- Department of Neurosurgery, University of Pittsburgh Medical Center, Pennsylvania, United States.
- Department of School of Medicine, University of Pittsburgh, Pittsburgh, Pennsylvania, United States.
Correspondence Address:
Enyinna Nwachuku
Department of Neurosurgery, University of Pittsburgh Medical Center, Pennsylvania, United States.
DOI:10.25259/SNI_562_2020
Copyright: © 2021 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Enyinna Nwachuku1, James Duehr2, Matthew W. Pease1, L. Dade Lunsford1, Edward A. Monaco1. Successful management of an intraluminal superior sagittal sinus meningioma causing elevated intracranial pressure using gamma knife radiosurgery in subacute setting: A case report. 08-Mar-2021;12:86
How to cite this URL: Enyinna Nwachuku1, James Duehr2, Matthew W. Pease1, L. Dade Lunsford1, Edward A. Monaco1. Successful management of an intraluminal superior sagittal sinus meningioma causing elevated intracranial pressure using gamma knife radiosurgery in subacute setting: A case report. 08-Mar-2021;12:86. Available from: https://surgicalneurologyint.com/surgicalint-articles/10637/
Abstract
Background: Gamma Knife stereotactic radiosurgery (GKRS) facilitates precisely focused radiation to an intracranial target while minimizing substantial off-target radiation in the surrounding normal tissue. Meningiomas attached to or invading the superior sagittal sinus may result in sinus occlusion and are often impossible to completely resect safely. The authors describe successful management of a patient with a meningioma located completely inside the posterior aspect of the superior sagittal sinus.
Case Description: A 46-year-old woman presented to the emergency department with progressive generalized headaches accompanied by worsening vision. The patient underwent a diagnostic brain magnetic resonance imaging which showed a solitary a 7 × 6 × 10 mm homogeneously contrast-enhancing lesion within the lumen of the posterior aspect of superior sagittal sinus without ventricular enlargement or peritumoral edema. The lesion was thought to be a meningioma radiographically. To evaluate the suspected increased intracranial pressure, a lumbar puncture was subsequently performed and demonstrated an opening pressure of 30 cm H2O. After drainage of 40 cc of CSF, the spinal closing pressure was 9 cm H2O. After failure of conservative management with acetazolamide, and determination of surgical inoperability due to the critical intraluminal location of the mass lesion, the patient underwent Gamma Knife radiosurgery. The 0.36 cc tumor was treated as an outpatient in the Perfexion® model Gamma Knife with a highly conformal and selective plan that enclosed the 3D geometry of the tumor with a minimal margin tumor dose of 14 gy at the 50% isodose. Three months after GKRS, the patient reported continued reduction in the frequency and severity of both her headaches and her visual disturbance. Ophthalmological consultation noted progressive resolution of her optic disc edema confirmed by formal optical coherence tomography. The patient is now 3 years out from GKRS with complete resolution of headache symptoms along with persistent reduction in tumor size (3 × 1 × 4 mm) on serial period imaging and resolution of papilledema.
Conclusion: Tumors located in such critical anatomic regions, as in our patient, should be considered for primary GKRS when the risks of biopsy or removal are too high. GKRS was able to provide great radiographic and clinical result in an intricately located meningioma.
