- Department of Neurosurgery, Amsterdam University Medical Centers, Amsterdam, Netherlands, Europe.
DOI:10.25259/SNI_311_2020
Copyright: © 2020 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Goedemans T, Verbaan D, Vandertop WP, den Munckhof Pv. Letter to the Editor regarding “Can early cranioplasty reduce the incidence of hydrocephalus after decompressive craniectomy? A meta-analysis”. Surg Neurol Int 18-Jul-2020;11:198
How to cite this URL: Goedemans T, Verbaan D, Vandertop WP, den Munckhof Pv. Letter to the Editor regarding “Can early cranioplasty reduce the incidence of hydrocephalus after decompressive craniectomy? A meta-analysis”. Surg Neurol Int 18-Jul-2020;11:198. Available from: https://surgicalneurologyint.com/surgicalint-articles/10142/
To the editor
Nasi and Dobran published a meta-analysis considering the influence of timing of cranioplasty (CP) after decompressive craniectomy on post CP hydrocephalus.[
Assessing the methodological quality
To report a meta-analysis accurately and completely, it is important to use a guideline, such as PRISMA.[
Heterogeneity among studies
The authors’ finding that early CP in TBI patients is associated with a lower incidence of post CP hydrocephalus is based on significant heterogeneity (I2 = 85%). This considerable variation in results, in particular inconsistency in the direction of effect, makes it questionable to quote the intervention effect.[
Importantly, the included cohort study performed by Nasi et al. reported a hydrocephalus rate of 48% in the late CP group versus 5% when CP was performed early.[
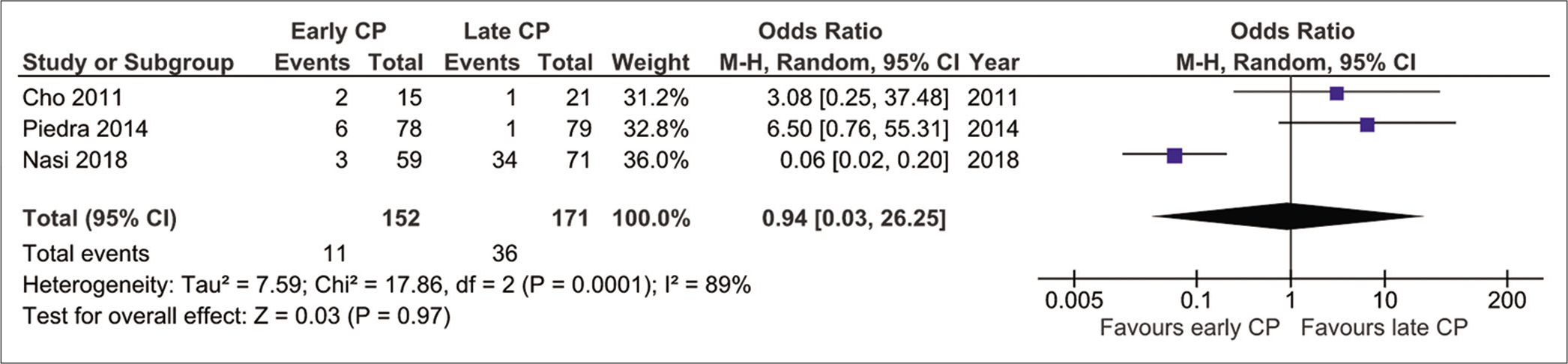
Figure 2:
Meta-analysis of hydrocephalus rate in patients undergoing early (within 3 months) versus late (after 3 months) cranioplasty after decompressive craniectomy for all pathologic conditions, with exclusion of outlying outcome result by Nasi et al.[
How to define post CP hydrocephalus?
