- Department of Neurosurgery, Papageorgiou Hospital, Thessaloniki, Greece,
- Department of Neurology, University Hospital of Alexandroupolis, Alexandroupolis, Greece,
- Department of Neurosurgery, University Hospital of Larissa, Larissa, Greece,
- Department of Neurosurgery, Cayuga Medical Center, Ithaca, New York, USA.
Correspondence Address:
Ioannis D. Siasios
Department of Neurosurgery, Cayuga Medical Center, Ithaca, New York, USA.
DOI:10.25259/SNI_436_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ioannis D. Siasios, Aggeliki Fotiadou, Kostas Fountas, Vassilios Dimopoulos. Holospinal epidural abscess in elderly patient: A case presentation and review. 18-Oct-2019;10:204
How to cite this URL: Ioannis D. Siasios, Aggeliki Fotiadou, Kostas Fountas, Vassilios Dimopoulos. Holospinal epidural abscess in elderly patient: A case presentation and review. 18-Oct-2019;10:204. Available from: http://surgicalneurologyint.com/surgicalint-articles/9713/
Abstract
Background: Holospinal epidural abscess (HEA) is a rare pathological entity with significant morbidity and mortality rates. Here, we present a 74-year-old male with HEA treated with focal skip laminectomies and catheter irrigation.
Case Description: A 74-year-old male presented with fever, neck/back pain, and slight weakness in his legs bilaterally (4/5). The patient underwent a magnetic resonance imaging (MRI) of the entire spine showing an epidural collection extending from C5-C6 to the L4-L5 levels. Laboratory studies revealed a leukocytosis and an elevated C-reaction protein level. Blood cultures were positive for methicillin-sensitive