- Clinical Neurological Sciences, London Health Sciences Centre, London, Ontario, Canada
- Medical Imaging, London Health Sciences Centre, London, Ontario, Canada
- Otolaryngology – Head and Neck Surgery, St. Joseph's Health Care, London, Ontario, Canada
Correspondence Address:
Neil Duggal
Clinical Neurological Sciences, London Health Sciences Centre, London, Ontario, Canada
DOI:10.4103/sni.sni_192_16
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Joel Bierer, Amparo Wolf, Donald H. Lee, Brian W. Rotenberg, Neil Duggal. Bilateral caudate nucleus infarcts: A case report of a rare complication following endoscopic resection of a tuberculum sellae meningioma. 26-Sep-2017;8:235
How to cite this URL: Joel Bierer, Amparo Wolf, Donald H. Lee, Brian W. Rotenberg, Neil Duggal. Bilateral caudate nucleus infarcts: A case report of a rare complication following endoscopic resection of a tuberculum sellae meningioma. 26-Sep-2017;8:235. Available from: http://surgicalneurologyint.com/surgicalint-articles/bilateral-caudate-nucleus-infarcts-a-case-report-of-a-rare-complication-following-endoscopic-resection-of-a-tuberculum-sellae-meningioma/
Abstract
Background:We present a rare complication of bilateral caudate infarcts and necrosed nasoseptal flaps after endoscopic transsphenoidal resection of tuberculum sellae meningioma. This case highlights the importance of early and accurate diagnosis and treatment of a postoperative cerebrospinal fluid (CSF) leak and associated bacterial meningitis, and reviews any existing guidelines regarding its management.
Case Description:A 54-year-old otherwise healthy man presented with progressive bitemporal hemianopsia. Magnetic resonance imaging of the head revealed a large, homogeneously enhancing sellar and suprasellar mass consistent with a meningioma. An endoscopic endonasal transsphenoidal approach was performed to resect the tuberculum sellae meningioma. The patient developed basal bacterial meningitis secondary to a CSF leak, requiring repair on two separate occasions. At the time of both repairs, there was evidence of necrosis of the nasoseptal flaps used for the repairs. Soon after the diagnosis of meningitis, the patient developed bilateral caudate infarcts.
Conclusion:This report discusses the possible underlying etiologies for the bilateral caudate infarcts and necrosed flaps including bacterial meningitis with associated local vasospasm of nearby vessels resulting in infarction. This case emphasizes the importance of concise management of postendoscopic CSF leak and discusses the guidelines regarding antimicrobial therapy and the management of lumbar drains.
Keywords: CSF leak, endoscopic transsphenoidal surgery, infarct, meningioma, meningitis
INTRODUCTION
The endoscopic endonasal transsphenoidal technique is routinely used to resect sellar and suprasellar lesions. Patient pain and discomfort can be reduced when undergoing endoscopic transsphenoidal resection compared to an open cranial procedure.[
CASE DESCRIPTION
A 54-year-old, right-handed gentleman presented with a 2-year history of progressive bitemporal hemianopsia, more severe on the left. Visual acuity was 20/25-2 in both eyes, with eccentric fixation. There was no relative afferent papillary defect. The remainder of the neurological examination was within normal limits. The patient was otherwise healthy, a nonsmoker, and on no medications. There was no history of vascular disease or vascular risk factors.
