- Department of Orthopedic Surgery, Akita University Graduate School of Medicine, 1-1-1, Hondo, Akita 010-8543, Japan.
DOI:10.25259/SNI_409_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Naohisa Miyakoshi, Michio Hongo, Yuji Kasukawa, Yoshinori Ishikawa, Daisuke Kudo, Yoichi Shimada. Cervical meningioma resection including the inner dura through an open-door laminoplasty using hydroxyapatite spacers: A case report. 02-Oct-2020;11:317
How to cite this URL: Naohisa Miyakoshi, Michio Hongo, Yuji Kasukawa, Yoshinori Ishikawa, Daisuke Kudo, Yoichi Shimada. Cervical meningioma resection including the inner dura through an open-door laminoplasty using hydroxyapatite spacers: A case report. 02-Oct-2020;11:317. Available from: https://surgicalneurologyint.com/surgicalint-articles/10305/
Abstract
Background: The ideal surgery for spinal cord tumors is complete resection to prevent recurrence. However, it should be accomplished safely/effectively without risking increased morbidity. Here, we report a cervical meningioma that was totally resected, including the inner dura, through a laminoplasty performed with hydroxyapatite (HA) spacers.
Case Description: A 61-year-old Asian male presented with a symptomatic intradural extramedullary C4-C6 cervical meningioma. At surgery, this required resection of the inner dural layer through an open-door laminoplasty. Preservation of the outer dural layer facilitated a watertight closure and the avoidance of a postoperative cerebrospinal fluid (CSF) fistula. Notably, the laminoplasty utilized HA spacers which were magnetic resonance (MR) compatible allowing for future follow-up studies to evaluate for tumor recurrence. At 5-year follow-up, the tumor had not recurred, the patient was asymptomatic, and alignment was maintained.
Conclusion: Gross total resection of an intradural extramedullary C4-C6 cervical meningioma was performed with removal of just the inner dural layer. Preservation of the outer dural layer allowed for a watertight closure and the avoidance of a postoperative CSF leak. Further, laminoplasty using HA spacers allowed for successful tumor resection, adequate fusion/stabilization, while not interfering with future MR studies (e.g., HA MR compatible).
Keywords: Bone union, Cervical spine, Dural layer, Hydroxyapatite spacer, Laminoplasty, Spinal meningioma
INTRODUCTION
