- Department of Neurosurgery, St. Marianna University School of Medicine, Kanagawa, Japan
Correspondence Address:
Hidemichi Ito
Department of Neurosurgery, St. Marianna University School of Medicine, Kanagawa, Japan
DOI:10.4103/2152-7806.196379
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Hidemichi Ito, Ryotaro Miyano, Taigen Sase, Daisuke Wakui, Takashi Matsumori, Hiroshi Takasuna, Kotaro Oshio, Yuichiro Tanaka. Outflow occlusion with A3–A3 anastomosis for a doughnut-shaped partially thrombosed giant A2 aneurysm. 21-Dec-2016;7:
How to cite this URL: Hidemichi Ito, Ryotaro Miyano, Taigen Sase, Daisuke Wakui, Takashi Matsumori, Hiroshi Takasuna, Kotaro Oshio, Yuichiro Tanaka. Outflow occlusion with A3–A3 anastomosis for a doughnut-shaped partially thrombosed giant A2 aneurysm. 21-Dec-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/outflow-occlusion-with-a3-a3-anastomosis-for-a-doughnutshaped-partially-thrombosed-giant-a2-aneurysm/
Abstract
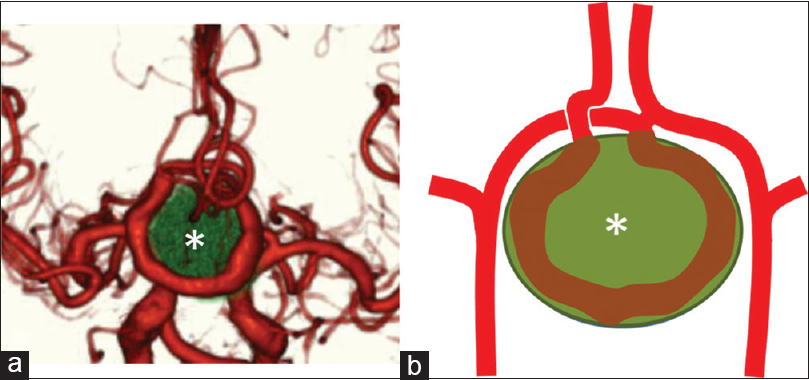
Background:A doughnut-shaped aneurysm, which is defined as a round-shaped aneurysm composed of an intraluminar thrombus and marginal parent artery, is an extremely uncommon subtype of partially thrombosed giant aneurysms. Surgical treatment of this characteristic aneurysm is technically challenging.
Case Description:We report a rare case of a 79-year-old man with a symptomatic doughnut-shaped giant aneurysm at the A2 portion, which was successfully treated by outflow occlusion with an A3–A3 side-to-side anastomosis. Postoperative angiograms demonstrated no filling of the doughnut-shaped aneurysm and perfusion in the distal right anterior cerebral artery territory via the anastomosis. Follow-up magnetic resonance imaging 1 year after the surgery demonstrated significant diminution of the aneurysm.
Conclusions:Outflow occlusion with distal revascularization could be an effective surgical option for such a unique aneurysm. To the best of our knowledge, this is the first report of outflow occlusion as a therapy for doughnut-shaped aneurysms.
Keywords: Anterior cerebral artery, bypass surgery, giant aneurysm, outflow occlusion, partially thrombosed aneurysm
INTRODUCTION
Giant aneurysms, those larger than 25 mm in diameter, are relatively uncommon and are often accompanied by thrombosis. Among such lesions, giant serpentine aneurysms have been described as a rare subcategory of partially thrombosed giant aneurysms.[
CASE REPORT
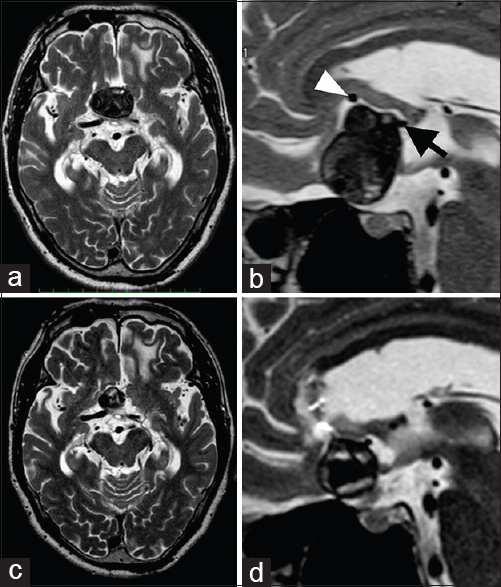
A 79-year-old man with no significant medical history presented with blurred vision for a few months. Native and contrast-enhanced magnetic resonance imaging (MRI) showed a heterogeneous round mass compressing the bilateral optic nerves and rectal gyri, which was 39 mm in maximum diameter, in the anterior interhemispheric fissure [Figure
Figure 1
Preoperative axial (a) and mid-sagittal (b) T2-weighted images obtained on admission demonstrating a giant round mass at the frontal interhemispheric fissure, which was 39 mm in diameter. This lesion was largely thrombosed but incorporated flow void signals, which suggested a partially thrombosed aneurysm. Inflow (black arrow) and outflow (white arrowhead) arteries were located behind and at the upper surface of the aneurysm, respectively. Postoperative axial (c) and mid-sagittal (d) T2-weighted images obtained 1 year postoperatively showing significant reduction of the aneurysm
Figure 3
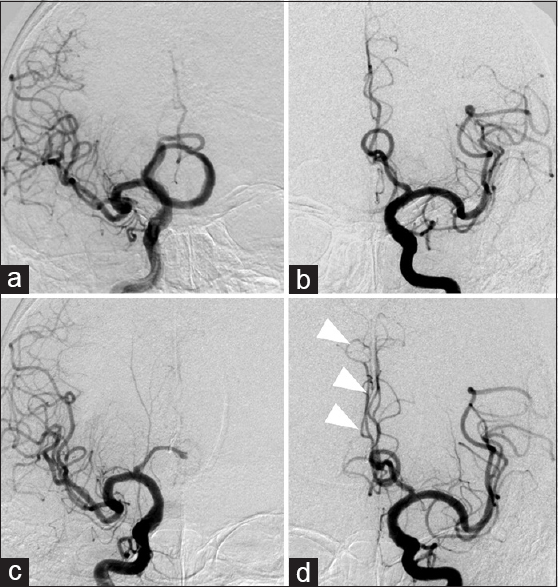
Preoperative right (a) and left (b) internal carotid angiograms demonstrating a giant aneurysm as a doughnut-shaped structure. Postoperative right (c) and left (d) internal carotid angiograms on the day after surgery revealing no filling of the aneurysm and right peripheral anterior cerebral arteries perfused by contralateral anterior cerebral arteries (arrowheads)