The goal of the meta-analysis by Nasi and Dobran was to investigate the influence of timing of CP after decompressive craniectomy on post CP hydrocephalus. A fundamental issue, while reviewing studies reporting on the incidence of hydrocephalus following early and late CP, is the exact definition of post CP hydrocephalus. If a patient with pre CP hydrocephalus undergoes CP and subsequently requires implantation of a permanent CSF shunt, does one classify this as post CP hydrocephalus? In our recently published study on 145 patients undergoing CP, 26 suffered from pre CP hydrocephalus and received external CSF drainage. After CP, 13 of these patients required post CP ventriculoperitoneal (VP) shunt implantation (10/37 early CP patients and 3/108 late CP patients). Since these shunt placements were more or less “foreseen,” we did not classify them as post CP hydrocephalus. Instead, only post CP VP shunt implantations in patients without symptomatic disturbance in CSF flow prior to CP were classified as post CP hydrocephalus, which occurred in one patient of the early CP group.[
Figure 3:
Meta-analysis of hydrocephalus rate in patients undergoing early (within 3 months) versus late (after 3 months) cranioplasty (CP) after decompressive craniectomy for all pathologic conditions; (a) hydrocephalus rate reported as new seen after CP by Goedemans et al.[
CONCLUSION
Based on the abovementioned comments, revision of the conclusions drawn by Nasi and Dobran seems warranted as random effects meta-analysis shows that early CP in TBI patients is not associated with a lower incidence of hydrocephalus. To analyse the true association between the timing of CP and hydrocephalus as a complication seen after CP, the rate of pre CP hydrocephalus must be taken into account.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bender A, Heulin S, Röhrer S, Mehrkens JH, Heidecke V, Straube A. Early cranioplasty may improve outcome in neurological patients with decompressive craniectomy. Brain Inj. 2013. 27: 1073-9
2. Bjornson A, Tajsic T, Kolias AG, Wells A, Naushahi MJ, Anwar F. A case series of early and late cranioplasty-comparison of surgical outcomes. Acta Neurochir (Wien). 2019. 161: 467-72
3. Cho K, Park S. Safety and efficacy of early cranioplasty after decompressive craniectomy in traumatic brain injury patients. J Korean Neurotraumatol Soc. 2011. 7: 74-7
4. Goedemans T, Verbaan D, van der Veer O, Bot M, Post R, Hoogmoed J. Complications in cranioplasty after decompressive craniectomy: Timing of the intervention. J Neurol. 2020. 267: 1312-20
5. Higgins JPThomas JChandler JCumpston MLi TPage MJ. Cochrane Handbook for Systematic Reviews of Interventions. Available from: http://www.training.cochrane.org/handbook.
6. Hng D, Bhaskar MI, Khan FM, Budgeon C, Damodaran O, Knuckey N. Delayed cranioplasty: Outcomes using frozen autologous bone flaps. Craniomaxillofac Trauma Reconstr. 2015. 1: 190-7
7. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009. 6: e1000097-
8. Morton RP, Abecassis IJ, Hanson JF, Barber JK, Chen M, Kelly CM. Timing of cranioplasty: A 10.75-year single-center analysis of 754 patients. J Neurosurg. 2018. 128: 1648-52
9. Nasi D, Dobran M. Can early cranioplasty reduce the incidence of hydrocephalus after decompressive craniectomy? A meta-analysis. Surg Neurol Int. 2020. 11: 94-
10. Nasi D, Gladi M, Di Rienzo A, Di Somma L, Moriconi E, Iacoangeli M. Risk factors for post-traumatic hydrocephalus following decompressive craniectomy. Acta Neurochir (Wien). 2018. 160: 1691-8
11. Piedra MP, Ragel BT, Dogan A, Coppa ND, Delashaw JB. Timing of cranioplasty after decompressive craniectomy for ischemic or hemorrhagic stroke. J Neurosurg. 2013. 118: 109-14
12. Piedra MP, Ragel BT, Dogan A, Coppa ND, Delashaw JB. Timing of cranioplasty after decompressive craniectomy for trauma. Surg Neurol Int. 2014. 5: 25-
13. Quah BL, Low HL, Wilson MH, Bimpis A, Nga VD, Lwin S. Is there an optimal time for performing cranioplasties? Results from a prospective multinational study. World Neurosurg. 2016. 94: 13-7
14. .editors. Review Manager (RevMan) [Computer Program], Version 5.3. Copenhagen: The Nordic Cochrane Centre. London: The Cochrane Collaboration; 2014. p.
15. Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017. 358: j4008-
16. Walcott BP, Kwon CS, Sheth SA, Fehnel CR, Koffie RM, Asaad WF. Predictors of cranioplasty complications in stroke and trauma patients. J Neurosurg. 2013. 118: 757-62