- Department of Neurosurgery, Nara City Hospital, Nara, Japan
- Department of Neurosurgery, Nara Prefecture General Medical Center, Nara, Japan
Correspondence Address:
Takayuki Morimoto, Department of Neurosurgery, Nara City Hospital, Nara, Japan.
DOI:10.25259/SNI_736_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Takayuki Morimoto1, Kenta Fujimoto2, Sungchul Ko1, Toshikazu Nishioka1, Hidemori Tokunaga1. A case of spontaneous direct vertebral artery - External vertebral venous plexus fistula in the upper cervical portion. 27-Sep-2024;15:351
How to cite this URL: Takayuki Morimoto1, Kenta Fujimoto2, Sungchul Ko1, Toshikazu Nishioka1, Hidemori Tokunaga1. A case of spontaneous direct vertebral artery - External vertebral venous plexus fistula in the upper cervical portion. 27-Sep-2024;15:351. Available from: https://surgicalneurologyint.com/surgicalint-articles/13116/
Abstract
Background:Spontaneous direct vertebral artery-external vertebral venous plexus (VA-EVVP) fistula is a rare disease that presents in patients with neurofibromatosis type 1 (NF-1) or trauma.
Case Description:An 82-year-old female patient with no neurological deficits or trauma presented to our hospital with right hemianopsia. Head magnetic resonance imaging (MRI) revealed left occipital cerebral infarction and magnetic resonance angiography demonstrated high signal intensity in the left transverse sinus (TS). The attending doctor diagnosed an old infarction on the left occipital lobe and dural arteriovenous fistula (AVF) in the TS. After 3 years after the first diagnosis, her new attending doctor re-checked the MRI and performed digital subtraction angiography (DSA). The DSA examination revealed a single-hole AVF between the vertebral artery and external vertebral plexus at the C2 level, which was diagnosed as upper cervical VA-EVVP. The patient presented with tinnitus due to a high-flow VA-EVVP fistula, so we performed coil embolization of the fistula under general anesthesia using a double-catheter technique and achieved subtotal embolization, which diminished the intracranial reflux. The 6-month follow-up DSA image revealed complete obliteration of the AVF.
Conclusion:We report a rare case of upper cervical VA-EVVP fistula in a patient with no history of trauma and relevant medical conditions. Coil embolization of the fistula was performed using a combination of balloon-assisted and double-catheter techniques. Although the patient showed residual shunt flow after the intervention, follow-up DSA revealed complete obliteration. These findings should provide novel insights for the treatment strategy against VA-EVVP fistula.
