- Department of Neurosurgery, Hospital Municipal Pimentas Bonsucesso, Guarulhos, São Paulo, Brazil
Correspondence Address:
Juliano N. Navarro
Department of Neurosurgery, Hospital Municipal Pimentas Bonsucesso, Guarulhos, São Paulo, Brazil
DOI:10.4103/2152-7806.184581
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Navarro JN, Alves RV. Postoperative cerebral myiasis: A rare cause of wound dehiscence in developing countries. Surg Neurol Int 23-Jun-2016;7:69
How to cite this URL: Navarro JN, Alves RV. Postoperative cerebral myiasis: A rare cause of wound dehiscence in developing countries. Surg Neurol Int 23-Jun-2016;7:69. Available from: http://surgicalneurologyint.com/surgicalint_articles/postoperative-cerebral-myiasis-a-rare-cause-of-wound-dehiscence-in-developing-countries/
Abstract
Background:Cerebral myiasis is a rare parasitic disease, especially in postoperative neurological surgery.
Case Description:We report a case of postoperative myiasis in a patient who underwent a craniotomy for resection of metastatic melanoma, evolving with wound dehiscence due to myiasis in the operative wound.
Conclusion:Myiasis infestation should be a differential diagnosis of surgical wound dehiscence, particularly when the classic signs of inflammation are not present and computed tomography of the brain shows signs suggestive of this disease entity.
Keywords: Myiasis, neurosurgical procedure, postoperative period
INTRODUCTION
Myiasis is an infection caused by a fly larva, usually occurring in tropical and subtropical areas. There are many ways for flies to transmit their larvae to human beings. Some flies attach their eggs on mosquitoes and wait for them to bite a human host, and then the larvae enter through these lesions.[
Other flies’ larvae burrow into the skin. They can enter the skin through people's bare feet when they walk through soil containing fly eggs or attach themselves to people's clothes and then burrow into their skin. Some flies put their larvae on or near a wound or sore, depositing eggs in sloughing-off dead tissue.[
Human cerebral myiasis is an exceedingly rare condition and is almost never encountered by physicians.[
Jan et al. described intranasal myiasis after a transnasal skull base surgery.[
CASE DESCRIPTION
A 36-year-old patient was taken into the emergency room with an acute decreased level of consciousness. On clinical examination, he was comatose, had 8 points on the Glasgow Coma Scale, no apparent focal deficit, and right inguinal lymphadenomegaly. His wife reported that he had been subjected to the treatment of cutaneous melanoma at another hospital for approximately 1 year.
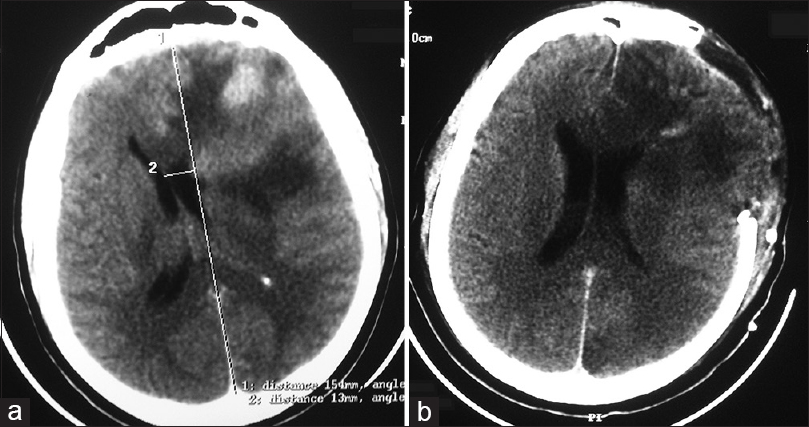
Emergency brain computed tomography (CT) showed the left frontal tumor lesion with significant mass effect [
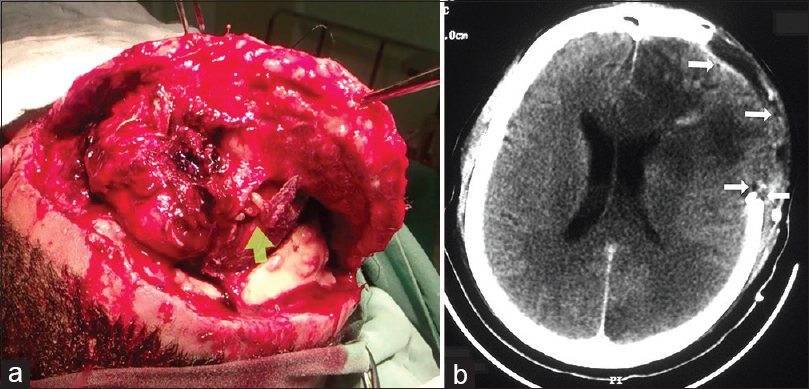
On the 7th postoperative day, his level of awareness did not improve, and the wound became dehiscent [
Faced with unexpected intraoperative findings, the postoperative CT was revised. Hypodense small, rounded, and regular images were identified at the surgical site [
He developed partial neurological improvement and received medical release with a Prognostic Glasgow Score of 2. Metastatic melanoma was the pathological diagnosis of the previously resected tumor.
We believe that the last infestation route, cited earlier in this article, has occurred in our case (flies lay their larvae in or near an operative wound).
CONCLUSION
Although rare, brain myiasis should be a differential diagnosis of surgical wound dehiscence in developing countries. This differential diagnosis should be remembered, particularly when the classic signs of inflammation are not present and brain CT shows hypodense round and regular lesions on imaging.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Video Available on: www.surgicalneurologyint.com
References
1. Last accessed on 2016 Feb 01. Available from: www.cdc.gov/parasites/myiasis .
2. Cheshier SH, Bababeygy SR, Higgins D, Parsonnet J, Huhn SL. Cerebral myiasis associated with angiosarcoma of the scalp: Case report. Neurosurgery. 2007. 61: E167-
3. Fidalgo LE, López-Beceiro AM, Vila-Pastor M, Martínez-Carrasco C, Barreiro-Vázquez JD, Pérez JM. Use of computed tomography as a non-invasive method for diagnosing cephenemyiosis in roe deer (Capreolus capreolus). Med Vet Entomol. 2015. 29: 110-3
4. Jan TA, Redjal N, Walcott BP, Sheth SA. Intranasal myiasis: A rare complication of transnasal skull base surgery. J Clin Neurosci. 2013. 20: 1178-80
5. Terterov S, Taghva A, MacDougall M, Giannotta S. Posttraumatic human cerebral myiasis. World Neurosurg. 2010. 73: 557-9