- Department of Neurosurgery, University of Minnesota, United States.
- Department of Neurosurgery, Hennepin County Medical Center, Minneapolis, Minnesota, United States.
Correspondence Address:
Shiwei Huang, Department of Neurosurgery, University of Minnesota, Minneapolis, Minnesota, United States.
DOI:10.25259/SNI_850_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Shiwei Huang1, David Freeman1, Walter Galicich2, Thomas Bergman2. Ventral cervico-thoracic meningeal cyst resulting in myelopathy: Case report and literature review. 11-Oct-2021;12:510
How to cite this URL: Shiwei Huang1, David Freeman1, Walter Galicich2, Thomas Bergman2. Ventral cervico-thoracic meningeal cyst resulting in myelopathy: Case report and literature review. 11-Oct-2021;12:510. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=11173
Abstract
Background: Spinal meningeal (dural) cysts rarely cause spinal cord compression and/or myelopathy.
Case Description: A 38-year-old male presented with 6 weeks of worsening bilateral lower extremity paresthesias and an unsteady gait. Notably, the patient was involved in a snowmobile accident 7 years ago that resulted in trauma to his thoracic spine for which he had undergone a corpectomy and posterior fusion. A full spine MRI was obtained to evaluate his new paresthesias and myelopathy, which revealed a large extra-axial fluid collection consistent with a meningeal cyst extending from C2 to T4. This caused severe spinal cord compression, maximal at the T1-3 level. The patient underwent a T1-3 laminectomy initially accompanied by partial cyst resection/ drainage, but ultimately he returned and required a subsequent cystoperitoneal shunt. Following the final surgery, the patient’s symptoms gradually resolved over 6 months postoperatively.
Conclusion: Spinal meningeal cysts rarely cause back pain and/or neurological symptoms. MRI is the diagnostic study of choice for defining this entity. Operative intervention must be tailored to the symptoms, location, extent, and type of the cyst. If cysts recur after partial resection and drainage, cystoperitoneal shunt placement is warranted.
Keywords: Cystoperitoneal shunt, Myelopathy, Spinal meningeal cyst
INTRODUCTION
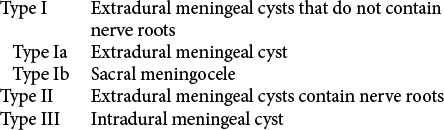
Spinal meningeal cysts are deverticula of the spinal meninges, nerve root sheath, or arachnoid. There are three types: Type I - extradural meningeal cyst without nerve root fibers, Type II – extradural meningeal cyst with spinal nerve fibers, Type III intradural meningeal cysts [
CASE DESCRIPTION
Seven years prior to the presentation, the patient had undergone a T12 corpectomy with T11-L1 posterior fusion following a snowmobile accident that resulted in a fracture-dislocation at T12. Now at age of 38 years, he newly presented with a 6-weeks of progressive dysesthesias from the waist down and a mild paraparesis/unsteady gait. On examination, he had subtle left leg weakness (attributed to his old trauma), but also reported newly decreased sensation to fine touch, pain, and temperature sensation from T5 level downward.
Diagnostic studies
The electromyogram showed a chronic peripheral neuropathy and left peroneal mononeuropathy, which did not fully explain the patient’s symptoms. However, the full spine MRI revealed a large extra-axal fluid collection consistent with an arachnoid cyst extending from C2 to T4 that resulted in spinal cord compression, maximal between the T1-3 level [
Figure 1:
(a) Pre-operative imaging sagittal T2-weighted magnetic resonance image (MRI) of the thoracolumbar spine revealed a large ventral extra-axial cystic lesion causing spinal canal stenosis worst at T1-3. (b) Preoperative imaging sagittal T2-weighted MRI of the cervicothoracic spine revealed the cystic lesion extends to C2 level.