Keywords: Gamma Knife radiosurgery, Image-guided neurosurgery, Lesion, Radiosurgery, Stereotactic surgery
INTRODUCTION
Gamma Knife stereotactic radiosurgery (GKRS) facilitates precisely focused radiation to an intracranial target while minimizing substantial off-target radiation in the surrounding normal tissue. GKRS is frequently used for meningiomas located in critical structures such as the cavernous sinus (of any Grades 1–3) to reduce risks associated with attempted resection.[
CASE REPORT
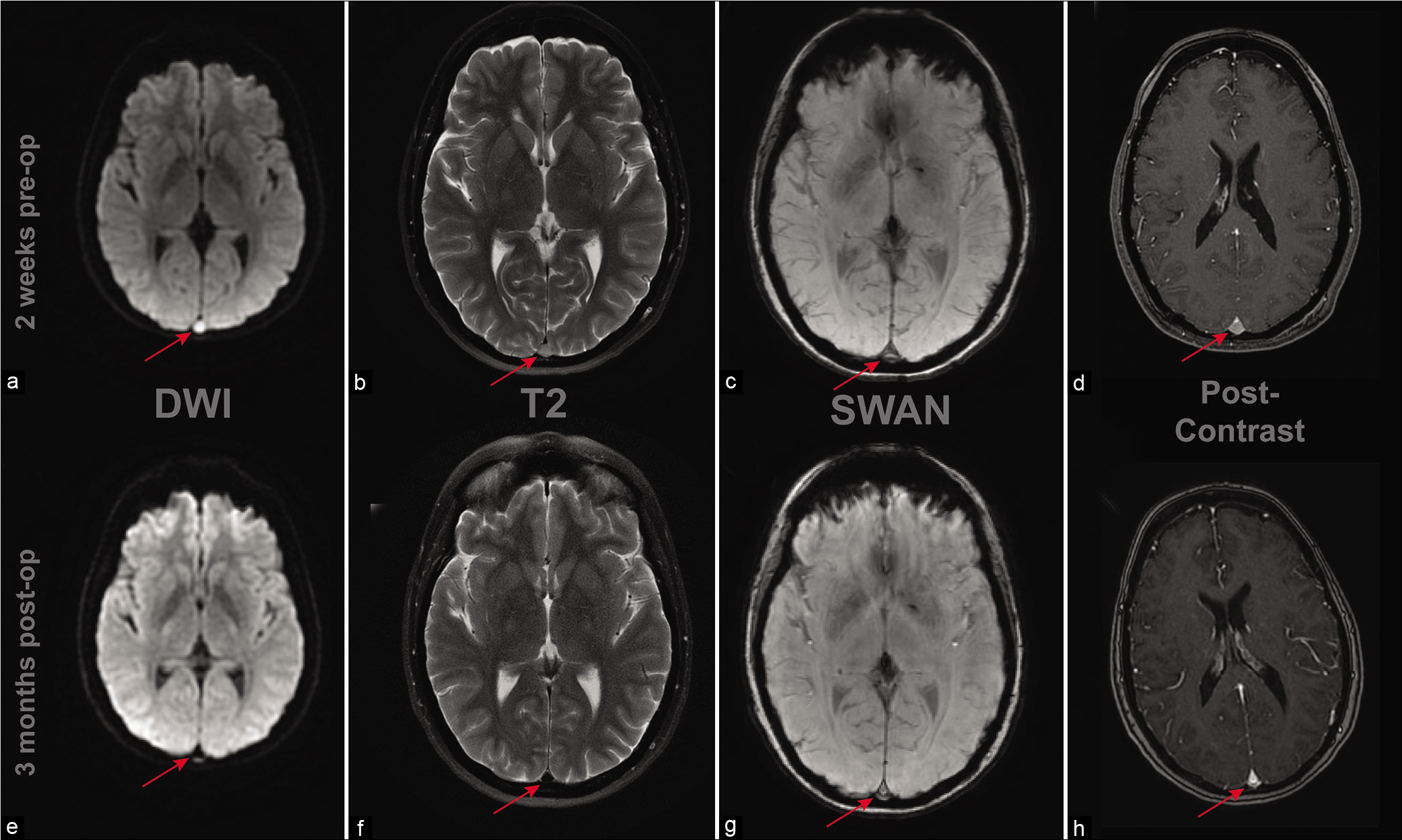
A 46-year-old woman with a history of sleep apnea, obesity, and osteoarthritis presented to the emergency department with progressive generalized headaches accompanied by worsening vision. One month previously, she noted a gradual increase in frequency of headache which she interpreted as related to underlying migraine events. The headaches were accompanied by increasing visual changes, notably zigzagging lines and a string in the middle of her visual field. After admission, the patient underwent a diagnostic brain magnetic resonance imaging (MRI) followed by MR