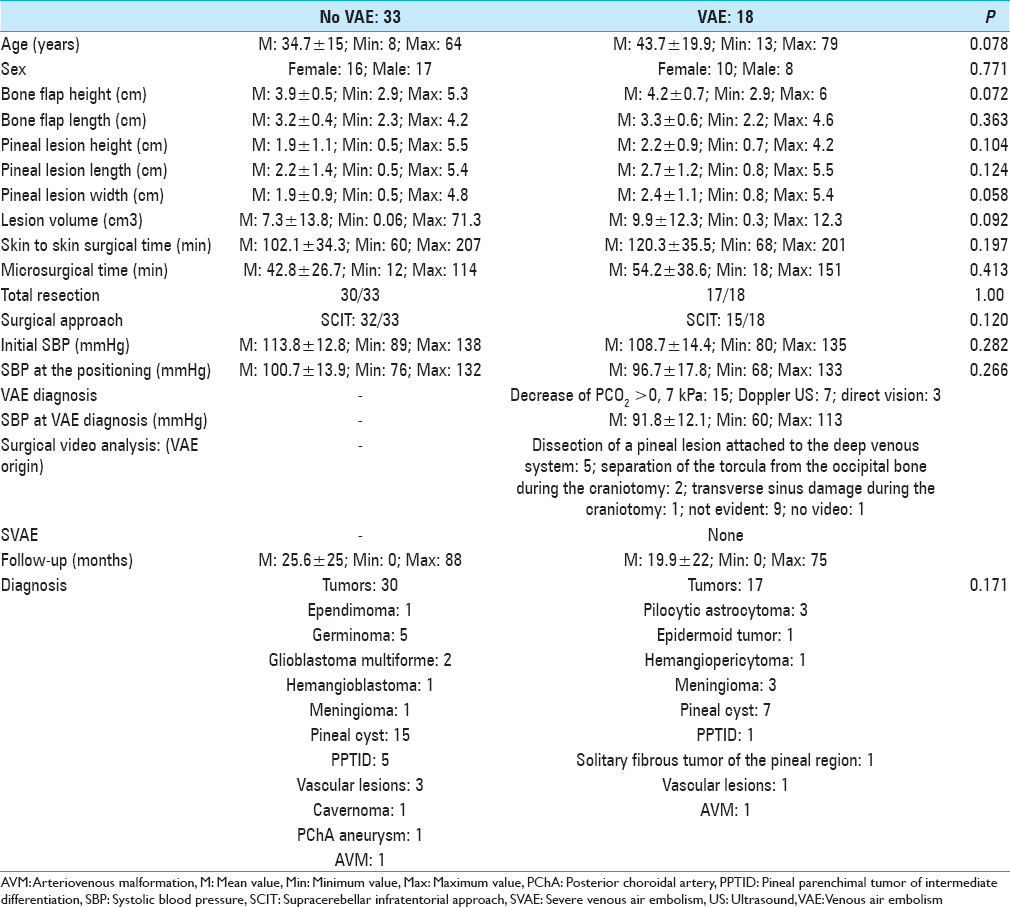
Sixty-one patients with pineal lesions were consecutively operated on by the senior author (JH) between March 2008 and October 2015. Three patients were not operated on in the sitting position. Other three patients were not included due to missing data (anesthetic information, preoperative images, or appropriate follow-up). Four pediatric patients did not use antigravity trousers but elastic bandages, and were excluded from the study as well. Characteristics of the remaining 51 patients are presented in the
Outcome data and main results
The rate of VAE was 35.3% (18 patients). VAEs were diagnosed mainly by monitoring of the end-tidal CO2 (83.33%). Only three cases were recognized by direct vision during the surgery; however, the retrospective surgical video analysis revealed a venous system lesion also in other five patients. In nine patiens with no evident venous damage, we highly suspected the presence of microvenous lesions due to the vascular manipulation during the dissection of the pineal lesion and/or small openings of the venous sinuses during the dura opening. No analyzed surgical variable was associated with the prescence of VAE [
Severe VAE was absent in our series. However, three adult patients (respectively harboring a pineal cyst, a solitary fibrous tumor, and an arteriovenous malformation) presented a very short period (one measurement in a 5-min interval) of low systolic blood pressure associated with VAE, which was rapidly corrected with vasoactives and fluid filling. Mean arterial pressure was over 50 mmHg in two cases, and 45 in other one. No change in the ventilation during the surgery, no inmediate nor late postoperative complications were observed in these patients.
