- Department of Clinical Neuroscience, Division of Neurological Surgery, Spectrum Health, Michigan State University, Departments of Neurosurgery,
- College of Medicine, Central Michigan University, Mt. Pleasant,
- Ascension St. Mary’s Hospital Neurosurgery Associates, Saginaw,
- Field Neuroscience Institute, Saginaw, Michigan, USA.
Correspondence Address:
Theresa A. Elder
College of Medicine, Central Michigan University, Mt. Pleasant,
Ascension St. Mary’s Hospital Neurosurgery Associates, Saginaw,
Field Neuroscience Institute, Saginaw, Michigan, USA.
DOI:10.25259/SNI_36_2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Leonard H. Verhey, Theresa A. Elder, Joseph G. Adel. Iatrogenic cortical pseudoaneurysm following ventriculoperitoneal shunt insertion presenting with intraventricular hemorrhage. 13-Sep-2019;10:179
How to cite this URL: Leonard H. Verhey, Theresa A. Elder, Joseph G. Adel. Iatrogenic cortical pseudoaneurysm following ventriculoperitoneal shunt insertion presenting with intraventricular hemorrhage. 13-Sep-2019;10:179. Available from: http://surgicalneurologyint.com/surgicalint-articles/9640/
Abstract
Background: Cerebral pseudoaneurysm formation associated with ventricular catheterization is an exceedingly rare complication that results from direct catheter-induced injury to a vessel. We report a case of intracerebral pseudoaneurysm formation associated with ventricular catheterization in a patient with hydrocephalus following aneurysmal subarachnoid hemorrhage.
