- School of Medicine, New York Medical College, Valhalla, New York, United States.
- Department of Neurosurgery, University of New Mexico Hospital, Albuquerque, New Mexico, United States.
- Department of Emergency Medicine, New York Medical College, Valhalla, New York, United States.
Correspondence Address:
Christian A. Bowers
Department of Neurosurgery, University of New Mexico Hospital, Albuquerque, New Mexico, United States.
DOI:10.25259/SNI_46_2021
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ida Azizkhanian1, Ryan Alcantara1, Zachary Ballinger1, Edward Cho1, Silvi Dore1, Stergios Gatzofilas1, Raeesa Habiba Hossain1, Jesse Honig1, Nicole Matluck1, Jonathan V. Ogulnick1, Michael Rothbaum1, Iliya Rybkin1, Harrison Smith1, Brian Tung1, Syed Faraz Kazim2, Ivan Miller3, Meic H. Schmidt2, Chad D. Cole2, Christian A. Bowers2. Spine surgery complexity score predicts outcomes in 671 consecutive spine surgery patients. 03-May-2021;12:206
How to cite this URL: Ida Azizkhanian1, Ryan Alcantara1, Zachary Ballinger1, Edward Cho1, Silvi Dore1, Stergios Gatzofilas1, Raeesa Habiba Hossain1, Jesse Honig1, Nicole Matluck1, Jonathan V. Ogulnick1, Michael Rothbaum1, Iliya Rybkin1, Harrison Smith1, Brian Tung1, Syed Faraz Kazim2, Ivan Miller3, Meic H. Schmidt2, Chad D. Cole2, Christian A. Bowers2. Spine surgery complexity score predicts outcomes in 671 consecutive spine surgery patients. 03-May-2021;12:206. Available from: https://surgicalneurologyint.com/surgicalint-articles/10778/
Abstract
Background: The spine surgery complexity score (SSCS), previously reported by us, is a simple grading system to predict postoperative complications and hospital length of stay (LOS). This scale is based on the technical difficulty of the spinal procedures being performed.
Methods: We performed a retrospective chart review to validate SSCS in 671 consecutive patients undergoing spine procedures at a quaternary academic hospital.
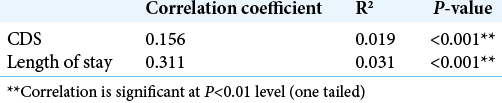
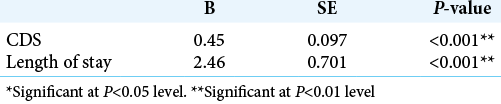
Results: The SSCS was predictive of the hospital LOS and postoperative complications (defined by the ClavienDindo score), based on linear regression analysis (P
Conclusion: Categorizing procedures according to the SSCS may enable neurosurgeons to assess surgical risk and predict longer LOS courses after spine surgery. Thus, it may prove useful in preoperative patient evaluation/ education and determining a prognosis based on surgical complexity.
Keywords: Hospital length of stay, Outcomes, Postoperative complications, Spine surgery, Surgical complexity scale
INTRODUCTION
Characterizing procedural complexity related to postsurgical outcomes can aid neurosurgeons in patient selection, preoperative counseling, and determining the prognosis.[
Here, we attempt to validate the spine surgery complexity score (SSCS), recently proposed by us,[
MATERIALS AND METHODS
Data collection
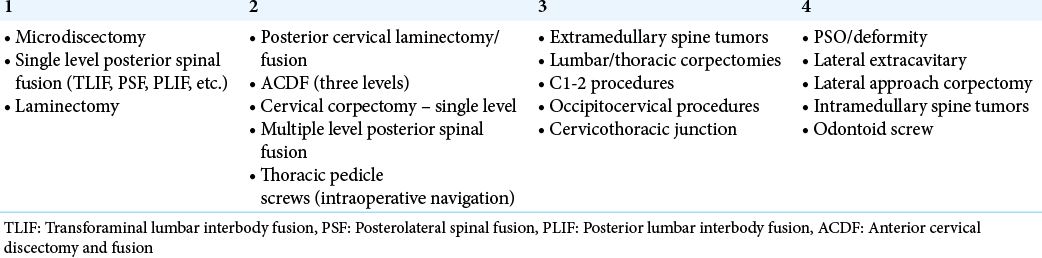
The patients undergoing spine surgery were identified from operating room logs of the Department of Neurosurgery, Westchester Medical Center, 2015–2017. A 4-level subjective complexity scale (SSCS) was devised based on what year of residency trainees typically learn each procedure [
Statistical analysis
Spearman’s correlation and univariate linear regression analysis were performed for comparing continuous variables and Likert scale scores. Significance was set at a cutoff of P < 0.05. All statistical analyses were performed using SPSS 24 software (IBM Corp., Armonk, NY).