The ideal surgery for a cervical intradural extramedullary meningioma is gross total resection, as this avoids tumor recurrence. It is best to resect just the inner layer of dura, so the outer dural layer may be utilized for a watertight closure, thus decreasing the risk of a postoperative cerebrospinal fluid (CSF) fistula. Some cervical meningiomas, as in this case, can be effectively removed through an open-door laminoplasty using hydroxyapatite (HA) spacers; this prevent short-/long-term instability, while preserving magnetic resonance (MR) compatibility.
CASE PRESENTATION
History and examination
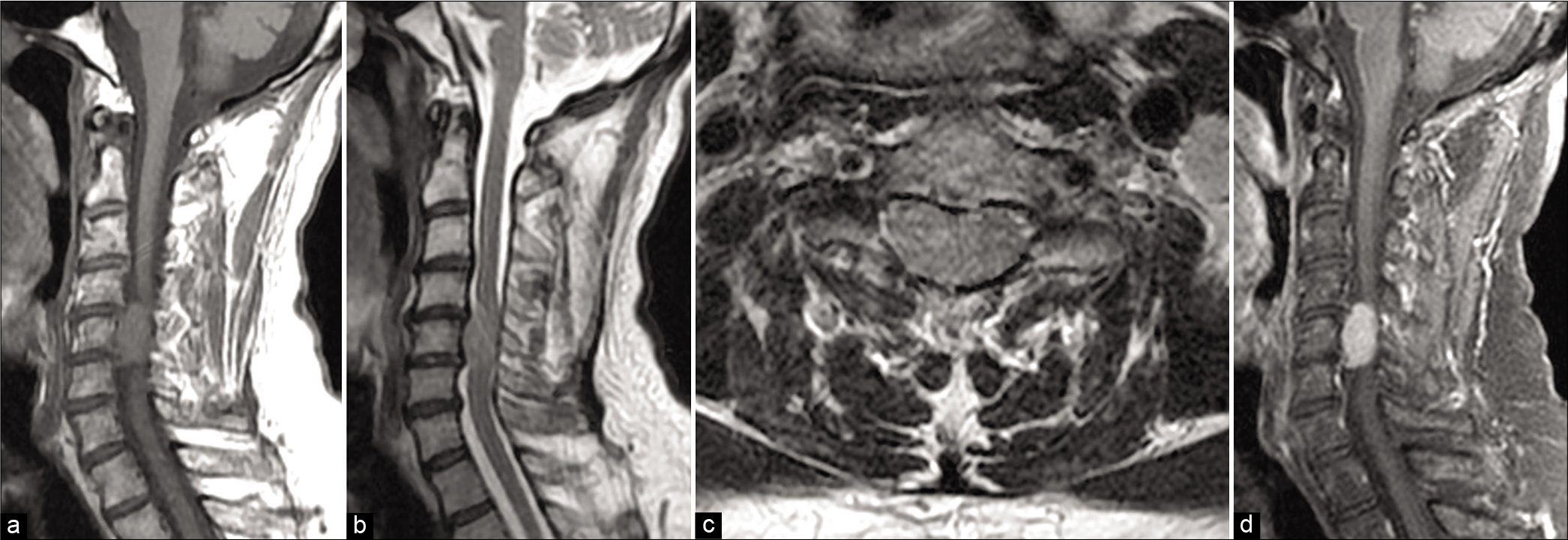
A 61-year-old Asian male presented with a 7-month history of a progressive spastic quadriparesis. The cervical MR imaging demonstrated a large intradural extramedullary anterior tumor at the C4-C6 level that severely compressed the spinal cord [
Figure 1:
(a) Sagittal T1-weighted image of preoperative magnetic resonance imaging (MRI) showing the intradural extramedullary spinal cord tumor anterior to the spinal cord, located from the C4 to C6 level, centered on the C5 level. (b) Sagittal T2-weighted image of the tumor. (c) Axial T2-weighted MRI at the C5 level reveals a large tumor filling the spinal canal, and no boundary with the spinal cord is identifiable. (d) Gadolinium-enhanced sagittal MRI demonstrates a homogeneously enhanced tumor with dural tail sign located anterior to the spinal cord.
Operative technique
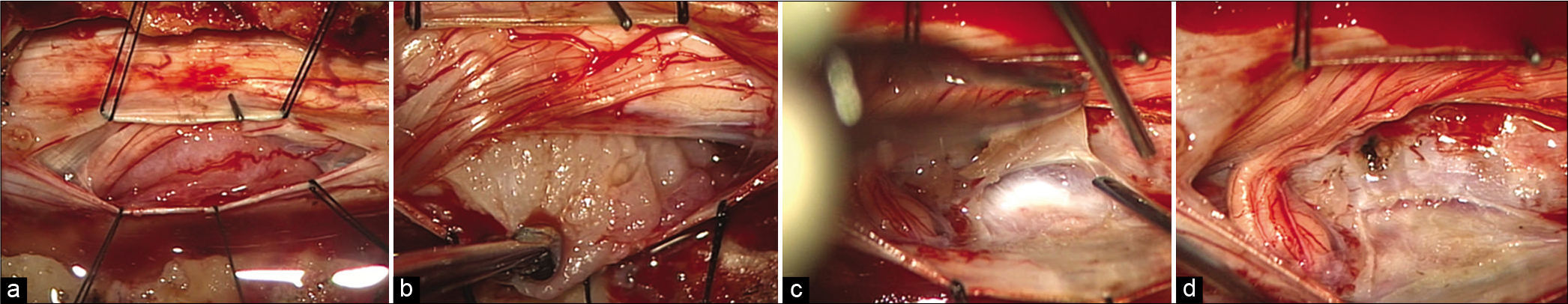
The operative plan was to resect the tumor along with only the inner dural layer through an open-door laminoplasty using HA spacers. Intraoperative monitoring included the utilization of transcranial electrical stimulation of motor evoked potentials. At surgery, the laminoplasty required complete removal of the lateral laminae from C4 to C6 on the right side and hinging the lateral gutter on the left. The tumor was resected from the right side utilizing the cavitational ultrasonic surgical aspirator [
Figure 2:
(a) Intraoperative photographs after opening the dura. The tumor is seen anterior to the spinal cord. Right side of photographs = cranial side. (b) The tumor is excised little by little after dissecting two denticulate ligaments. (c) After complete tumor resection, the inner layer of dura as the base of the tumor is peeled away from the outer layer of dura. (d) The inner layer of the dura was resected.
