- Department of Neurosurgery, Doutou Neurosurgical Hospital, Kitami, Japan
- Department of Neurosurgery, Teikyo University School of Medicine, Tokyo, Japan
Correspondence Address:
Makoto Katsuno
Department of Neurosurgery, Teikyo University School of Medicine, Tokyo, Japan
DOI:10.4103/sni.sni_382_17
Copyright: © 2018 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Makoto Katsuno, Akira Matsuno. Aneurysm trapping by both direct and endovascular surgery for vertebral artery dissection: A case report. 16-Jan-2018;9:10
How to cite this URL: Makoto Katsuno, Akira Matsuno. Aneurysm trapping by both direct and endovascular surgery for vertebral artery dissection: A case report. 16-Jan-2018;9:10. Available from: http://surgicalneurologyint.com/surgicalint-articles/aneurysm-trapping-by-both-direct-and-endovascular-surgery-for-vertebral-artery-dissection-a-case-report/
Abstract
Background:Although vertebral artery (VA) dissecting aneurysms are treated by direct or endovascular surgery, some disadvantages are associated with each surgery. Therefore, the type of surgery should be selected based on the condition of the aneurysm. We performed aneurysm trapping by endovascular surgery via the contralateral VA after proximal direct ligation with bypass to prevent complications as well as achieve complete treatment.
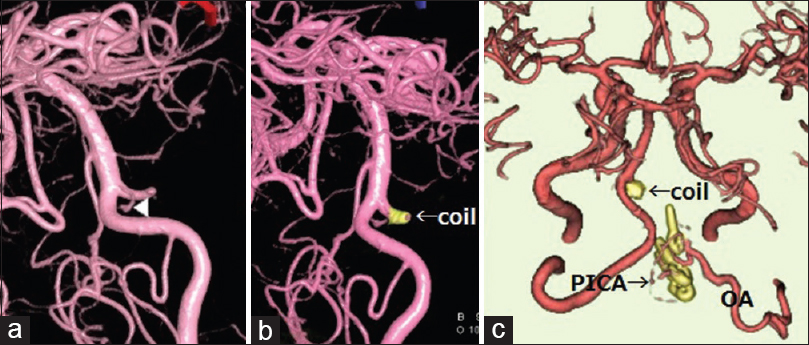
Case Description:We attempted to insert a distal clip to achieve complete trapping of the ruptured VA dissecting aneurysm after proximal ligation with occipital artery-posterior inferior cerebellar artery (PICA) anastomosis; however, the operative field was limited by the existence of lower cranial nerves, brain swelling, and tortuosity of VA. Therefore, we performed the aneurysmal trapping by endovascular surgery via contralateral VA just after the direct surgery.
Conclusions:This technique can provide complete resolution without any complications, particular in the case of bleeding VA dissecting aneurysms that have a PICA origin and are located in the high or contralateral position.
Keywords: Dissecting aneurysm, direct surgery, endovascular surgery, vertebral artery
INTRODUCTION
In recent years, the preferred surgery for vertebral artery (VA) dissecting aneurysm has been modified from a direct to an endovascular approach due to the development of endovascular instruments. However, endovascular surgery is not currently regarded to be sufficient or safe for cases that involve the posterior inferior cerebellar artery (PICA) or are associated with bleeding. Herein, we present a therapeutic technique using both direct and endovascular surgery.