On the other hand, a patient harboring an epidermoid tumor with a damaged dominant right transverse sinus, which was repeared by direct suturing, presented signs of minor air embolism without consistent reduction of her blood pressure.
In our series three patients had recurrent lesions: only a patient with a recurrent hemangiopericytoma presented a VAE.
As a part of the sitting position protocol, when VAE was suspected, an immediate reaction based on a good teamwork and a proper communication between the anesthesiologist and the surgeon was imperative. The compression of both jugular veins by the anesthesiologist was very effective to find the leak, which was repaired by the surgeon using hemostatic agents or direct suturing. Air aspiration from the central venous catheter was never used.
Postoperative course was uneventful with no complication related to the positioning nor to the use of the antigravity trousers. No cervical spine cord injury, no facial or tongue edema nor peripheral nerve damage were reported.
DISCUSSION
Essential anesthetic considerations and antigravity trousers as well, together with a skillful neurosurgery and an imperative proper teamwork may effectively prevent, the risk of severe VAE during pineal region surgery in the ergonomic “praying-sitting position.”
In a systematic review of craniotomy studies comparing sitting and horizontal positions, the incidence of VAE was respectively 15–45% and 0–12%.[
Previous series from our department reported a rate of minor VAE in patients undergoing pineal lesion removal in sitting position between 19% and 50%, in relation to the considered limit of PCO2 decrease (0.7 kPa or 0.3 kPa). Precordial Doppler is always used as a part of our protocol for the sitting position in Helsinki neurosurgery. In this retrospective study most of the VAEs were diagnosed by a PCO2 decrease. Even if we assume that Doppler ultrasound is more sensitive than PCO2, as reported in the literature, we believe that the changing signal from the Doppler is not so specific. Hence, in our daily clinical practice, VAE is usually reported by the anesthesiologists only when the Doppler changing signal occurs together with an end-tidal PCO2 decrease, or when end-tidal PCO2 falls without any change in Doppler.
Nonetheless, VAE was never associated with simultaneous hemodynamic instability nor with a modification in minute ventilation.[
The incidence of VAE in sitting position may be reduced by adopting a careful surgical technique, as well as by maintaining an optimal right atrial pressure. Classically, intravenous fluids, an antigravity suit, and the application of a positive end-expiratory pressure are used for that.[
However, Giebler et al. observed that the incidence of VAE did not differ between patients undergoing conventional ventilation and those undergoing ventilation with 10 cm H2O of positive end-expiratory pressure.[
In this regard, we conclude that risk for VAE is directly related to an intraoperative accidental venous structures laceration and to a low cardiac preload due to the surgical position.
Hence, as above mentioned, we strongly believe that an effective surgical teamwork cooperation, together with a skillfull neurosurgery and the use of antigravity trousers, is imperative to reduce the risk for VAE and hemodynamic instability.[
Antigravity trousers are commonly used in military airplanes, and they were first used for medical purposes in the 1950s. Compressed air is widely available inside operating theaters: this made easier their use.[
Benefits of antigravity trousers in sitting position for neurosurgery were early recognized.[
In our department we use the antigravity trousers since 1997. We usually inflate them at a pressure of 40 mmHg, and no complication occurred so far.[
The average microsurgical time of our surgical series was 48 ± 32 min, and the average surgical skin to skin time was 109 ± 35 min.