Staphylococcus aureus. The patient underwent skip laminectomies at C6 and C7; T2, T3, T5, T6, T8, T9, T10, and T12; and L3, L4, and L5 with catheter irrigation between these levels; this minimized the risk of postoperative kyphosis and instability. His postoperative course was uneventful. Other surgical approaches to HEA described in literature include laminectomy, focal laminectomies, and skip laminectomies.
Conclusion: In this case of a holospinal HEA, skip laminectomies and catheter irrigation avoided neurological deterioration and delayed spinal instability in a 74-year-old male.
Keywords: Abscess, Epidural, Holospinal, Laminectomy, Surgery
INTRODUCTION
Epidural abscess (EDA) is a life-threatening condition that can rapidly lead to permanent neurological deficits and even death due to sepsis if the diagnosis and treatment are delayed.[
The clinical triad for EDA includes fever, back pain, and neurologic decline; however, in some patients, symptoms and signs may be nonspecific (e.g., malaise and fever).[
CASE DESCRIPTION
A 74-year-old male complained of neck and back pain for 10 days duration. He had previously been diagnosed with lumbar spinal stenosis (L3/4 and L4/5) and had recently been placed on methylprednisolone. In the emergency department, he was febrile to 37.7°C, and he exhibited intermittent confusion, mild weakness in both lower extremities (4/5), and diminished deep tendon reflexes bilaterally. Laboratory studies showed a marked leukocytosis (33,000/mm3) with 92% neutrophils and a markedly elevated C-reaction protein (CRP) (166 mg/L) level.
Diagnostic MR and laboratory studies
