- Department of Neurological Surgery, University of Pittsburgh Medical Center, Pittsburgh, PA, USA
Correspondence Address:
Robert M. Friedlander
Department of Neurological Surgery, University of Pittsburgh Medical Center, Pittsburgh, PA, USA
DOI:10.4103/2152-7806.183541
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Zwagerman NT, Pardini J, Mousavi SH, Friedlander RM. A refractory arachnoid cyst presenting with tremor, expressive dysphasia, and cognitive decline. Surg Neurol Int 03-Jun-2016;7:
How to cite this URL: Zwagerman NT, Pardini J, Mousavi SH, Friedlander RM. A refractory arachnoid cyst presenting with tremor, expressive dysphasia, and cognitive decline. Surg Neurol Int 03-Jun-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/a-refractory-arachnoid-cyst-presenting-with-tremor-expressive-dysphasia-and-cognitive-decline/
Abstract
Background:Arachnoid cysts are common incidental findings on intracranial imaging, although they are rarely symptomatic.
Case Description:We present a case of a 49 year-old woman with a recurrent left supraorbital arachnoid cyst who developed staring spells, expressive dysphasia, and tremor after cyst fenestration and cystoperitoneal shunting. Her symptoms resolved after removing the shunt valve and creating a valveless system. The case is discussed and the literature reviewed.
Conclusion:We present a case of a recurrent arachnoid cyst that developed worsening and new symptoms after cysto-peritoneal shunting with a programmable valve, which reducing the pressure in the cyst resulted in remarkable resolution of her symptoms.
Keywords: Arachnoid cyst, cystoperitoneal shunt, optic nerve, seizures, tremor, valve-less shunt
INTRODUCTION
The expansion of imaging capabilities has made the diagnosis of arachnoid cysts an increasingly common incidental finding on intracranial imaging. Previous studies on the topic have estimated the prevalence to be between 0.3% and 1.7% of the general population and highest in the pediatric subpopulation with a prevalence of 2.6%.[
CASE REPORT
A 49-year-old right-handed woman presented with left-sided headache, double vision, and left-sided facial numbness. She was found to have a multiloculated lesion appearing to originate from the region of the left orbital apex measuring 3 cm × 2.5 cm × 1.7 cm with signal intensity consistent with cerebrospinal fluid (CSF) likely representing an arachnoid cyst. The lesion displaced the optic chiasm to the right. The left optic nerve was also displaced along with the internal carotid artery and middle cerebral artery [
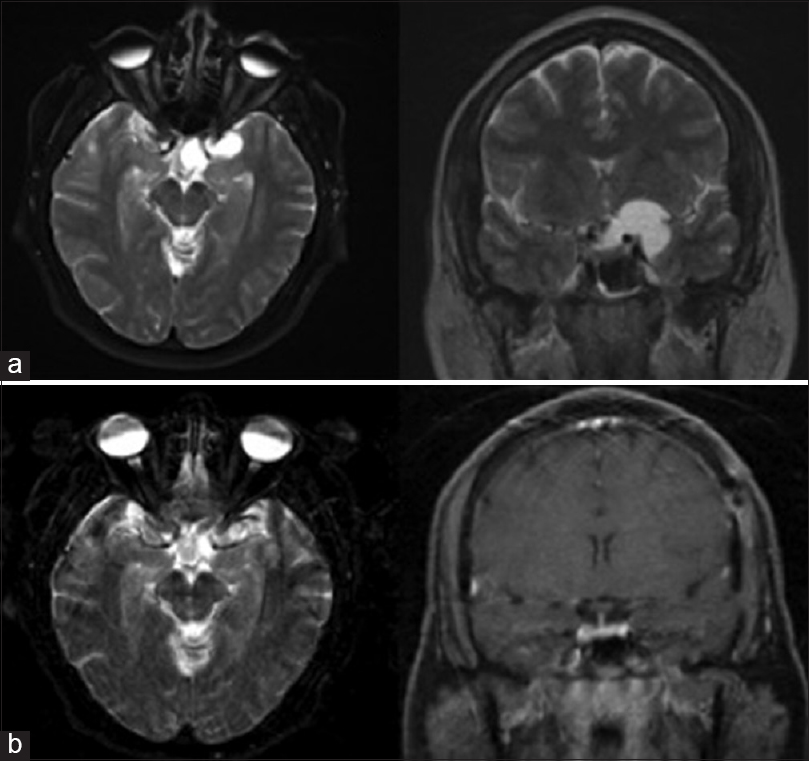
Figure 1
(a) T2 axial and coronal weighted magnetic resonance imaging depicting the preoperative arachnoid cyst located in the left supraorbital region compressing the left optic nerve, optic chiasm, internal carotid artery, and middle cerebral artery. (b) T2-weighted axial and T1 with contrast magnetic resonance imaging taken after left pterional craniotomy following fenestration of the cyst with near complete resolution of the cyst and patient symptoms