Imaging
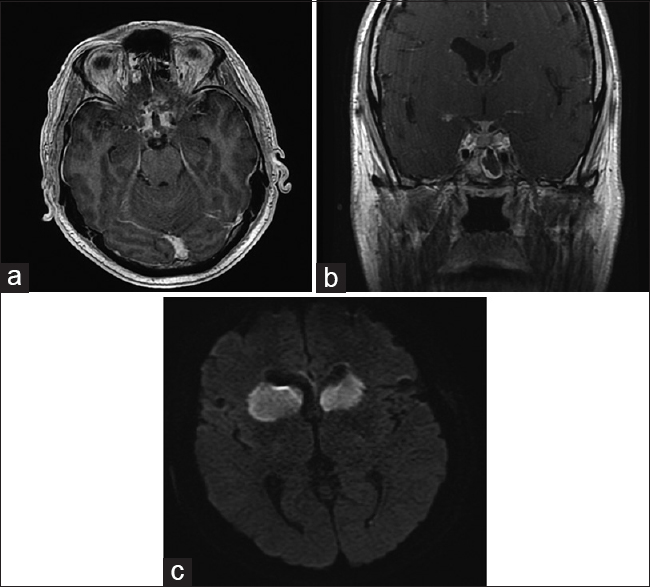
Magnetic resonance imaging (MRI) of the head revealed a well-defined enhancing mass in the sella turcica and suprasellar cistern measuring 2.6 × 2.7 cm, with an enhancing dural tail extending along the planum sphenoidale. The pituitary gland and infundibulum were displaced posteriorly. The optic chiasm was significantly displaced superiorly and draped over the superior aspect of the mass. Furthermore, the anterior communicating artery, bilateral A1 segments, and bilateral A2 segments were superiorly displaced. Imaging characteristics were most consistent with a tuberculum sella meningioma [
Figure 1
Radiographic appearance of a sellar and suprasellar meningioma in the current patient (a) Axial T1 MRI with gadolinium showing large homogeneously enhancing suprasellar mass. (b) Sagittal T1 MRI with gadolinium showing sellar/suprasellar mass with enhancing dural tail along planum sphenoidale. (c) Coronal T1 MRI with gadolinium showing superior displacement of optic chiasm
Surgical procedure
Endocrinological investigations did not reveal any signs of pituitary insufficiency. Taking into account the progressive visual changes, the patient elected to undergo endoscopic transsphenoidal resection. The patient was given 2 g cefazolin (Ancef) 30 minutes prior to the surgery. The surgical approach to sella was performed by an otolaryngologist in conjunction with a neurosurgeon. A posterior nasal septectomy was performed to allow binasal access. The face of the sphenoid and intersphenoidal septations were removed and an accessory approach through the superior 1/3 of the clivus was also created to maximize access and to facilitate mobilization of the pituitary gland during the case. The tumor was removed by a combination of suction and gentle traction. A gross total resection was achieved. The A1, A2, anterior communicating arteries, optic chiasm, and pituitary stalk were visualized and preserved during the surgery. Intraoperative CSF leak was repaired in a layered fashion consisting of gelfoam, fat, and fascia graft with a dura matrix overlay. A vascularized nasoseptal flap, fashioned at the beginning of the case, was positioned over the repair. Lastly, gelfoam soaked with tranexamic acid and fibrin glue (Tisseel) was laid down into the nasal cavity supported by an inflated Foley catheter. A lumbar drain was inserted postoperatively and discontinued 5 days later. Pathology confirmed the diagnosis of a grade I meningioma, meningothelial subtype.
Postoperative course
The patient's vision and endocrinological status remained stable. Approximately 10 days post surgery, the patient developed a CSF leak and a lumbar drain was reinserted. The patient was brought back to the operating room for repair of the CSF leak. The nasoseptal flap was found to be necrosed up to the proximal arterial supply with surrounding purulent material, which was sent for microbiology and pathology. The flap geometry had not been twisted or under undue tension to account for the necrosis. The repair site was taken down to the dura, which appeared infected from the nasal flap. A muscle graft from the left thigh was then transposed intracranially into the dural defect and dura matrix layered above, followed by a new vascularized inferior turbinate flap secured in place with gelfoam and fibrin glue (Tisseel). A Foley catheter maintained gentle pressure at the repair site and was deflated on postoperative day 1. Microbiological culture from the septal flap was positive for Haemophilus influenzae. Pathology confirmed necrotic tissue of the septal flap with prominent acute inflammation and bacterial aggregates. CSF sent from the lumbar drain had a glucose count of 2.7 mmol/L, protein 977 mg/L, and a nucleated cell count 708 × 106/L.