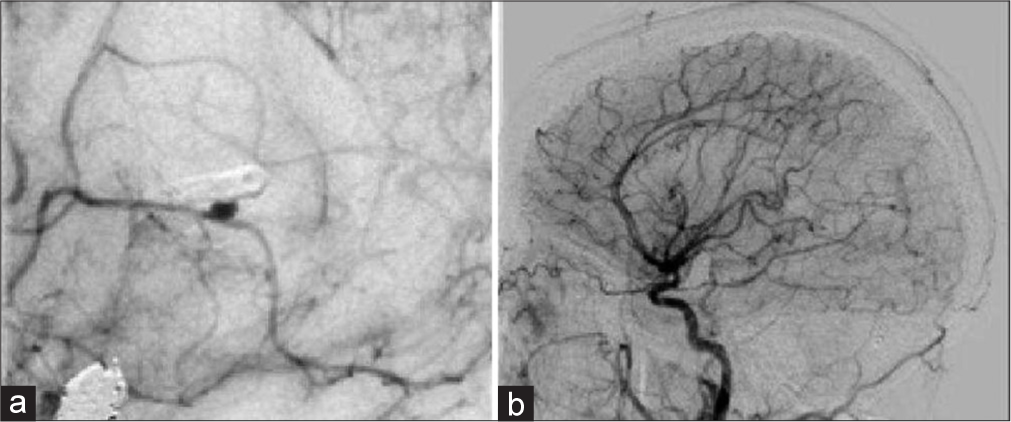
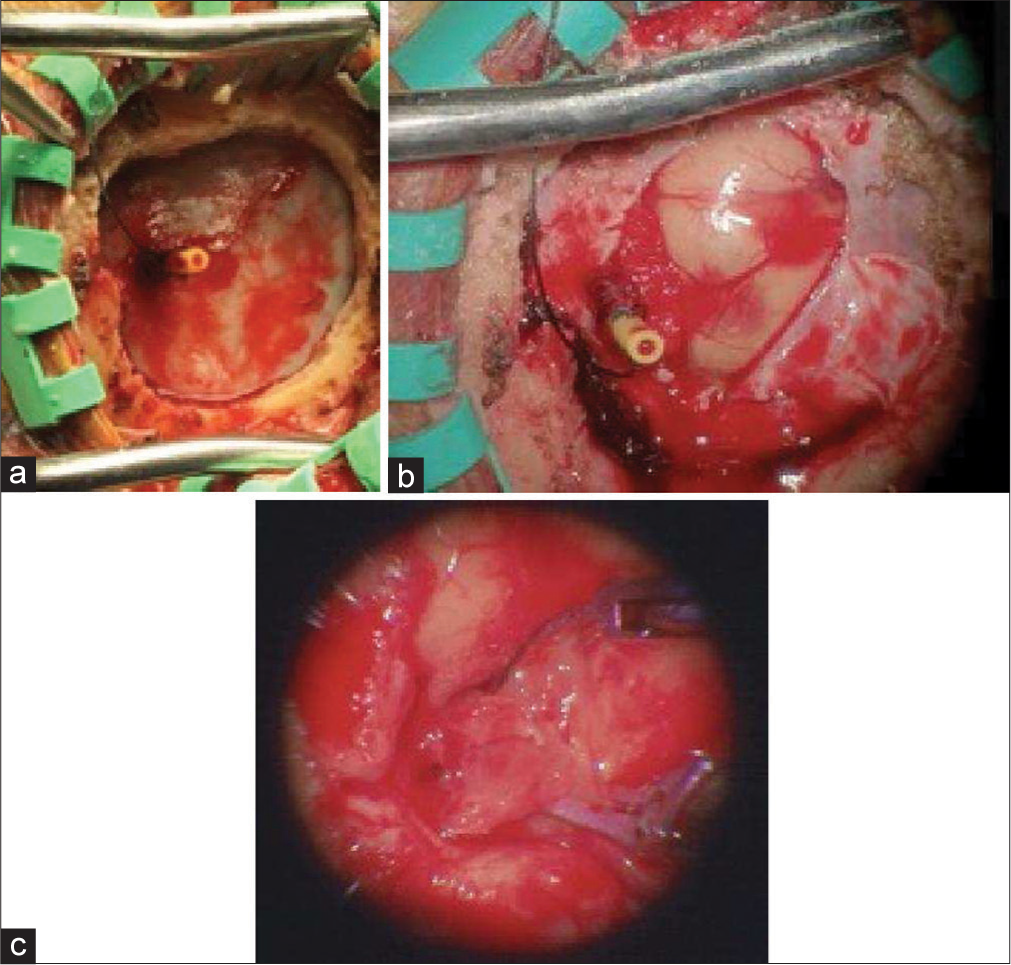
Case Description: The patient presented with aneurysmal subarachnoid hemorrhage and underwent partial endovascular embolization of the offending wide-necked basilar tip aneurysm with the plan for a Stage 2 stent-assisted coiling after initial recovery. Before discharge, a ventriculoperitoneal shunt (VPS) was placed for postaneurysmal hydrocephalus. Three weeks later, she presented with intraparenchymal and intraventricular hemorrhage. Angiography revealed a cortical aneurysm contiguous to the ventricular catheter of the VPS. She underwent microsurgical excision of the aneurysm, and a new VPS was placed after resolution of the intraventricular hemorrhage. She later underwent the second stage of the treatment and had an excellent neurological recovery to an independent state.
Conclusion: Iatrogenic intracerebral pseudoaneurysm formation is an exceedingly rare complication of ventricular catheterization but is associated with significant mortality. Identifying a pseudoaneurysm in this context warrants prompt and definitive treatment with microsurgical or endovascular treatment.
Keywords: Hydrocephalus, Intraventricular hemorrhage, Pseudoaneurysm, Subarachnoid hemorrhage, Ventriculoperitoneal shunt, Ventriculostomy
INTRODUCTION