Surgery
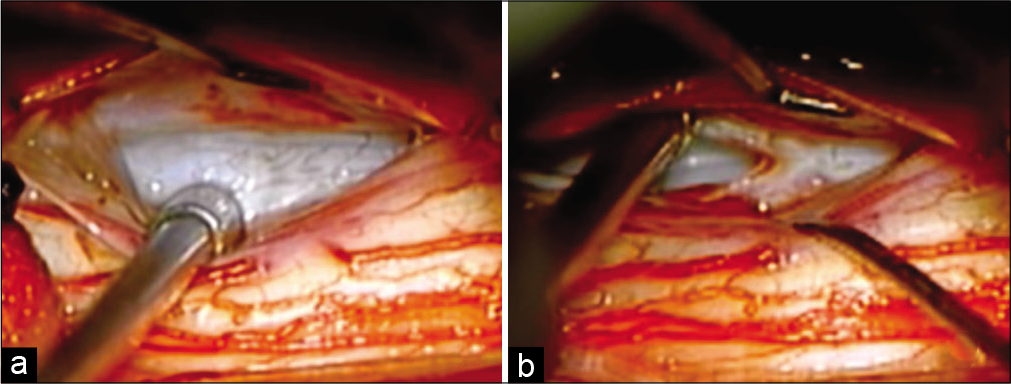
The patient initially underwent a T1-3 laminectomy for cyst resection. Once the dura was opened and the spinal cord was mobilized laterally, a few arachnoid bands were encountered and lysed, but no clear arachnoid cyst was visualized [
Post-operative course
Post-operatively, the patient had improvements in his symptoms over the next 3 days and was discharged.
Nevertheless, the patient returned 2 months later with recurrent symptoms. The repeat MRI demonstrated recurrence of the fluid collection. As the prior laminectomy with cyst fenestration had failed, the repeat surgery included a cystoperitoneal shunt placement [
DISCUSSION
Etiology of spinal meningeal cysts
Spinal meningeal cysts are defined as diverticula or pouches of arachnoid or dura that result in CSF accumulation. Their etiology is unknown. One popular proposed mechanism is that a small defect, either congenital or traumatic, results in a cleft in the inner layer of the dura with the outer layer remaining intact. CSF fills the resultant “potential space” between the inner and outer dural layers. Hydrostatic dissection by CSF pulsations subsequently enlarges this potential space and forms a meningeal cyst.[
Spinal meningeal cyst types
There are three types of spinal meningeal cyst classification (Type 1a/Ib, II, and III) [
Location of meningeal cysts
The majority of meningeal cysts are discovered accidentally. Approximately 80% of the cysts occur in the lower thoracic and/or lumbar spinal, and only 20% occur ventrally.[
MR diagnosis of meningeal cysts
MR usually reveals the fluid in these cysts is consistent with CSF, although it can be more hyperintense than CSF on T2 due to the lack of CSF pulsations.[
Neurological symptoms of meningeal cysts
Most meningeal cysts are asymptomatic, but when symptoms occur the most frequent symptoms are low back pain followed by radiculopathy. Very rarely do these lesions cause cord compression resulting in myelopathy, and rare cases of quadriplegia or paraplegia have been reported.[
Management of meningeal cysts
The treatment of meningeal cysts may include fenestration, shunting (i.e., cystoperitoneal shunts), or complete surgical excision. Although patients may have initial symptoms relief following fenestration or decompression of the cysts, many will experience recurrence of symptoms. Management of recurrent meningeal cysts includes cyst shunting to ensure long-term CSF outflow from the cyst.[
CONCLUSION
Spinal meningeal cysts rarely cause back pain and/or myelopathy, especially in the cervical-thoracic region. Notably, these lesions may be refractory to conventional surgical fenestration techniques and often warrant cystoperitoneal shunting.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Aoyama T, Miyaoka Y, Ogiwara T, Ito K, Seguchi T, Hongo K. Long segment spinal dural cyst: A case report. World Neurosurg. 2016. 88: 686.e13-7
2. Kunz U, Mauer UM, Waldbaur H. Lumbosacral extradural arachnoid cysts: Diagnostic and indication for surgery. Eur Spine J. 1999. 8: 218-22
3. Nabors MW, Pait TG, Byrd EB, Karim NO, Davis DO, Kobrine AI. Updated assessment and current classification of spinal meningeal cysts. J Neurosurg. 1988. 68: 366-77
4. Netra R, Min L, Hui MS, Wang JC, Bin Y, Ming Z. Spinal extradural meningeal cysts: An MRI evaluation of a case series and literature review. J Spinal Disord Tech. 2011. 24: 132-6
5. Prevedello DM, Tatsui CE, Koerbel A, Grande CV, Cordeiro JG, Araujo JC. Ventral extradural spinal meningeal cyst causing cord compression: Neurosurgical treatment. Arq Neuropsiquiatr. 2005. 63: 855-8
6. Sato K, Nagata K, Sugita Y. Spinal extradural meningeal cyst: Correct radiological and histopathological diagnosis. Neurosurg Focus. 2002. 13: ecp1