angiogram and MR venogram. The diagnostic MRI showed a solitary 7 × 6 × 10 mm homogeneously contrast-enhancing lesion within the lumen of the posterior aspect of superior sagittal sinus not accompanied by ventricular enlargement or peritumoral edema [
Figure 1:
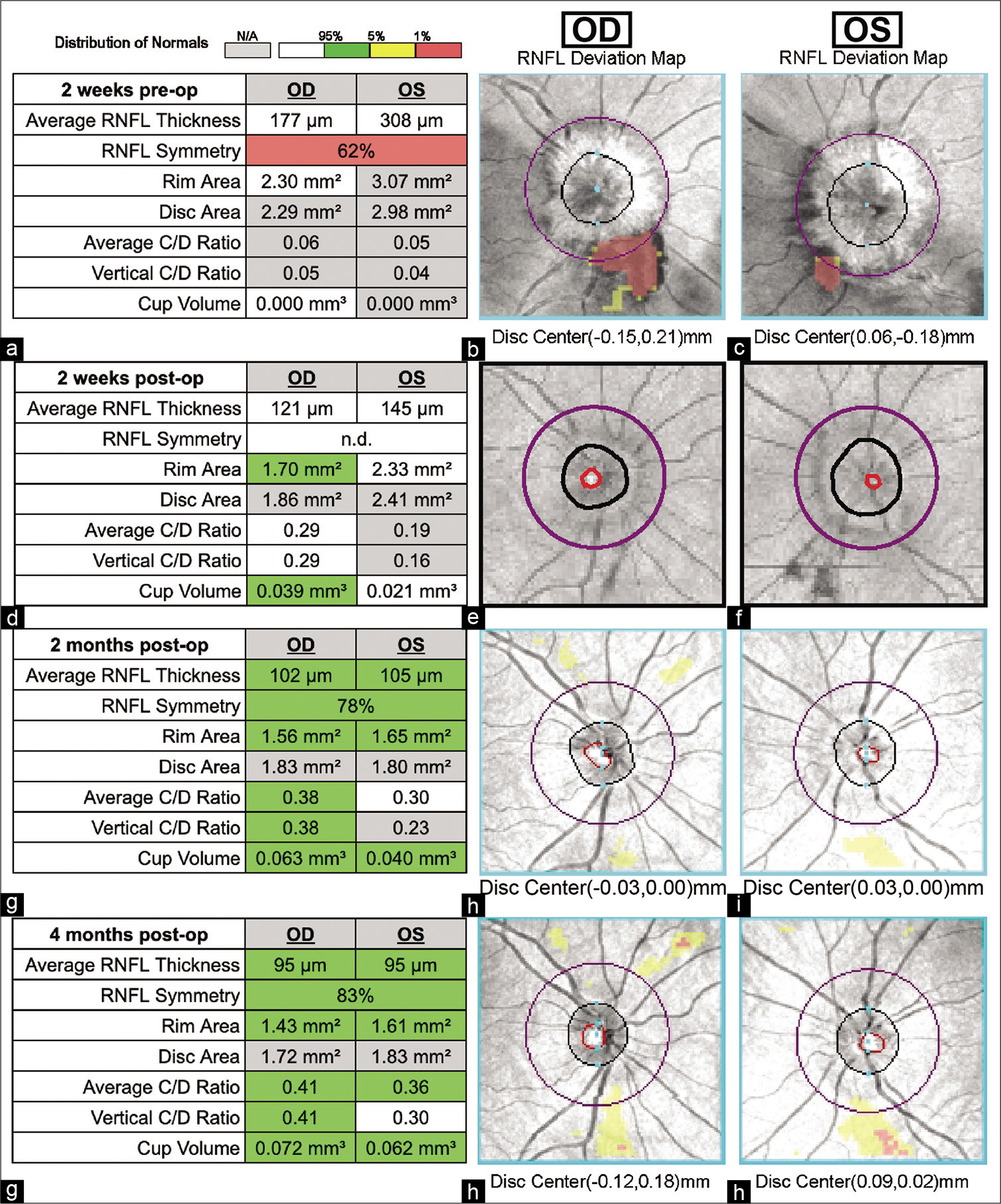
Optical coherence tomography (OCT) scans before and after GKRS treatment. OCT is a technique that permits noninvasive cross-sectional imaging of the retina. All images were obtained using a CIRRUS 5000 instrument with Zeiss OCT-HD software v9.0.0.281. (a-c) Two weeks before GKRS. (d-f) Two weeks post-GKRS. (g-i) Two months post-GKRS. (j-l) Four months post-GKRS. (a, d, g, and j) The summary data of the scan, including RNFL (Retinal Nerve Fiber Layer) thickness, RNFL symmetry (coefficient calculated by comparing OD and OS RNFL tomography), and C/D (cup to disc) ratios. (b, e, h, and k) The OD (right eye) RNFL deviation map, based on an en face fundus image with machine drawn boundaries of the cup (red), disc (black), and RNFL calculation circle (purple). (c, d, i, and l) The same for OS (left eye).