CONCLUSIONS
The risks of severe VAE during pineal region surgery in the “praying-sitting position” may be effectively prevented by some essential anesthetic considerations and by the use of antigravity trousers together with a skillful neurosurgery and an imperative proper teamwork.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Black S, Ockert DB, Oliver WC, Cucchiara RF. Outcome following posterior fossa craniectomy in patients in the sitting or horizontal positions. Anesthesiology. 1988. 69: 49-56
2. Brodrick PM, Ingram GS. The antigravity suit in neurosurgery. Cardiovascular responses in seated neurosurgical patients. Anaesthesia. 1988. 43: 762-65
3. Choque-Velasquez J, Colasanti R, Baffigo-Torre V, Sacieta-Carbajo LE, Olivari-Heredia J, Falcon-Lizaraso Y. Developing the First Highly Specialized Neurosurgical Center of Excellence in Trujillo, Peru: Work in Progress-Results of the First Four Months. World Neurosurg. 2017. 102: 334-9
4. Choque-Velasquez J, Colasanti R, Fotakopoulos G, Elera-Florez H, Hernesniemi J. Seven Cerebral Aneurysms: A Challenging Case from the Andean Slopes Managed with 1-Stage Surgery. World Neurosurg. 2017. 97: 565-70
5. Choque-Velasquez J, Colasanti R, Jahromi BR, Hernesniemi J. “Squeeze Maneuver” Assisted by Indocyanine Green Videoangiography: Simple Technique to “Resuscitate” Partially Occluded Bridging Veins During Microneurosurgical Operations. World Neurosurg. 2017. 97: 225-30
6. Choque-Velasquez J, Colasanti R, Jahromi BR, Rafei A, Sharafeddin F, Hernesniemi J. Short-Burst Bipolar Coagulation for Repairing Partially Damaged Brain Arteries Preserving Their Flow: Technical Note. World Neurosurg. 2016. 93: 324-9
7. Choque-Velasquez J, Colasanti R, Resendiz-Nieves JC, Jahromi BR, Kozyrev DA, Thiarawat P. Supracerebellar infratentorial paramedian approach in Helsinki Neurosurgery: Cornerstones of a safe and effective route to the pineal region. World Neurosurg. 2017. 105: 534-42
8. Choque-Velasquez J, Colasanti R, Resendiz-Nieves J, Gonzáles-Echevarría K, Raj R, Rezai Jahromi B. Praying sitting position for pineal region surgery: An efficient variant of a classic positioning in Neurosurgery. World Neurosurg. 2018. p.
9. Choque-Velasquez J, Kozyrev DA, Colasanti R, Thiarawat P, Intarakhao P, Jahromi BR. The open access video collection project “Hernesniemi's 1001 and more microsurgical videos of Neurosurgery”: A legacy for educational purposes. Surg Neurol Int. 2017. 8: 188-
10. Dohn DF, Gardner WJ. The antigravity suit (G-suit) in surgery; control of blood pressure in the sitting position and in hypotensive anesthesia. J Am Med Assoc. 1956. 162: 274-6
11. Duke DA, Lynch JJ, Harner SG, Faust RJ, Ebersold MJ. Venous air embolism in sitting and supine patients undergoing vestibular schwannoma resection. Neurosurgery. 1998. 42: 1282-6
12. Fathi A-R, Eshtehardi P, Meier B. Patent foramen ovale and neurosurgery in sitting position: Asystematic review. Br J Anaesth. 2009. 102: 588-96
13. Gale T, Leslie K. Anaesthesia for neurosurgery in the sitting position. J Clin Neurosci. 2004. 11: 693-6
14. Ganslandt O, Merkel A, Schmitt H, Tzabazis A, Buchfelder M, Eyupoglu I. The sitting position in neurosurgery: Indications, complications and results. a single institution experience of 600 cases. Acta Neurochir (Wien). 2013. 155: 1887-93
15. Giebler R, Kollenberg B, Pohlen G, Peters J. Effect of positive end-expiratory pressure on the incidence of venous air embolism and on the cardiovascular response to the sitting position during neurosurgery. Br J Anaesth. 1998. 80: 30-5
16. Harrison EA, Mackersie A, McEwan A, Facer E. The sitting position for neurosurgery in children: Areview of 16 years’ experience. Br J Anaesth. 2002. 88: 12-7
17. Hernesniemi J, Romani R, Albayrak BS, Lehto H, Dashti R, Ramsey C. Microsurgical management of pineal region lesions: Personal experience with 119 patients. Surg Neurol. 2008. 70: 576-83
18. Iacoangeli M, Colasanti R, Esposito D, Di Rienzo A, di Somma L, Dobran M. Supraorbital subfrontal trans-laminar endoscope-assisted approach for tumors of the posterior third ventricle. Acta Neurochir (Wien). 2017. 159: 645-54
19. Jadik S, Wissing H, Friedrich K, Beck J, Seifert V, Raabe A. A standardized protocol for the prevention of clinically relevant venous air embolism during neurosurgical interventions in the semisitting position. Neurosurgery. 2009. 64: 533-8
20. Lehecka M, Laakso A, Hernesniemi J.editors. Helsinki microneurosurgery basics and tricks. Helsinki: Druckerei Hohl GmbH and Co. KG; 2011. p.