Postoperative course
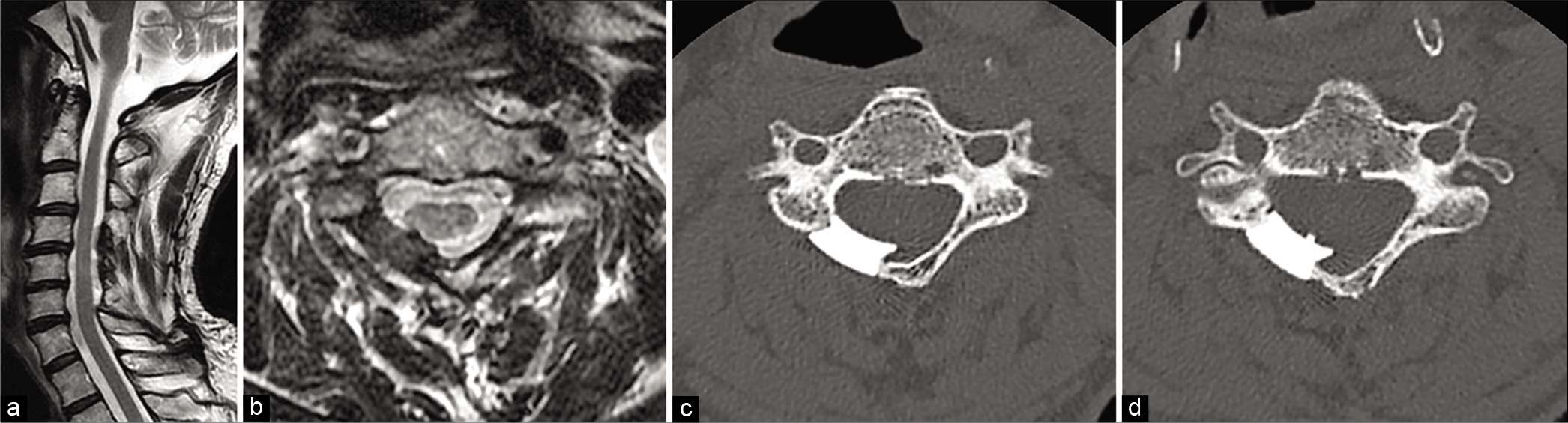
The postoperative course was uneventful; there was no CSF leak, and the patient was asymptomatic within 3 weeks. The 5-year follow-up MR showed no tumor recurrence (HA spacers avoided metal artifact) and stable spinal alignment [
Figure 3:
(a) Postoperative MRI of the cervical spine obtained at 5 years after surgery. Sagittal T2-weighted MRI shows no tumor recurrence with unchanged normal sagittal alignment. (b) Axial T2-weighted MRI at the C5 level shows no tumor recurrence with good visualization inside the spinal canal. (c) Postoperative axial image of computed tomography (CT) at the C4 level demonstrates a newly created spinal canal with hydroxyapatite spacers bonded to host bone. (d) Axial image of CT at C5 level.
DISCUSSION
Conventional surgical procedures for the resection of spinal meningiomas include three major options: (1) complete dural resection with duroplasty, (2) extensive coagulation of the dura without dural resection, or (3) removal of the inner dural layer with preservation of the outer layer to facilitate watertight dural closure. Saito et al. reported three cases of spinal meningioma successfully resected utilizing the third technique; they observed no recurrences with a follow-up duration of 4 months–2 years 10 months.[
Choosing a unique laminoplasty approach with HA fusion
Conventional laminectomies are associated with symptomatic epidural scar and/or postlaminectomy kyphosis.[
CONCLUSION
Here, we reported a C4-C6 cervical meningioma successfully resected along with the inner dural layer through an open-door laminoplasty using MR compatible HA spacers. Five years postoperatively, the MR/CT studies documented no tumor recurrence and adequate HA incorporation/fusion/ stabilization without kyphosis.
Ethical approval
Informed consent was obtained from the patient in the study. All procedures performed in studies involving human participants were conducted in accordance with the ethical standards of the institutional review board.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Fassett DR, Clark R, Brockmeyer DL, Schmidt MH. Cervical spine deformity associated with resection of spinal cord tumors. Neurosurg Focus. 2006. 20: E2
2. Humadi A, Chao T, Dawood S, Tacey M, Barmare A, Freeman B. A meta-analysis of cervical laminoplasty techniques: Are mini-plates superior?. Global Spine J. 2017. 7: 373-81
3. Miyakoshi N, Hongo M, Kasukawa Y, Shimada Y. En-bloc resection of thoracic calcified meningioma with inner dural layer in recapping T-saw laminoplasty: A case report. BMC Surg. 2015. 15: 82
4. Miyakoshi N, Kudo D, Hongo M, Kasukawa Y, Ishikawa Y, Shimada Y. Intradural extramedullary tumor in the stenotic cervical spine resected through open-door laminoplasty with hydroxyapatite spacers: Report of two cases. BMC Surg. 2018. 18: 38
5. Montano N, Trevisi G, Cioni B, Lucantoni C, Della Pepa GM, Meglio M. The role of laminoplasty in preventing spinal deformity in adult patients submitted to resection of an intradural spinal tumor. Case series and literature review. Clin Neurol Neurosurg. 2014. 125: 69-74
6. Ryken TC, Heary RF, Matz PG, Anderson PA, Groff MW, Holly LT. Cervical laminectomy for the treatment of cervical degenerative myelopathy. J Neurosurg Spine. 2009. 11: 142-9
7. Saito T, Arizono T, Maeda T, Terada K, Iwamoto Y. A novel technique for surgical resection of spinal meningioma. Spine (Phila Pa 1976). 2001. 26: 1805-8