Ventriculoperitoneal shunt (VPS) insertion is a routine neurosurgical procedure for managing hydrocephalus and achieving cerebrospinal fluid (CSF) flow diversion. Since an excess of 35,000 ventriculostomies is performed annually in the United States,[
CLINICAL PRESENTATION
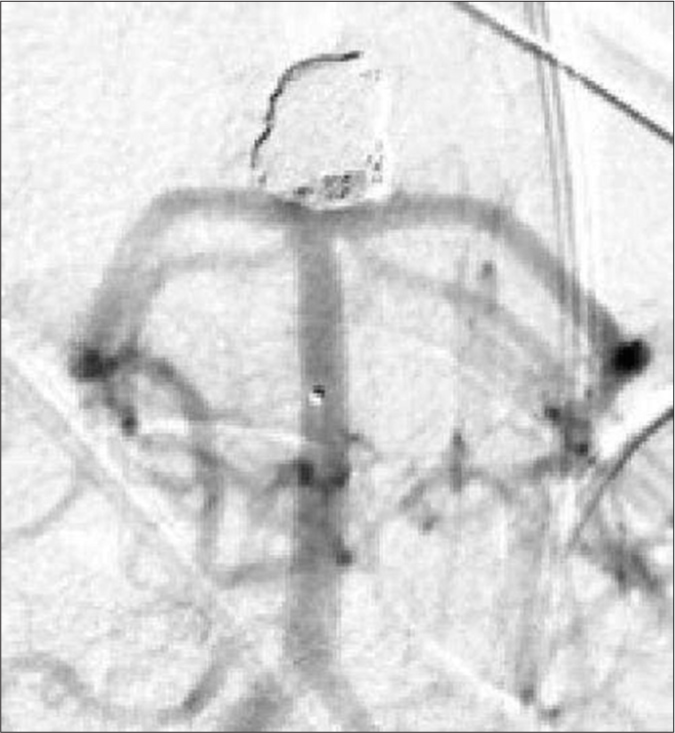
The patient is a 44-year-old female, smoker with a family history of intracranial aneurysms and aneurysmal subarachnoid hemorrhage, who was transferred to our hospital with a Hunt-Hess Grade 3 and Fisher Grade 4 subarachnoid hemorrhage due to a ruptured basilar tip aneurysm [
After discussing treatment options with the family, they elected for endovascular treatment. The aneurysm had a wide neck, so we performed partial embolization leaving a residual neck [
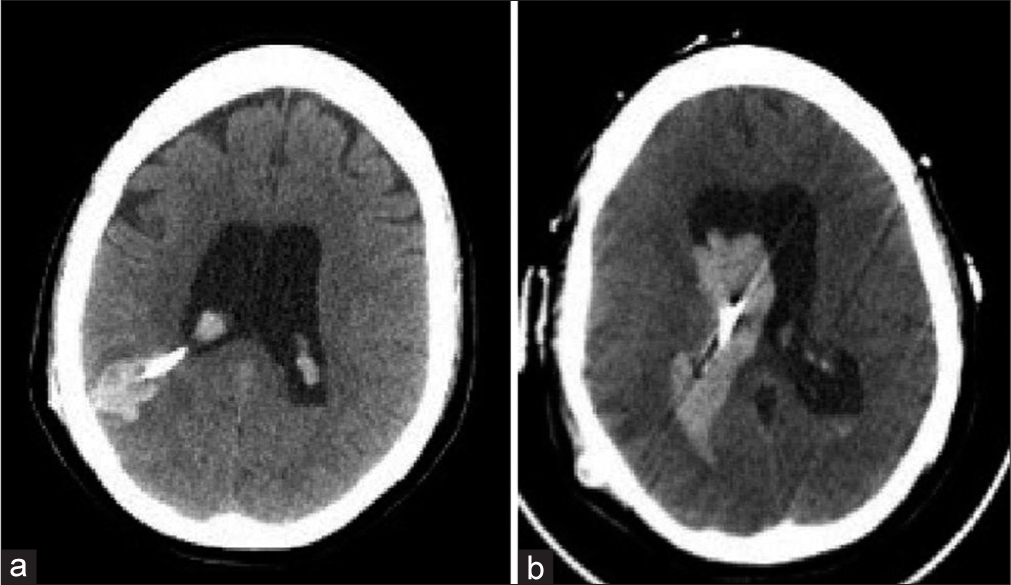
She presented 3 weeks later to an outside hospital with severe headache. Imaging revealed intraventricular hemorrhage for which reason she was transferred back to our institution. On arrival, her neurologic examination was nonfocal, but she rapidly became obtunded with worsening intraparenchymal and intraventricular hemorrhage [
Again, she recovered very well, neurologically intact and was discharged to rehabilitation after insertion of a new VPS. She then returned for elective stent-assisted coiling of the residual aneurysm and continues to be neurologically intact and independent.