Keywords: Arteriovenous fistula, Coil embolization, Spontaneous, direct vertebral artery-external vertebral venous plexus fistula
INTRODUCTION
Spontaneous direct vertebral artery-external vertebral venous plexus (VA-EVVP) fistula is a rare entity that presents as an arteriovenous fistula (AVF) between the vertebral artery (VA) and the adjacent venous plexus.[
CASE REPORT
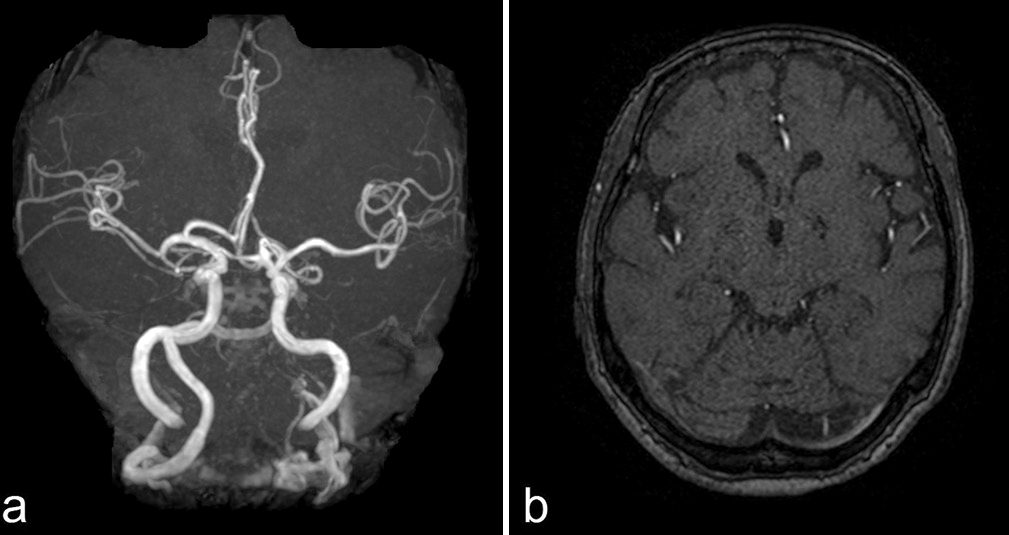
An 82-year-old female patient presented to our outpatient department with right-lower quadrantanopia and tinnitus. Her medical history included episodes of depression, hypertension, and no congenital disease. Head magnetic resonance imaging (MRI) revealed an old infarction in the left medial occipital lobe, and time of flight (TOF) imaging demonstrated high intensity in the left transverse sinus (TS) [
Figure 2:
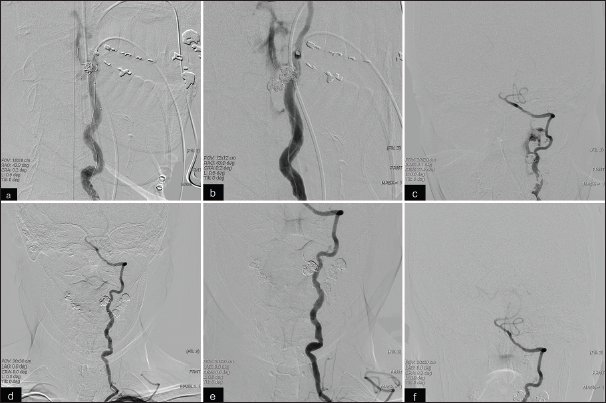
(a) Left vertebral artery (VA) angiography revealing vertebral artery- external vertebral venous plexus (VA-EVVP) fistula at the C2 level and venous drainage into the external VVP (EVVP), internal VVP (IVVP), internal jugular vein, and transverse sinus. (b, c, d) Three-dimensional rotational angiography and cone-beam computed tomography of the VA showing a single hole of a large fistula (arrow), EVVP (white arrowhead), and IVVP (red arrowhead).
Endovascular treatment was performed under general anesthesia. An 8-Fr OPTIMO catheter (Tokai Medical Products, Aichi, Japan) was guided into the left VA using a 6-Fr JB2 catheter and a 0.035-inch guiding wire. An intermediate catheter (NAVIEN; Medtronic, Minneapolis, MN, USA) was then advanced into the distal VA. A microcatheter (Excelsior SL-10; Stryker, Kalamazoo, MI, USA) was inserted into the lateral EVVP using a microwire (SynchroSELECT soft; Stryker). Another microcatheter (Phenom 17; Medtronic) was placed in the varix of the EVVP near the fistula using a microwire. A balloon catheter (Scepter XC: Terumo, Tokyo, Japan) was placed in the VA where the fistula was present [
Figure 3:
(a) Microcatheters were introduced into the EVVP (white arrowhead) and IVVP (red arrowhead). The arrow indicates the balloon catheter in the left VA. (b) Coil embolization by a combination of balloon-assisted and double-catheter techniques. (c) VA angiography after coil embolization. (d,e,f) VA angiography at three months after treatment showing complete occlusion of the fistula.