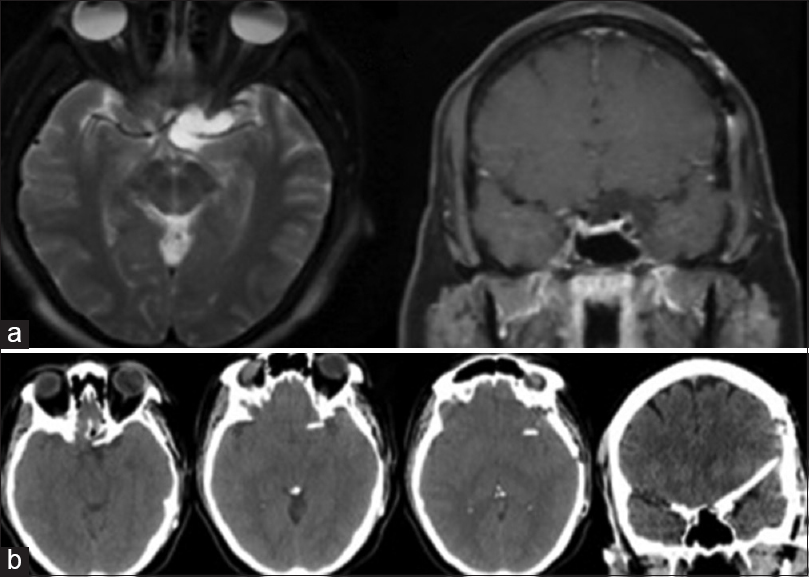
Figure 2
(a) T2-weighted axial and T1 with contrast coronal magnetic resonance imaging depicting a recurrent arachnoid cyst 3 years after surgical intervention for first cyst. (b) Sequential axial computed tomography images and coronal computed tomography image indicating the location of the cystoperitoneal shunt within the now obliterated cyst. Note: The catheter is not intraparenchymal but rather traveling on the skull base
DISCUSSION
Arachnoid cysts are a common incidental finding on intracranial imaging and in the vast majority of cases have a benign course and do not require treatment. A recent report by Al-Holou et al. indicated the imaging prevalence of 1.4% in adults.[
Surgical complications from treatment of arachnoid cysts include postoperative intracranial hematomas, CSF leak, infection, injury to vasculature, stroke, seizure, brain injury, nerve injury, pituitary dysfunction, or complications related to general anesthesia.[
Our patient had a symptomatic cyst that underwent fenestration with complete resolution of her symptoms for 3 years. After recurrence of her symptoms, imaging demonstrated recurrence of the cyst. For recurrent arachnoid cysts, the senior author placed a cystoperitoneal shunt using a programmable valve. Despite complete resolution of the cyst after surgery, the patient developed new symptoms including concerning EEG findings that were controlled with antiepileptic medications. Our patient suffered new cognitive decline, severe expressive aphasia, and tremors without any remarkable imaging finding to explain the new symptoms. The decision to remove the valve was made because the patient's pseudomeningocele was not improving despite the fact that the shunt was functional, and the valve was programmed to the minimum pressure setting. After removing the valve, the pseudomeningocele and (to our surprise) her severe expressive aphasia and tremors were completely resolved.
We speculate that the cause of the symptomatic decline following placement of the cyst to peritoneal shunt was surgical irritation of the temporal lobe combined with the residual pressure in the cyst. Although the purpose of eliminating the valve was to treat the pseudomeningocele, clearly reducing the cyst pressure resulted in a surprising and marked improvement of her severe expressive aphasia and tremors. Reduction of cyst pressure was enough for this patient to demonstrate a remarkable improvement. This case suggests that with symptomatic arachnoid cysts, symptoms may be related to subtle compression of adjacent neural structures, which may be relieved with the use of a valveless shunt system.