Within a day of the repair, the patient developed an abrupt severe headache and increasing confusion without obvious evidence of meningismus. MRI of the head revealed extensive leptomeningeal enhancement, surrounding the optic nerves and chiasm, into the Sylvian fissures and encasing the infundibulum [
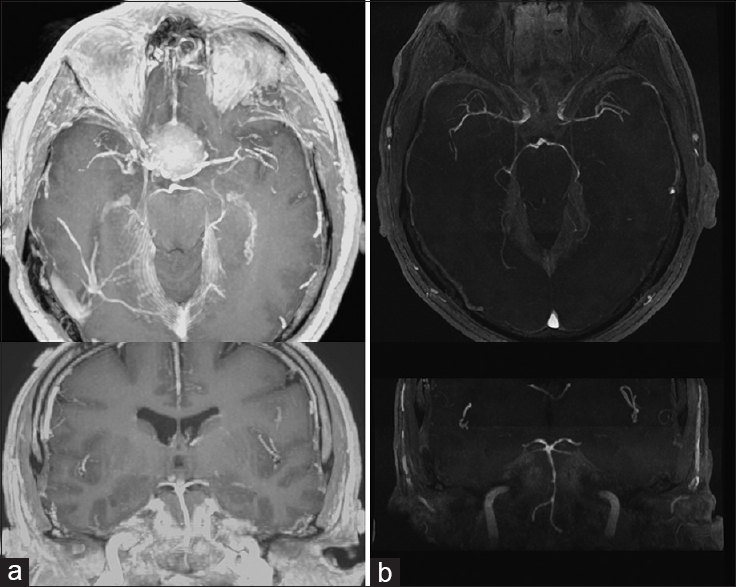
Figure 2
MRI head post resection of sellar/suprasellar meningioma. (a) Axial T1-weighted MRI with gadolinium showing extensive leptomeningeal enhancement around the base of the brain and postsurgical packing with no evidence of residual tumor, and (b) coronal T1-weighted MRI with gadolinium showing enhancement extending along the optic nerves and infundibulum. (c) T2-weighted trace, acquired from diffusion-weighted MRI, highlighting infarcts within the caudate head bilaterally, more extensively present on the right
The patient was diagnosed with bacterial meningitis and was treated with vancomycin and ceftriaxone to cover for H. influenzae and coagulase-negative Staphylococcus. The lumbar drain was discontinued on day 5. Six days after the first repair, the patient underwent a second CSF leak repair due to experiencing rhinorrhea when in a dependent position. Similar to the previous repair, the intranasal turbinate flap was completely necrosed; however, the rest of the repair remained virtually intact. Adjustment of the muscle graft stopped the leak. Tisseel and Gelfoam were again used to overlay the wound.
The patient was discharged home without any obvious neurological deficits related to the bilateral caudate infarcts. During interview with the family, the only changes noted were a subtle change in personality, impaired short-term memory, and the observation that the patient infrequently initiated speech. At the 6-month follow-up, the patient had no evidence of pituitary insufficiency and improved visual fields.
DISCUSSION
Bilateral caudate nucleus infarcts are relatively rare incidents. Behavioral abnormalities, movement disorders, language disturbances, and memory loss may occur, however, prognosis is favorable as 60% of patients fully recover.[
The intimate temporal relationship between this patient's bilateral caudate nucleus infarcts and diagnosis of basal meningitis points to the etiology of this vaso-occlusive event. MRI revealed basal cisternal infection with extensive leptomeningeal enhancement. There was visible local narrowing on MR angiogram of the A1 segments likely impacting on flow within the medial lenticulostriates as well as small cortical perforators, resulting in the infarcts. There was also narrowing of the M1 Sylvian segments and mild narrowing of the basilar artery; however, there was likely enough collateral blood supply distal to these to prevent any more extensive infarcts. In the context of cerebral inflammation or bacterial meningitis, many different factors influence cerebral blood flow including inflammatory hyperemia, mean cerebral blood flow velocity, increased intracranial pressure, arterial CO2, and mean arterial pressure among others. Cerebral inflammation in bacterial meningitis has been associated with reactive vasospasm of cerebral arteries and arterioles, effectively reducing the downstream blood flow.[
An initial review of this case focused on the use of the anti-fibrinolytic agent tranexamic acid during the meningioma resection operation. Tranexamic acid is used in patients with major life-threatening bleeding and has many off-label uses including dental procedures, perioperative bleeding control in cardiac and spinal surgery, epistaxis, blood conservation in hip or knee arthroplasties, caesarean sections, and transurethral prostatectomies.[
Necrosed vascularized nasal flaps have been reported in the literature, although it is not clear why tissue viability was lost in this case. Prior radiation to the nasopharynx or paranasal sinuses is a risk factor for flap necrosis, whereas septal spurs and iatrogenic injury can lead to intraoperative injury of the flap.[
In cases of intraoperative CSF leakage, meticulous reconstruction of the sellar floor is indicated to prevent postoperative fistula formation. The routine insertion of a lumbar drain in patients in whom an intraoperative CSF leakage has occurred has been shown in one study to significantly reduce the incidence of postoperative meningitis.[
In conclusion, this patient experienced two rare postoperative complications following a successful tuberculum sellae meningioma transsphenoidal endoscopic resection, namely bilateral caudate nucleus infarctions and recurrent necrosed nasoseptal flaps. The most likely etiology is acquired bacterial basal meningitis from a CSF leak, resulting in reactive vasospasm of local arteries. This case reinforces the importance of the early identification of a postoperative CSF leak and early identification and treatment of meningitis to avoid these potential complications.
