- School of Medicine, Wayne State University, Detroit, Michigan, United States,
- Department of Neurosurgery, Detroit Medical Center, Detroit, Michigan, United States.
Correspondence Address:
Richard Justin Garling
Department of Neurosurgery, Detroit Medical Center, Detroit, Michigan, United States.
DOI:10.25259/SNI_621_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Sharath Kumar Anand1, Richard Justin Garling2, Jessica Johns1, Manan Shah2, Parthasarathi Chamiraju2. Intradural extramedullary spinal metastases from uterine carcinosarcoma: A case report. 21-Oct-2020;11:354
How to cite this URL: Sharath Kumar Anand1, Richard Justin Garling2, Jessica Johns1, Manan Shah2, Parthasarathi Chamiraju2. Intradural extramedullary spinal metastases from uterine carcinosarcoma: A case report. 21-Oct-2020;11:354. Available from: https://surgicalneurologyint.com/surgicalint-articles/10341/
Abstract
Background: In recent years, improvements in oncological care have led to an increased incidence of intradural extramedullary spinal metastases (IESMs) attributed to uterine carcinosarcoma (UCS). When such lesions occur, they typically carry a poor prognosis. Here, we have evaluated newer treatments, management strategies, and outcomes for IESM due to UCS.
Case Description: A 59-year-old female with a history of recurrent UCS presented with the new onset of the left lower extremity pain, numbness, and episodic urinary incontinence. When the MR revealed an enhancing intradural extramedullary mass posterior to the L1 vertebral body, she underwent a focal decompressive laminectomy. Although she improved neurologically postoperatively, she succumbed to the leptomeningeal spread of her disease within 2 postoperative months.
Conclusion: Management of IESM due to UCS requires multifaceted, individualized treatment modalities, including neurosurgery, radiation therapy, and medical oncologic management to maximize outcomes.
Keywords: Intradural extramedullary spinal metastases, Malignant mixed Mullerian tumor, Spinal oncology
INTRODUCTION
Intradural extramedullary spinal cord metastases (IESMs) from various types of cancers are uncommon; they are found at autopsy in less than 5% of all cancer patients.[
CASE REPORT
A 59-year-old morbidly obese, African-American female had a history of Stage IIIc recurrent endometrial carcinosarcoma with para-aortic and pelvic lymph node involvement. Over several years, after initial surgery, she required repeated bouts of chemotherapy and radiation therapy. She now, however, newly presented with a 1-month history of numbness of the left vulva, worsening left lower extremity pain/numbness, and episodic urinary incontinence. The thoracic/lumbar MR revealed a 1.4 × 1.8 cm enhancing intradural extramedullary mass inferior to the conus at the L1 and L4-L5 levels. In addition, there was abnormal enhancement of the left-sided intradural nerve roots, and the bilateral, perihilar lung metastases [
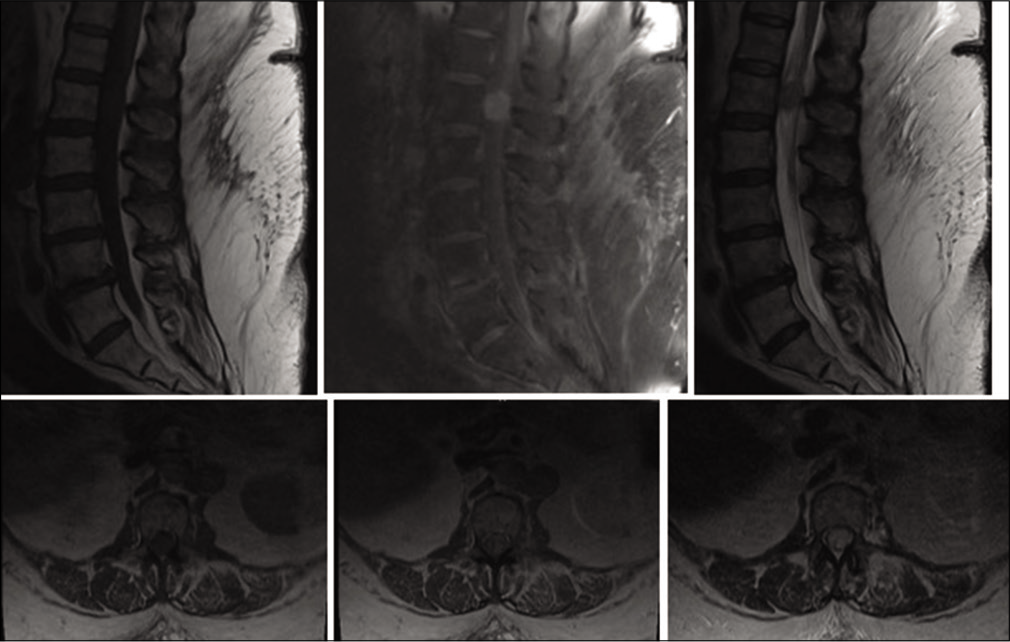
Figure 1:
Preoperative magnetic resonance imaging of the lumbar spine shows the intradural spinal cord lesion. Top row, from left to right: sagittal T1 without contrast, sagittal T1 with contrast, sagittal T2. Bottom row, from left to right: axial T1 without contrast, axial T1 with contrast, axial T2.