CONCLUSIONS
We present a case of a woman with a recurrent arachnoid cyst who, after cystoperitoneal shunting with a programmable valve, developed worsening and new symptoms, both on physical examination and neuropsychological testing. Reducing the pressure in the cyst resulted in remarkable resolution of her symptoms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Al-Holou WN, Terman S, Kilburg C, Garton HJ, Muraszko KM, Maher CO. Prevalence and natural history of arachnoid cysts in adults. J Neurosurg. 2013. 118: 222-31
2. Al-Holou WN, Yew AY, Boomsaad ZE, Garton HJ, Muraszko KM, Maher CO. Prevalence and natural history of arachnoid cysts in children. J Neurosurg Pediatr. 2010. 5: 578-85
3. Banna M. Arachnoid cysts on computed tomography. AJR Am J Roentgenol. 1976. 127: 979-82
4. Choi KY, Jung S, Kang SS, Kim IY, Jung TY, Jang WY. Technical considerations to prevent postoperative endocrine dysfunction after the fenestration of suprasellar arachnoid cyst. J Korean Neurosurg Soc. 2011. 49: 262-6
5. Ciricillo SF, Cogen PH, Harsh GR, Edwards MS. Intracranial arachnoid cysts in children. A comparison of the effects of fenestration and shunting. J Neurosurg. 1991. 74: 230-5
6. Duz B, Kaya S, Daneyemez M, Gonul E. Surgical management strategies of intracranial arachnoid cysts: A single institution experience of 75 cases. Turk Neurosurg. 2012. 22: 591-8
7. Eskandary H, Sabba M, Khajehpour F, Eskandari M. Incidental findings in brain computed tomography scans of 3000 head trauma patients. Surg Neurol. 2005. 63: 550-3
8. Gangemi M, Seneca V, Colella G, Cioffi V, Imperato A, Maiuri F. Endoscopy versus microsurgical cyst excision and shunting for treating intracranial arachnoid cysts. J Neurosurg Pediatr. 2011. 8: 158-64
9. Gündüz B, Yassa MI, Ofluoglu E, Ekinci B, Erdogan U, Asiltürk M. Two cases of arachnoid cyst complicated by spontaneous intracystic hemorrhage. Neurol India. 2010. 58: 312-5
10. Katzman GL, Dagher AP, Patronas NJ. Incidental findings on brain magnetic resonance imaging from 1000 asymptomatic volunteers. JAMA. 1999. 282: 36-9
11. Kim BS, Illes J, Kaplan RT, Reiss A, Atlas SW. Incidental findings on pediatric MR images of the brain. AJNR Am J Neuroradiol. 2002. 23: 1674-7
12. Levy ML, Wang M, Aryan HE, Yoo K, Meltzer H. Microsurgical keyhole approach for middle fossa arachnoid cyst fenestration. Neurosurgery. 2003. 53: 1138-44
13. Mottolese C, Szathmari A, Simon E, Ginguene C, Ricci-Franchi AC, Hermier M. The parallel use of endoscopic fenestration and a cystoperitoneal shunt with programmable valve to treat arachnoid cysts: Experience and hypothesis. J Neurosurg Pediatr. 2010. 5: 408-14
14. Rosell R, Monzó M, Pifarré A, Ariza A, Sánchez JJ, Moreno I. Molecular staging of non-small cell lung cancer according to K-ras genotypes. Clin Cancer Res. 1996. 2: 1083-6
15. Shim KW, Lee YH, Park EK, Park YS, Choi JU, Kim DS. Treatment option for arachnoid cysts. Childs Nerv Syst. 2009. 25: 1459-66
16. Vernooij MW, Ikram MA, Tanghe HL, Vincent AJ, Hofman A, Krestin GP. Incidental findings on brain MRI in the general population. N Engl J Med. 2007. 357: 1821-8
17. Weber F, Knopf H. Incidental findings in magnetic resonance imaging of the brains of healthy young men. J Neurol Sci. 2006. 240: 81-4