Disclosure
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Caplan LR, Schmahmann JD, Kase CS, Feldmann E, Baquis G, Greenberg JP. Caudate infarcts. Arch Neurol. 1990. 47: 133-43
2. Dehdashti AR, Ganna A, Karabatsou K, Gentili F. Pure endoscopic endonasal approach for pituitary adenomas: Early surgical results in 200 patients and comparison with previous microsurgical series. Neurosurgery. 2008. 62: 1006-
3. Dunn CJ, Goa KL. Tranexamic acid: A review of its use in surgery and other indications. Drugs. 1999. 57: 1005-32
4. Eisenhut M. Vasospasm in cerebral inflammation. Int J Inflam 2014. 2014. p.
5. El-Sayed IH, Roediger FC, Goldberg AN, Parsa AT, McDermott MW. Endoscopic reconstruction of skull base defects with the nasal septal flap. Skull Base. 2008. 18: 385-94
6. Fassbender K, Ries S, Schminke U, Schneider S, Hennerici M. Inflammatory cytokines in CSF in bacterial meningitis: Association with altered blood flow velocities in basal cerebral arteries. J Neurol Neurosurg Psychiatry. 1996. 61: 57-61
7. Frank G, Pasquini E, Farneti G, Mazzatenta D, Sciarretta V, Grasso V. The endoscopic versus the traditional approach in pituitary surgery. Neuroendocrinology. 2006. 83: 240-8
8. Gondim JA, Almeida JP, Albuquerque LA, Schops M, Gomes E, Ferraz T. Endoscopic endonasal approach for pituitary adenoma: Surgical complications in 301 patients. Pituitary. 2011. 14: 174-83
9. Ivan ME, Bryan Iorgulescu J, El-Sayed I, McDermott MW, Parsa AT, Pletcher SD. Risk factors for postoperative cerebrospinal fluid leak and meningitis after expanded endoscopic endonasal surgery. J Clin Neurosci. 2015. 22: 48-54
10. Khan OH, Krischek B, Holliman D, Klironomos G, Kucharczyk W, Vescan A. Pure endoscopic expanded endonasal approach for olfactory groove and tuberculum sellae meningiomas. J Clin Neurosci. 2014. 21: 927-33
11. Lyons EL, Leeds NE. The angiographic demonstration of arterial vascular disease in purulent meningitis. Report of a case. Radiology. 1967. 88: 935-8
12. Morrison JJ, Dubose JJ, Rasmussen TE, Midwinter MJ. Military Application of Tranexamic Acid in Trauma Emergency Resuscitation (MATTERs) Study. Arch Surg. 2012. 147: 113-9
13. Pellizzaro Venti M, Paciaroni M, Caso V. Caudate infarcts and hemorrhages. Front Neurol Neurosci. 2012. 30: 137-40
14. Roberts I, Prieto-Merino D, Manno D. Mechanism of action of tranexamic acid in bleeding trauma patients: An exploratory analysis of data from the CRASH-2 trial. Crit Care. 2014. 18: 685-
15. Rotenberg B, Tam S, Ryu WH, Duggal N. Microscopic versus endoscopic pituitary surgery: A systematic review. Laryngoscope. 2010. 120: 1292-7
16. van Aken MO, Feelders RA, de Marie S, van de Berge JH, Dallenga AH, Delwel EJ. Cerebrospinal fluid leakage during transsphenoidal surgery: Postoperative external lumbar drainage reduces the risk for meningitis. Pituitary. 2004. 7: 89-93
17. Yutthakasemsunt S, Kittiwatanagul W, Piyavechvirat P, Thinkamrop B, Phuenpathom N, Lumbiganon P. Tranexamic acid for patients with traumatic brain injury: A randomized, double-blinded, placebo-controlled trial. BMC Emerg Med. 2013. 13: 20-
18. Zhang F, Wang K, Li FN, Huang X, Li Q, Chen Z. Effectiveness of tranexamic acid in reducing blood loss in spinal surgery: A meta-analysis. BMC Musculoskelet Disord. 2014. 15: 448-
19. Zhang Y, Fu X, Liu WX, Li YM, Ma XL, Li ZJ. Safety and efficacy of intra-articular injection of tranexamic acid in total knee arthroplasty. Orthopedics. 2014. 37: e775-82