CASE REPORT
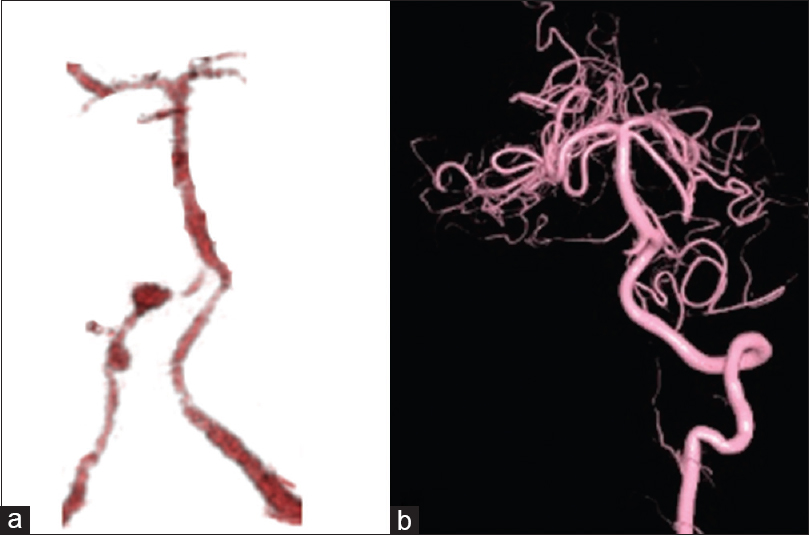
A 58-year-old man suddenly suffered from disturbance of consciousness. He was subsequently diagnosed with subarachnoid hemorrhage due to a ruptured right VA dissecting aneurysm [
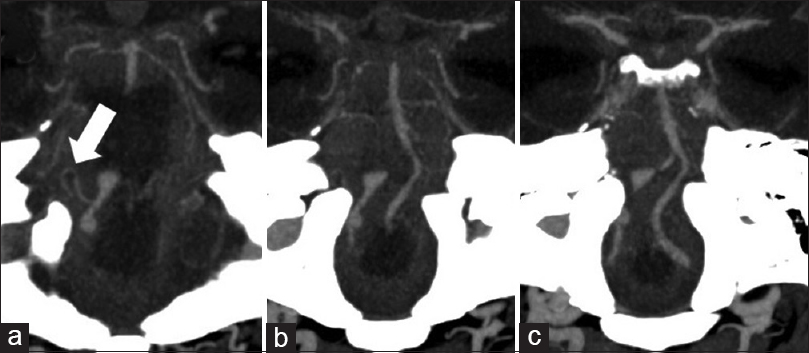
Figure 2
Enhancement computed tomography demonstrates a right vertebral artery dissection, which involves the posterior inferior cerebellar artery origin (arrow) (a). The level of the aneurysm extends from the jugular foramen (b) to above the internal acoustic canal (c); the distal edge of the dissection extends contralaterally because of the tortuosity of the right verterbral artery (c)
Figure 3
The distal section of the aneurysm and anterior spinal artery (arrowhead) observed at the contralateral vertebral artery (VA) during post direct surgery angiography (a). Retrograde placement of the coil performed at the proximal origin of the anterior spinal artery via the contralateral VA (b). The postoperative three-dimensional computed tomography demonstrates occipital artery to posterior inferior cerebellar artery bypass and the disappearance of the dissecting aneurysm via clip and coil (c). OA, occipital artery; PICA, posterior inferior cerebellar artery
DISCUSSION
Aneurysm trapping is considered to be the best treatment for VA dissecting aneurysm rather than proximal ligation, which prevents the worsening of the dissection.[
In conclusion, the aim of the treatment for bleeding VA dissecting aneurysm is complete trapping without any complications that cause occlusion of the PICA, perforators or the anterior spinal artery without damaging the lower cranial nerve. Although several combined surgeries for VA dissecting aneurysms have been reported,[
Disclosure
All authors certify that there is no conflict of interest (any financial or non-financial interest) in the subject matter or materials discussed in this manuscript.
Informed consent was obtained from all individual participants included in the study. Additional informed consent was obtained from all individual participants for whom identifying information is included in this article.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form tha patient(s) has /have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Endo H, Matsumoto Y, Kondo R, Sato K, Fujimura M, Inoue T. Medullary infarction as a poor prognostic factor after internal coil trapping of a ruptured vertebral artery dissection. J Neurosurg. 2013. 118: 131-9
2. Hamada J, Kai Y, Morioka M, Yano S, Todaka T, Ushio Y. Multimodal treatment of ruptured dissecting aneurysms of the vertebral artery during the acute stage. J Neurosurg. 2003. 99: 960-6
3. Iihara K, Sakai N, Murao K, Sakai H, Higashi T, Kogure S. Dissecting aneurysms of the vertebral artery: A management strategy. J Neurosurg. 2002. 97: 259-67
4. Masuo O, Terada T, Walker G, Tsuura M, Matsumoto H, Tohya K. Study of the patency of small arterial branches after stent placement with an experimental in vivo model. AJNR Am J Neuroradiol. 2002. 23: 706-10
5. Mizutani T, Aruga T. Rupture and outcome of vertebrobasilar dissecting aneurysms presenting subarachnoid hemorrhage. Surg Cereb Stroke. 1994. 22: 389-93
6. Rabinov JD, Hellinger FR, Morris PP, Ogilvy CS, Putman CM. Endovascular management of vertebrobasilar dissecting aneurysms. AJNR Am J Neuroradiol. 2003. 24: 1421-8
7. Starke RM, Ding D, Durst CR, Crowley RW, Liu KC. Combined microsurgical PICA-PICA bypass and endovascular parent artery occlusion for a ruptured dissecting vertebral artery aneurysm. Neurosurg Focus. 2015. 38:
8. Takai N, Ezuka I, Sorimachi T, Kumagai T, Sano K. Vertebral artery dissecting aneurysm rebleeding after proximal occlusion. Neurol Med Chir (Tokyo). 1993. 33: 165-8