After initial stabilization in the emergency room, she was discharged after gentle intravenous hydration for her headache. Neurological evaluation failed to disclose any clinical signs. To evaluate the suspected increased intracranial pressure, a lumbar puncture was subsequently performed and demonstrated an opening pressure of 30 cm H2O. After drainage of 40 cc of CSF, the spinal closing pressure was 9 cm H2O. Ophthalmological examination demonstrated normal visual acuity and fields including a slip lamp examination. The clinical suspicion of papilledema was confirmed by optical coherence tomography (OCT) which showed bilateral optic edema [
Figure 2:
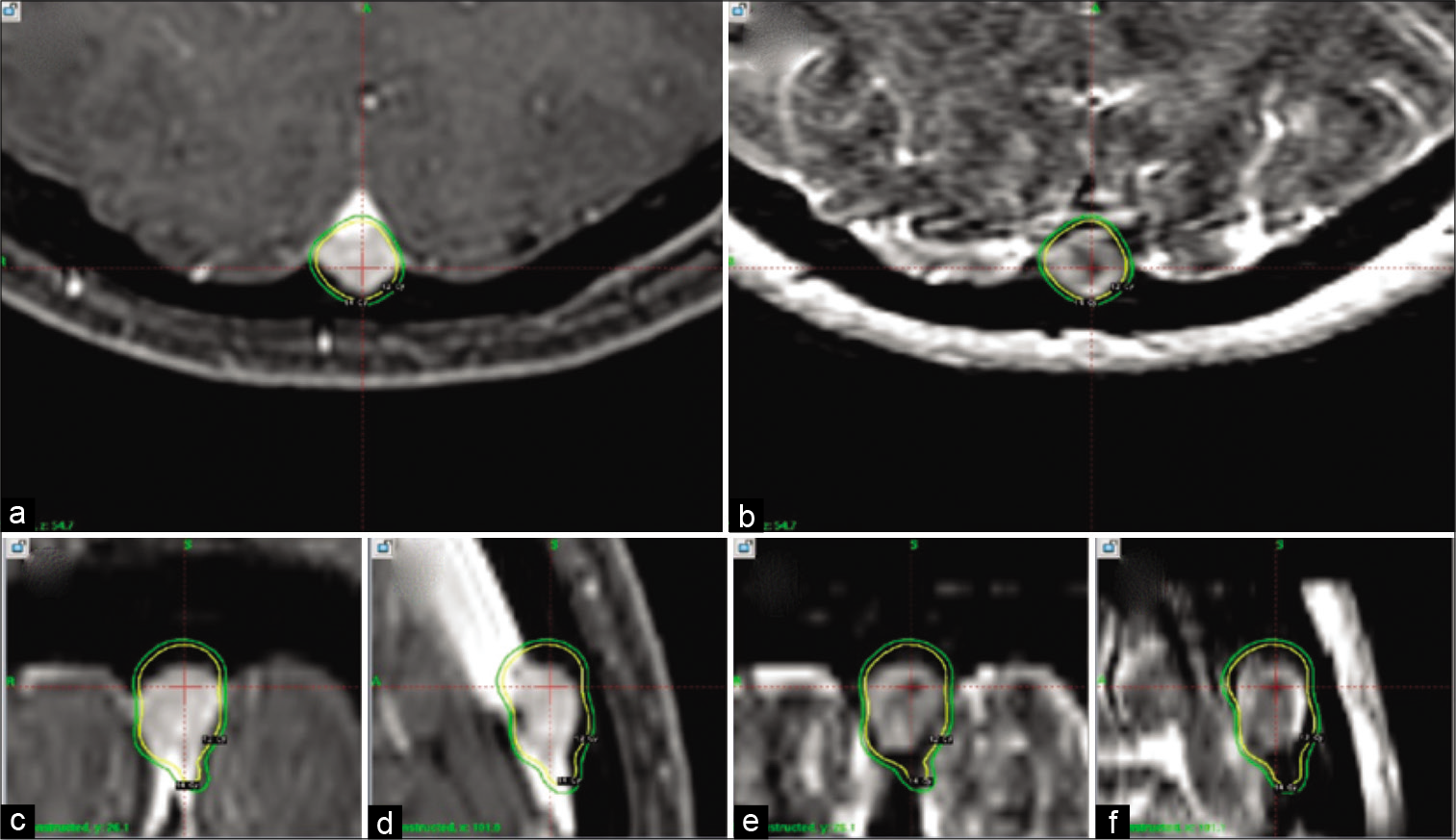
Gamma Knife radiosurgery dosage and localization plan. Treatment plan for GKRS irradiation using a Leksell Gamma Knife® Perfexion™ instrument. (a, c, and d) T1-weighted sequences with gadolinium contrast, while (b, e, and f) T2 weighted. Illustrated are the 12 gy (yellow) and 14 gy (green) isodose lines. Orientation as follows: (a and b) axial. (c and e) Coronal. (d and f) Sagittal.