21. Lindroos A-CB, Niiya T, Silvasti-Lundell M, Randell T, Hernesniemi J, Niemi TT. Stroke volume-directed administration of hydroxyethyl starch or Ringer's acetate in sitting position during craniotomy. Acta Anaesthesiol Scand. 2013. 57: 729-36
22. Lindroos A-C, Niiya T, Randell T, Romani R, Hernesniemi J, Niemi T. Sitting position for removal of pineal region lesions: The Helsinki experience. World Neurosurg. 2010. 74: 505-13
23. Luostarinen T, Lindroos A-C, Niiya T, Silvasti-Lundell M, Schramko A, Hernesniemi J. Prone Versus Sitting Position in Neurosurgery-Differences in Patients’ Hemodynamic Management. World Neurosurg. 2017. 97: 261-6
24. Matjasko J, Petrozza P, Cohen M, Steinberg P. Anesthesia and surgery in the seated position: Analysis of 554 cases. Neurosurgery. 1985. 17: 695-702
25. Porter JM, Pidgeon C, Cunningham AJ. The sitting position in neurosurgery: Acritical appraisal. Br J Anaesth. 1999. 82: 117-28
26. Randall P, Banks J, Little RA. Medical (military) anti-shock trousers--a short review. Arch Emerg Med. 1984. 1: 39-51
27. Rushatamukayanunt P, Seanho P, Muangman S, Raksakietisak M. Severe Venous Air Embolism Related to Positioning in Posterior Cranial Fossa Surgery in Siriraj Hospital. J Med Assoc Thai. 2016. 99: 511-6
28. Sharafeddin F, Hafez A, Lehecka M, Raj R, Colasanti R, Rafiei A. A5 segment aneurysm of the anterior cerebral artery, imbedded into the body of the corpus callosum: A case report. Surg Neurol Int. 2017. 8: 18-
29. Slbin MS, Babinski M, Maroon JC, Jannetta PJ. Anesthetic management of posterior fossa surgery in the sitting position. Acta Anaesthesiol Scand. 1976. 20: 117-28
30. Standefer M, Bay JW, Trusso R. The sitting position in neurosurgery: Aretrospective analysis of 488 cases. Neurosurgery. 1984. 14: 649-58
31. Velasquez JC, Lau J, Kozyrev D, Sharafeddin F, Colasanti R, Luostarinen T. Clean, fast and preserving normal anatomy: “The Helsinki revolution” in microneurosurgery. J Neurosurg Sci. 2016. 60: 44-53
32. Yonekawa Y. [Operative neurosurgery: Personal view and historical backgrounds (8) suboccipital craniotomy-sitting position-linear incision]. No Shinkei Geka. 2011. 39: 789-809
33. Young ML, Smith DS, Murtagh F, Vasquez A, Levitt J. Comparison of surgical and anesthetic complications in neurosurgical patients experiencing venous air embolism in the sitting position. Neurosurgery. 1986. 18: 157-61