Surgery
The patient underwent a T12-L2 laminectomy for gross total resection of the L1 intradural/extramedullary mass; the main aim of surgery was to provide neurological symptomatic relief. Intraoperatively, diffuse carcinomatosis of the cauda equina was observed along with a large lesion located anteroinferior to the conus. Grossly, the tumor appeared vascular and involved multiple, swollen, engorged nerve roots. Dissection ceased (e.g., subtotal resection) once intraoperative electromyographic monitoring showed significant changes while dissecting tumor away from tumor infiltrated, matted nerve roots (e.g., gastrocnemius in particular). The permanent pathology showed a mesenchymal malignant Mullerian mixed tumor (carcinosarcoma) without an epithelial component.
Postoperative course
Although the postoperative MR [
DISCUSSION
Although extramedullary spinal cord tumors account for more than 70% of intradural spinal cord tumors, metastasis to the extramedullary space is exceedingly rare.[
MR study of choice for diagnosing IESM with UCS
MRI has largely replaced computed tomography myelography as the study of choice for diagnosing extramedullary spinal cord lesions. Unfortunately, it is unable to distinguish IESM from primary spinal cord tumors or other non-neoplastic lesions.[
Prognosis of IESM due to UCS
Surgery
The diagnosis of an IESM due to metastatic UCS represents significant systemic disease and thus carries a grave prognosis; the mean survival is estimated to be <1 year.[
However, there are no clear-cut guidelines regarding the use of chemotherapy and/or radiation therapy to treat IESM secondary to UCS.[
CONCLUSION
Intradural extramedullary spinal cord metastases are rare complications of cancer and carry a grave prognosis. Here, a patient with an IESM, due to UCS, and a long-standing prior history of UCS metastatic disease, required lumbar decompressive surgery to achieve symptomatic relief, but succumbed to her metastatic UCS disease within 2 postoperative months.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Akhavan A, Mehrabaniyan MR, Jarahi M, Navabii H. Intradural extramedullary metastasis from papillary carcinoma of thyroid. BMJ Case Rep. 2012. 2012: bcr0220125801
2. Denschlag D, Ulrich UA. Uterine carcinosarcomas-diagnosis and management. Oncol Res Treat. 2018. 41: 675-9
3. Fakih M, Schiff D, Erlich R, Logan TF. Intramedullary spinal cord metastasis (ISCM) in renal cell carcinoma: A series of six cases. Ann Oncol. 2001. 12: 1173-7
4. Galaal K, van der Heijden E, Godfrey K, Naik R, Kucukmetin A, Bryant A. Adjuvant radiotherapy and/or chemotherapy after surgery for uterine carcinosarcoma. Cochrane Database Syst Rev. 2013. 2013: CD006812
5. Hosh M, Antar S, Nazzal A, Warda M, Gibreel A, Refky B. Uterine sarcoma: Analysis of 13,089 cases based on surveillance, epidemiology, and end results database. Int J Gynecol Cancer. 2016. 26: 1098-104
6. Koyama K, Takahashi H, Inoue M, Okawa A, Nakajima A, Sonobe M. Intradural metastasis to the cauda equina found as the initial presentation of breast cancer: A case report. J Med Case Rep. 2019. 13: 220
7. Sherman ME, Devesa SS. Analysis of racial differences in incidence, survival, and mortality for malignant tumors of the uterine corpus. Cancer. 2003. 98: 176-86
8. Traul DE, Shaffrey ME, Schiff D. Part I: Spinal-cord neoplasms-intradural neoplasms. Lancet Oncol. 2007. 8: 35-45
9. Villegas AE, Guthrie TH. Intramedullary spinal cord metastasis in breast cancer: Clinical features, diagnosis, and therapeutic consideration. Breast J. 2004. 10: 532-5
10. Wostrack M, Pape H, Kreutzer J, Ringel F, Meyer B, Stoffel M. Surgical treatment of spinal intradural carcinoma metastases. Acta Neurochir (Wien). 2012. 154: 349-57