Treatment
Using mild intravenous conscious sedation with midazolam and fentanyl supplemented by local anesthesia (0.5% bupivacaine and 0.5% lidocaine mixture, 40 cc total given with 10 cc at each pin site), a Leksell Model G (Elekta, Inc., Atlanta, GA) stereotactic head frame was attached to the cranial vault. Axial plane contrast enhanced 1.5 mm SPGR and 3 mm nonskipping T2-weighted whole-head MRI imaging were obtained. The 0.36 cc tumor was treated as an outpatient the Perfexion model Gamma Knife that used 3 isocenters of radiation employing the 4 and 8 mm diameter collimators to create a 14 Gy treatment volume at 50% isodose which enclosed 99% of the T1 contrast and T2 images with 3 mm cuts [
Figure 3:
Magnetic resonance imaging (MRI) sequences before and after Gamma Knife stereotactic radiosurgery treatment. (a-d) MRI with contrast obtained 2 weeks before treatment. (e-h) MRI with contrast obtained 3 months posttreatment. Specific sequences (DWI, T2 weighted, SWAN, and postcontrast) are as delineated in the figure. Red arrow shows progression at tumor regression with treatment with top figures showing pretreatment and figures at the bottom showing post-treatment.
RESULTS
Three months post-GKRS, the patient was reevaluated. She reported continued reduction in the frequency and severity of both her headaches and her visual disturbance over a 2-week time period following GKRS. Ophthalmological consultation noted progressive resolution of her optic disc edema confirmed by formal OCT tomography (OCT) 2 weeks after radiosurgery. The patient’s OCT showed significant improvement in the ensuing 4 months accompanied by improved retinal nerve fiber layer thickness [
DISCUSSION
Many critical advancements in imaging techniques, surgical approaches, and medical technology have greatly improved outcomes after resection of convexity meningiomas tumors located in the posterior aspect of the superior sagittal sinus often prove to be problematic because of the obstruction of normal venous outflow and resultant increased intracranial pressure.[
At our center, where more than 16,500 patients have undergone cranial radiosurgery during a 33-year interval, more than 2000 patients have had meningiomas. Both our outcome studies and many other published reports indicate that between 85–95% of meningiomas have progression-free survivals extending now for more than 30 years.[
The average accepted dosage around this location was 14 Gy, as was utilized in our patient.[
Given the completely intraluminal location of this lesion, the histology of this solitary tumor is unconfirmed but suspected by imaging to be a meningioma. Given that symptoms resolved with 14 Gy, the grade was likely low (1 or atypical, but not beyond). The risk of tumor biopsy or resection of a tumor in the posterior sagittal sinus was an impediment to histological confirmation. Hemangiopericytomas may mimic meningiomas using MRI and often respond more quickly and with greater volumetric reduction than do meningiomas,[
CONCLUSION
We believe that tumors located in such critical anatomic regions should be considered for primary GKRS when the risks of biopsy or removal are too high. The rapid improvement in patient symptoms and early tumor regression after radiosurgery were additionally gratifying outcomes in this patient. This case further illustrates that GKRS can be effectively implemented as a neurosurgical tool in the subacute management of symptomatic cavernous sinus meningiomas with partial intraluminal infiltration.
Statement of ethics
Formal informed consent was obtained from the patient involved in addition to all her information being deidentified for the purpose of publication.