RESULTS
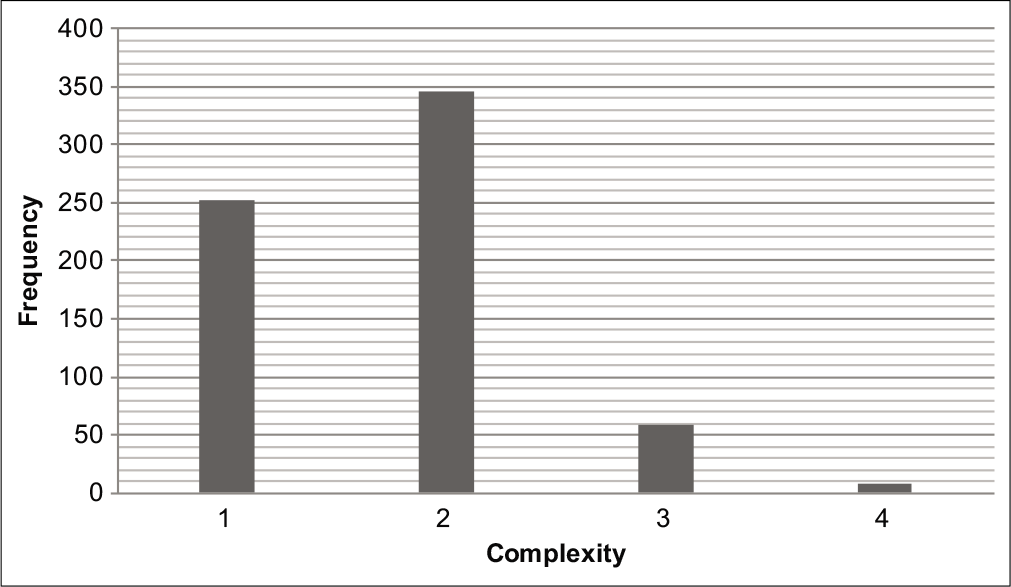
A total of 671 patients were included in this study with average age of 50 ± 17.15 years. Of these patients, 53.6% were men and 46.4% were women. The median SSCS was 2 (IQR:1); the average LOS was 7.14 ± 10.4 days; and the median CDS was 0 (IQR:2) [
DISCUSSION
Agreed-upon scales for both complexity and surgical outcomes are increasingly required for standardized evaluation of procedures, LOS, and outcomes in neurological surgery.[
Emphasizing postsurgical complications rather than patient functional impairment, the SSCS is also the only neurosurgical scale to use CDS as an endpoint, instead of, for example, change in Glasgow Coma Score (GCS). The most appropriate outcome measure may vary by subspecialty within neurosurgery. For example, a spine complexity scale that measures change in GCS may not yield important information about the difficulty of the preceding procedure. The most appropriate outcome measure may vary by subspecialty within neurosurgery. Current efforts by the N2QOD spine division are focused on preventing readmission after spine surgery and comparing effectiveness of different approaches to surgical treatment of spondylolisthesis using patient-reported outcome data. They also evaluate the endpoints of blood loss and LOS as reflections of surgical efficiency. Ultimately, future work should include evaluation of multiple endpoints to offer comprehensive analysis of surgical risk and operative complexity. Finally, as national patient databases become increasingly available, statistically derived complexity scales should be devised and compared to existing ones.
CONCLUSION
Stratifying procedures using the SSCS may enable neurosurgeons to assess surgical risk and predict hospital courses and outcomes for patients after spine surgery.
Declaration of patient consent
Institutional Review Board (IRB) permission obtained for the study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Asher AL, McCormick PC, Selden NR, Ghogawala Z, McGirt MJ. The national neurosurgery quality and outcomes database and neuropoint alliance: Rationale, development, and implementation. Neurosurg Focus. 2013. 34: E2
2. Asher AL, Speroff T, Dittus RS, Parker SL, Davies JM, Selden N. The national neurosurgery quality and outcomes database (N2QOD): A collaborative north American outcomes registry to advance value-based spine care. Spine (Phila Pa 1976). 2014. 39: S106-16
3. Azizkhanian I, Rothbaum M, Alcantara R, Ballinger Z, Cho E, Dore S. Demographics and outcomes of interhospital neurosurgical transfer patients undergoing spine surgery. World Neurosurg. 2020. 144: e221-6
4. Broggi M, Zattra C, Ferroli P. How to compare outcomes and complications in neurosurgery: We must make the mission possible!. Surg Neurol Int. 2018. 9: 65
5. Dindo D, Clavien PA. Quality assessment in surgery: Mission impossible?. Patient Saf Surg. 2010. 4: 18
6. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004. 240: 205-13
7. McGirt MJ, Speroff T, Dittus RS, Harrell FE, Asher AL. The national neurosurgery quality and outcomes database (N2QOD): General overview and pilot-year project description. Neurosurg Focus. 2013. 34: E6
8. Than KD, Curran JN, Resnick DK, Shaffrey CI, Ghogawala Z, Mummaneni PV. How to predict return to work after lumbar discectomy: Answers from the neuropoint-SD registry. J Neurosurg Spine. 2016. 25: 181-6
9. Whitmore RG, Curran JN, Ali ZS, Mummaneni PV, Shaffrey CI, Heary RF. Predictive value of 3-month lumbar discectomy outcomes in the neuropoint-SD registry. J Neurosurg Spine. 2015. 23: 459-66