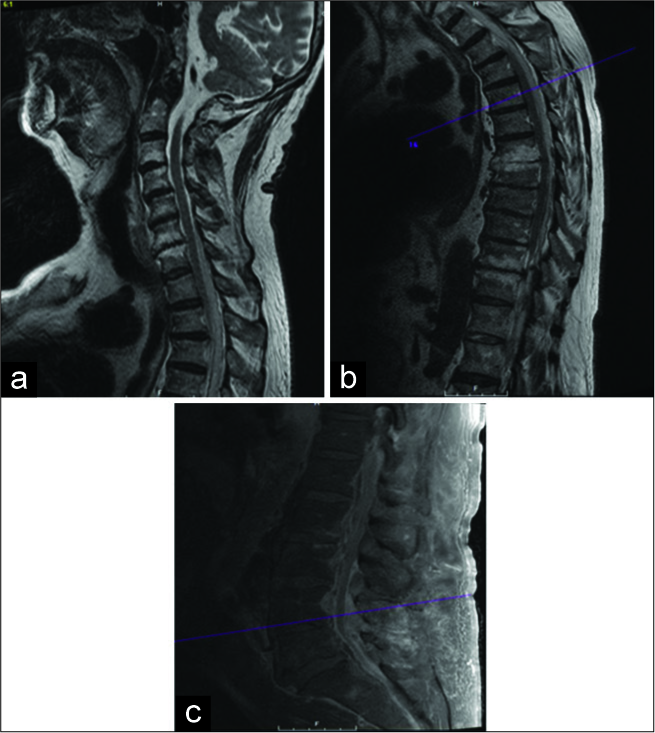
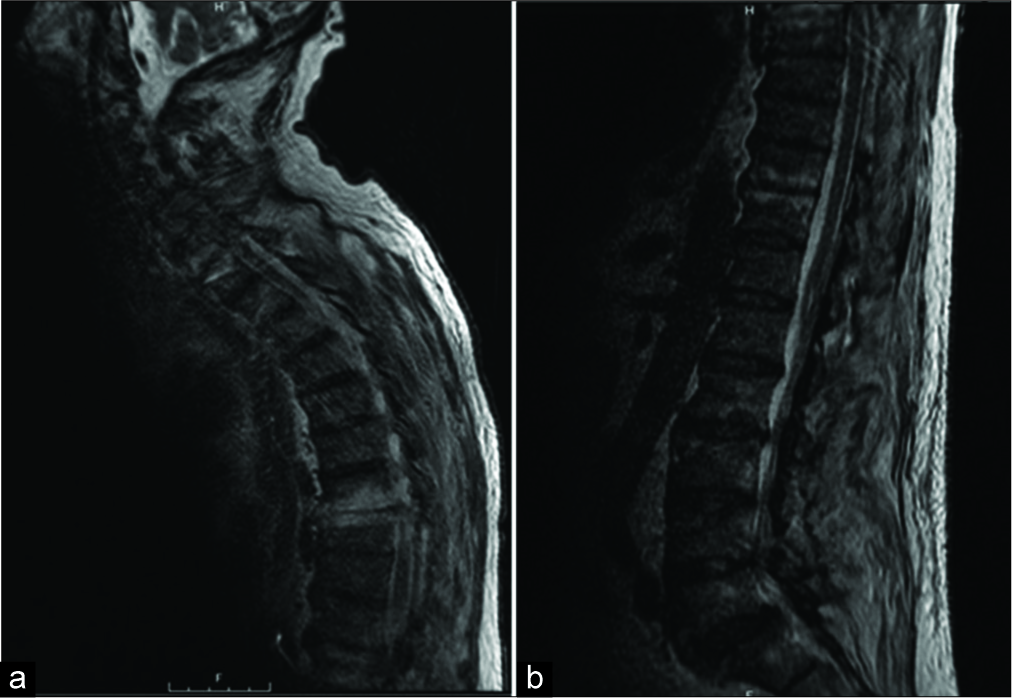
The patient underwent an MRI of the entire spine with and without contrast; it showed an epidural collection consistent with an epidural abscess extending from C5/C6 all the way to L4/L5 level, accompanied by maximal cord compression at C6 and T4 [
Lumbar surgery
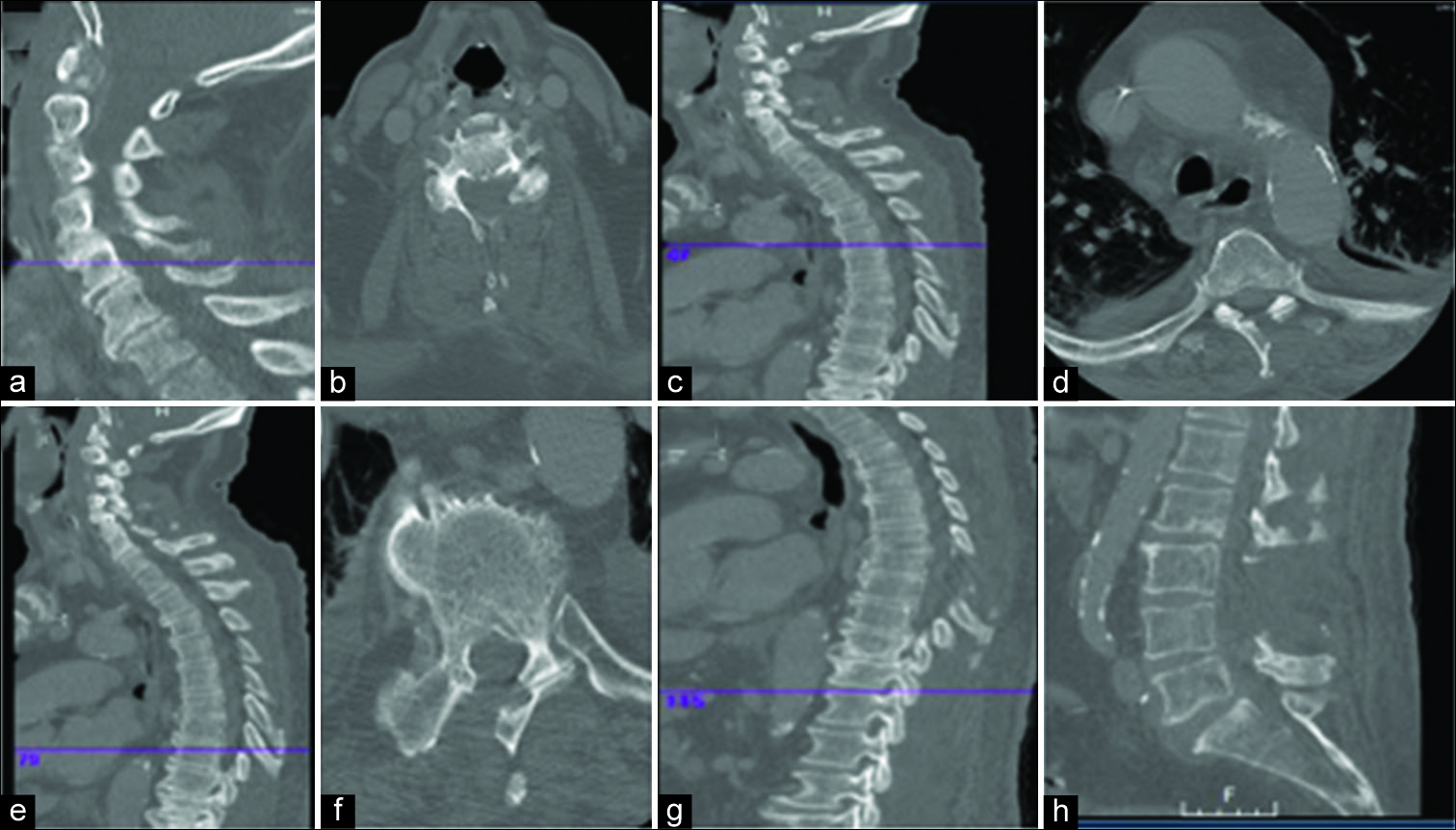
With the diagnosis of a holospinal spinal EDA, the patient underwent multiple skip laminectomies (e.g., at the C6, C7, T2, T3, T5, T6, T8, T9, T10, and T12 levels); complete laminectomies were performed at L3, L4, and L5 [
DISCUSSION
Diagnosis of HEA
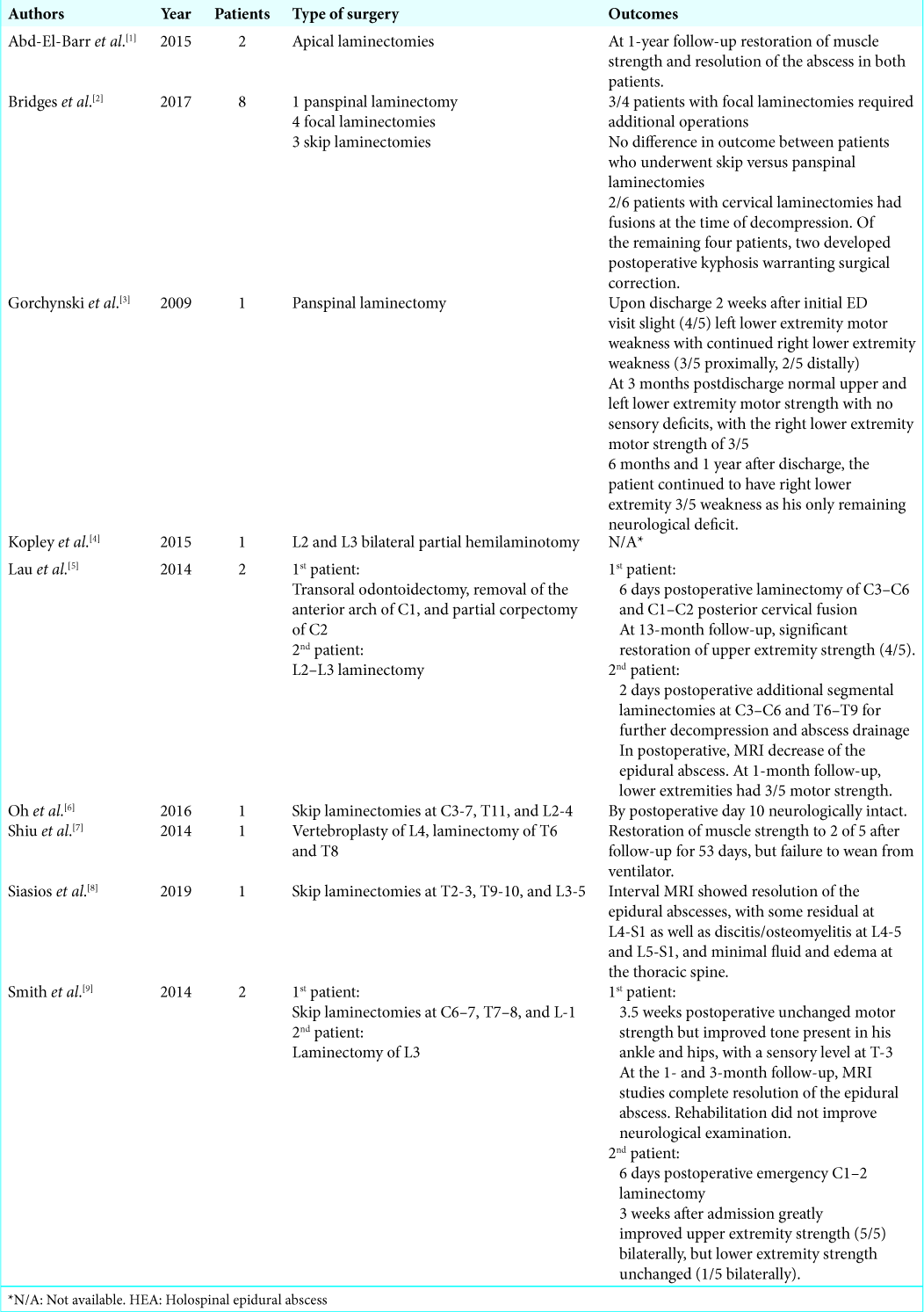
In literature, there are few reports of HEAs [
Surgery of HEA
Surgical management of HEAs is critical to avoid neurological deterioration.[
Surgical approaches
Multiple surgical alternatives for treating HEAs include (1) multilevel laminectomy (e.g., of the entire vertebral column), (2) focal laminectomies (e.g., at levels of maximal cord compromise), and (3) skip laminectomies using epidural irrigation/aspiration (e.g., fewer laminectomies/reduced instability).[
Skip laminectomies
A modification of skip laminectomies for liquid pus evacuation was described by Abd-El-Barr et al.; this involved three separate midline incisions at the midcervical, midthoracic, and midlumbar levels.[
CONCLUSION
Complete evacuation of dorsally located and liquefied HEAs is feasible even in elderly patients with significant comorbidities utilizing skip laminectomies and intervening catheter irrigation for aspiration of epidural pus. Such skip procedures significantly