Head MRI on the following day showed no remarkable infarction and intracranial venous reflux, and the patient’s tinnitus disappeared. She was discharged on post-operative day 7. The 3-month follow-up DSA scan demonstrated complete occlusion of the VA-EVVP fistula with patency of the left VA [
DISCUSSION
VA-EVVP fistula is a rare disease caused by trauma, iatrogenic complications, or congenital disorders.[
VA-EVVP fistula is a rare disorder that presents with a single hole and a high-flow shunt between the VA and vertebral venous plexus (VVP).[
Due to the rare incidence of VA-EVVP fistula, its clinical course has not been established. While the appearance of symptoms such as numbness, neck pain, and gait disturbances can easily inform the decision to perform treatment for VA-EVVP fistula, treatment decisions for cases showing asymptomatic fistulas or fistulas with only bruit require more careful consideration. In comparison with other fistulas, the VA-EVVP fistula rarely shows spontaneous thrombosis.[
Various methods to treat VA-EVVP fistula, including surgery and endovascular treatment, have been reported to date. Endovascular treatment accounts for the majority of cases and surgery is limited to cases showing unsuccessful endovascular treatment.[
Preservation of VA patency in endovascular treatment of VA-EVVP fistula is also challenging, and some reports have recommended the use of assisted techniques to preserve VA patency.[
CONCLUSION
We report a rare case of spontaneous VA-EVVP fistula in a patient with no history of trauma, iatrogenic injuries, and congenital disease. DSA was performed due to the non-specific symptoms and the difficulty of diagnosis with only a head MRI. Coil embolization using a combination of balloon-assisted and double-catheter techniques finally resulted in complete obliteration of the fistula.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Bahar S, Chiras J, Carpena JP, Meder JF, Bories J. Spontaneous vertebro-vertebral arterio-venous fistula associated with fibro-muscular dysplasia. Report of two cases Neuroradiology. 1984. 26: 45-9
2. Briganti F, Tedeschi E, Leone G, Marseglia M, Cicala D, Giamundo M. Endovascular treatment of vertebrovertebral arteriovenous fistula. A report of three cases and literature review. Neuroradiol J. 2013. 26: 339-46
3. Chen C, Wu Y, Zhao K, Duan G, Liu J, Huang Q. Endovascular treatment of vertebro-vertebral arteriovenous fistula in neurofibromatosis type I: A report of two cases and literature review with a focus on endovascular treatment. Clin Neurol Neurosurg. 2021. 207: 106806
4. Deans WR, Bloch S, Leibrock L, Berman BM, Skultety FM. Arteriovenous fistula in patients with neurofibromatosis. Radiology. 1982. 144: 103-7
5. Gao P, Chen Y, Zhang H, Zhang P, Ling F. Vertebral arteriovenous fistulae (AVF) in neurofibromatosis type 1: A report of two cases. Turk Neurosurg. 2013. 23: 289-93
6. Geng J, Hu P, Ma Y, Zhang P, Zhang H. Endovascular treatment of V3 segment vertebro-vertebral arteriovenous fistula with Willis covered stent: Case report and literature review. Interv Neuroradiol. 2019. 25: 97-101
7. Gobin YP, Duckwiler GR, Viñuela F. Direct arteriovenous fistulas (carotid-cavernous and vertebral-venous). Diagnosis and intervention Neuroimaging Clin N Am. 1998. 8: 425-43
8. Halbach VV, Higashida RT, Hieshima GB. Treatment of vertebral arteriovenous fistulas. AJR Am J Roentgenol. 1988. 150: 405-12
9. Honarmand AR, Ansari SA, Alden TD, Soltanolkotabi M, Schoeneman SE, Hurley MC. Endovascular management of pediatric high-flow vertebro-vertebral fistula with reversed basilar artery flow. A case report and review of the literature. Interv Neuroradiol. 2013. 19: 215-21
10. Hori Y, Goto K, Ogata N, Uda K. Diagnosis and endovascular treatment of vertebral arteriovenous fistulas in neurofibromatosis type 1. Interv Neuroradiol. 2000. 6: 239-50
11. Iampreechakul P, Siriwimonmas S. Spontaneous obliteration of spontaneous vertebral arteriovenous fistula associated with fibromuscular dysplasia after partial surgery: A case report. Interv Neuroradiol. 2016. 22: 717-27
12. Lasjaunias P, Ter Brugge KG, Berenstein A, editors. Surgical neuroangiography. Berlin: Springer; 2006. p.
13. Narayana RV, Pati R, Dalai S. Endovascular management of spontaneous vertebrovertebral arteriovenous fistula associated with neurofibromatosis 1. Indian J Radiol Imaging. 2015. 25: 18-20
14. Paolini S, Colonnese C, Galasso V, Morace R, Tola S, Esposito V. Extradural arteriovenous fistulas involving the vertebral artery in neurofibromatosis Type 1: Case report. J Neurosurg Spine. 2008. 8: 181-5
15. Sher MH, Meyer NI, Lenhardt HF, Trummer MJ. Arteriovenous fistula involving the vertebral artery: Report of three cases. Ann Surg. 1966. 163: 408-13
16. Uneda A, Suzuki K, Okubo S, Hirashita K, Yunoki M, Yoshino K. Neurofibromatosis Type 1-associated extracranial vertebral artery aneurysm complicated by vertebral arteriovenous fistula after rupture: Case report and literature review. World Neurosurg. 2016. 96: 609.e13-8