Authors’ contributions
Enyinna L. Nwachuku, M.D.: Concept, data acquisition, manuscript preparation, and revision James E. Duehr, Ph.D.: Data acquisition and manuscript preparation Matthew W. Pease, M.D.: Manuscript preparation and revision L. Dade Lunsford, M.D.: Manuscript preparation and revision Edward A. Monaco, M.D., Ph.D.: Concept and manuscript preparation and revision.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Azar M, Kazemi F, Jahanbakhshi A, Chanideh I, Jalessi M, Amini E. Gamma knife radiosurgery for cavernous sinus meningiomas: Analysis of outcome in 166 patients. Stereotact Funct Neurosurg. 2017. 95: 259-67
2. Bonnal J, Brotchi J. Surgery of the superior sagittal sinus in parasagittal meningiomas. J Neurosurg. 1978. 48: 935-45
3. Conti A, Pontoriero A, Salamone I, Siragusa C, Midili F, La Torre D. Protecting venous structures during radiosurgery for parasagittal meningiomas. Neurosurg Focus. 2009. 27: E11
4. Davidson L, Fishback D, Russin JJ, Weiss MH, Yu C, Pagnini PG. Postoperative Gamma Knife surgery for benign meningiomas of the cranial base. Neurosurg Focus. 2007. 23: E6
5. DiMeco F, Li KW, Casali C, Ciceri E, Giombini S, Filippini G. Meningiomas invading the superior sagittal sinus: Surgical experience in 108 cases. Neurosurgery. 2008. 62: 1124-35
6. Hafez RF, Morgan MS, Fahmy OM. Stereotactic Gamma Knife surgery safety and efficacy in the management of symptomatic benign confined cavernous sinus meningioma. Acta Neurochir (Wien). 2015. 157: 1559-64
7. Harrison G, Kano H, Lunsford LD, Flickinger JC, Kondziolka D. Quantitative tumor volumetric responses after Gamma Knife radiosurgery for meningiomas. J Neurosurg. 2016. 124: 146-54
8. Kollova A, Liscak R, Novotny J, Vladyka V, Simonova G, Janouskova L. Gamma Knife surgery for benign meningioma. J Neurosurg. 2007. 107: 325
9. Kondziolka D, Flickinger JC, Perez B. Judicious resection and/ or radiosurgery for parasagittal meningiomas: Outcomes from a multicenter review. Gamma Knife Meningioma Study Group. Neurosurgery. 1998. 43: 405-13
10. Kondziolka D, Lunsford LD, McLaughlin MR, Flickinger JC. Long-term outcomes after radiosurgery for acoustic neuromas. N Engl J Med. 1998. 339: 1426-33
11. Lee JY, Niranjan A, McInerney J, Kondziolka D, Flickinger JC, Lunsford LD. Stereotactic radiosurgery providing long-term tumor control of cavernous sinus meningiomas. J Neurosurg. 2002. 97: 65-72
12. Lunsford LD. Contemporary management of meningiomas: radiation therapy as an adjuvant and radiosurgery as an alternative to surgical removal?. J Neurosurg. 1994. 80: 187-90
13. Oka K, Go Y, Kimura H, Tomonaga M. Obstruction of the superior sagittal sinus caused by parasagittal meningiomas: The role of collateral venous pathways. J Neurosurg. 1994. 81: 520-4
14. Olson C, Yen CP, Schlesinger D, Sheehan J. Radiosurgery for intracranial hemangiopericytomas: Outcomes after initial and repeat Gamma Knife surgery. J Neurosurg. 2010. 112: 133-9
15. Park KJ, Kano H, Iyer A, Liu X, Tonetti DA, Lehocky C. Gamma Knife stereotactic radiosurgery for cavernous sinus meningioma: long-term follow-up in 200 patients. J Neurosurg. 2018. 2018: 1-10
16. Raza SM, Gallia GL, Brem H, Weingart JD, Long DM, Olivi A. Perioperative and long-term outcomes from the management of parasagittal meningiomas invading the superior sagittal sinus. Neurosurgery. 2010. 67: 885-93
17. Roche PH, Regis J, Dufour H, Fournier HD, Delsanti C, Pellet W. Gamma knife radiosurgery in the management of cavernous sinus meningiomas. J Neurosurg. 2000. 93: 68-73
18. Zeiler FA, McDonald PJ, Kaufmann AM, Fewer D, Butler J, Schroeder G. Gamma Knife radiosurgery of cavernous sinus meningiomas: An institutional review. Can J Neurol Sci. 2012. 39: 757-62