reduce the risk of postoperative kyphosis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abd-El-Barr MM, Bi WL, Bahluyen B, Rodriguez ST, Groff MW, Chi JH. Extensive spinal epidural abscess treated with “apical laminectomies” and irrigation of the epidural space: Report of 2 cases. J Neurosurg Spine. 2015. 22: 318-23
2. Bridges KJ, Than KD. Holospinal epidural abscesses institutional experience. J Clin Neurosci. 2018. 48: 18-27
3. Gorchynski J, Hwang J, McLaughlin T. A methicillin-resistant Staphylococcus aureuspositive holospinal epidural abscess. Am J Emerg Med. 2009. 27: 514-9
4. Koplay M, Sivri M, Emiroglu MK, Guler İ, Karabagli H, Paksoy Y. Holospinal epidural abscess in a child patient: Magnetic resonance imaging findings. Spine J. 2015. 15: e1-2
5. Lau D, Maa J, Mummaneni PV, Chou D. Holospinal epidural abscess. J Clin Neurosci. 2014. 21: 517-20
6. Oh GS, Abou-Al-Shaar H, Arnone GD, Barks AL, Hage ZA, Neckrysh S. Spinal epidural abscess in a patient with piriformis pyomyositis. Surg Neurol Int. 2016. 7: S911-13
7. Shiu SI, Lee BJ, Chen HC, Lin YH, Wang CY. Holospinal epidural abscess complicated with bilateral psoas muscle abscess. Spine J. 2014. 14: 1072-3
8. Siasios ID, Szewczyk B, Zakeri A, Kowalski JM, Dimopoulos VG. Holospinal epidural abscess combined with multifocal extraspinal abscesses in rheumatoid arthritis. J Neurosurg Sci. 2019. 63: 348-50
9. Smith GA, Kochar AS, Manjila S, Onwuzulike K, Geertman RT, Anderson JS. Holospinal epidural abscess of the spinal axis: Two illustrative cases with review of treatment strategies and surgical techniques. Neurosurg Focus. 2014. 37: E11-