DISCUSSION
A giant serpentine aneurysm is defined as a partially thrombosed giant aneurysm with tortuous vascular channels forming a serpentine pathway with separate inflow and outflow tracts.[
Optimal management of giant serpentine and doughnut-shaped aneurysms has not yet been established. In contrast to the usual saccular aneurysm, giant serpentine and doughnut-shaped aneurysms have separate inflow and outflow vessels; therefore, clipping the aneurysmal neck is unsuitable. For such cases, trapping of the involved segment with or without distal bypass is recommended. Proximal occlusion is also considered to be suitable for cases with surgical difficulty of trapping because proximal occlusion for aneurysms is believed to reduce the hemodynamic burden of the aneurysm, promote complete thrombosis in the aneurysm sac, and reduce the size of the aneurysm.[
Outflow occlusion for the management of partially thrombosed aneurysms has been described in some reports.[
Recently, several groups have reported the efficacy and feasibility of bypass technique for the complex distal ACA aneurysm.[
In the present case, because the patient presented with visual symptoms due to aneurysmal mass effect, the best treatment might be aneurysm trapping with distal revascularization and aneurysmectomy. However, we anticipated that damage to the frontal lobe could not be avoided if occlusion of the inflow vessel was attempted in such a deep and narrow surgical field. Therefore, we chose outflow occlusion with an A3–A3 side-to-side anastomosis.
CONCLUSIONS
We experienced an extremely rare case of a doughnut-shaped giant aneurysm causing a mass effect. Surgical treatment of such an aneurysm is technically challenging. To the best of our knowledge, this is the first reported case of this entity that was successfully treated by outflow occlusion with distal vascular reconstruction.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Day AL, Gaposchkin CG, Yu CJ, Rivet DJ, Dacey RG. Spontaneous fusiform middle cerebral artery aneurysms: Characteristics and a proposed mechanism of formation. J Neurosurg. 2003. 99: 228-40
2. Dunn GP, Gerrard JL, Jho DH, Ogilvy CS. Surgical treatment of a large fusiform distal anterior cerebral artery aneusyrm with in situ end-to-side A3–A3 bypass graft and aneurysml trapping: Case report and review of the literature. Neurosurgery. 2011. 68: E587-91
3. Hoh BL, Putman CM, Budzik RF, Carter BS, Oglivy CS. Combined surgical and endovascular techniques of flow alteration to treat fusiform and complex wide-necked intracranial aneurysms that are unsuitable for clipping or coil embolization. J Neurosurg. 2001. 95: 24-35
4. Horowitz MB, Yonas H, Jungreis C, Hung TK. Management of a giant middle cerebral artery fusiform serpentine aneurysm with distal clip application and retrograde thrombosis: Case report and review of the literature. Surg Neurol. 1994. 41: 221-5
5. Park ES, Ahn JS, Park JC, Kwon DH, Kwun BD, Kim CJ. STA-ACA bypass using the contralateral STA as an interposition graft for the treatment of complex ACA aneurysms: Report of two cases and a review of the literature. Acta Neurochir. 2012. 154: 1447-53
6. Rosta L, Battaglia R, Pasqualin A, Beltramello A. Italian cooperative study on giant intracranial aneurysms: 2. Radiological data. Acta Neurochir Suppl. 1998. 42: 53-9
7. Sanai N, Zador Z, Lawton MT. Bypass surgery for complex brain aneurysms: An assessment of intracranial-intracranial bypass. Neurosurgery. 2009. 65: 670-83
8. Segal HD, McLaurin RL, Giant serpentine aneurysm. Report of two cases. J Neurosurg. 1977. 46: 115-20