DISCUSSION
Pseudoaneurysms are distinguished from true aneurysms in that there is a complete disruption of all vessel layers, whereas in true aneurysms, the tunica adventitia remains intact. In pseudoaneurysm formation, a contained hematoma associated with the vessel maintains the integrity of the vessel but also, when compared to true aneurysms, accounts for their relative instability and high rate of expansion and rupture.[
Traumatic intracranial pseudoaneurysms comprise <1% of all cerebral aneurysms[
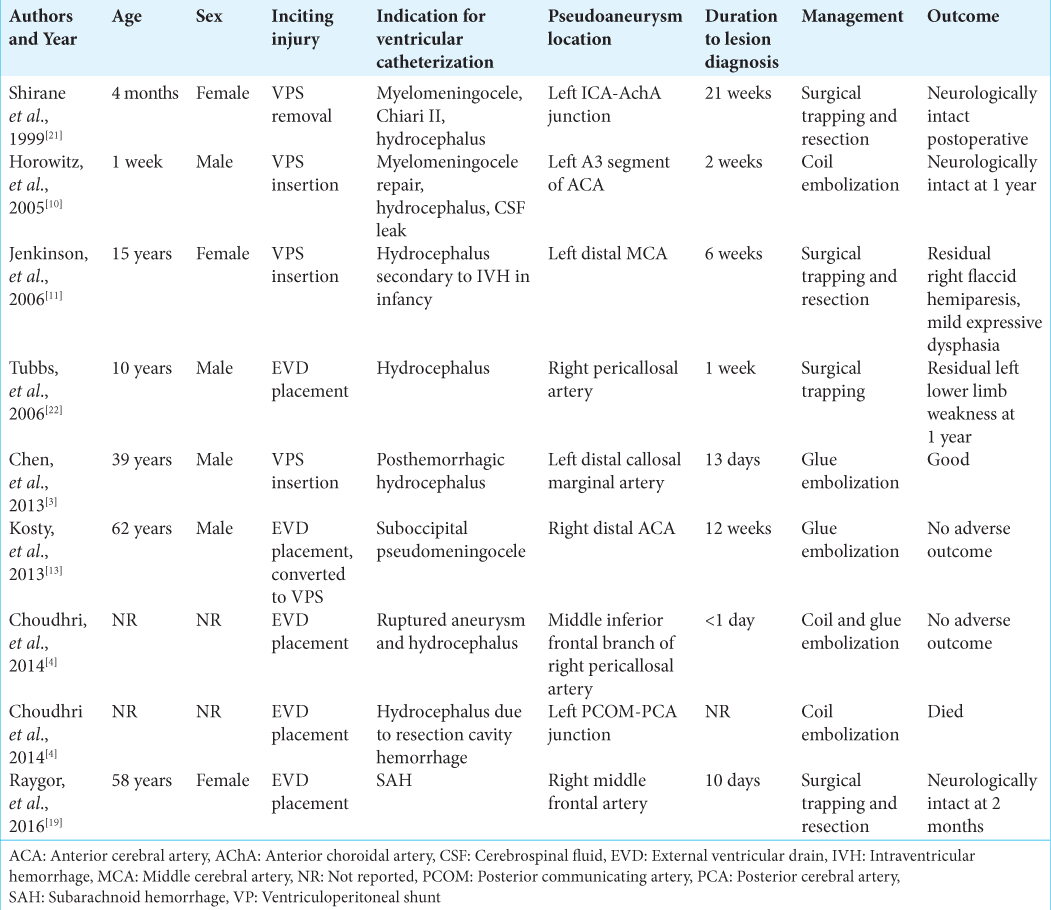
We searched MEDLINE and Embase for articles published in English between January 1, 1960, and March 1, 2018. Search terms were “pseudoaneurysm,” “traumatic aneurysm,” “cerebral,” “intracerebral,” “ventriculostomy,” “external ventricular drain” OR “EVD,” “VPS” OR “VPS,” and “iatrogenic.” References in the original articles were also reviewed. We identified nine cases[
In our case, we postulate two potential offenders that could have contributed to the formation of the aneurysm. During shunt placement, we usually open the dura in a circular fashion utilizing an 11 blade and a Bovie electrocautery. This maneuver, although routinely used and not previously associated with prior complications, could have caused enough thermal injury to damage the vessel. The other potential offenders could be the catheter itself. We usually use an antibiotic impregnated catheter that we sharply cut its blunt end to be able to advance the endoscope. This could have created a sharp edge that injured the vessel during insertion. We have since modified these practices after encountering this complication. Although a connective disorder such as Ehlers-Danlos syndrome could have increased the risk of her developing another aneurysm, we elected not to investigate that given the patient’s lack of family history or features concerning for connective tissue disease and given that we had a good mechanical cause.
The time to intracerebral pseudoaneurysm diagnosis after ventricular catheter insertion varies but can be broadly classified into those pseudoaneurysms that form early (within 2 weeks of catheter insertion) and those that form late (months after catheter insertion).[
Traumatic intracerebral pseudoaneurysms are associated with significant mortality, with reports as high as 50%, especially when treated conservatively.[
CONCLUSION
Iatrogenic intracerebral pseudoaneurysm formation is an exceedingly rare complication associated with ventricular catheterization. Catheter tract hemorrhage may be the heralding sign of a developing pseudoaneurysm and should motivate further investigation with vascular imaging. Discovery of a pseudoaneurysm warrants prompt and definitive treatment with microsurgical clip ligation or endovascular treatment with embolization, flow diversion, or vessel sacrifice.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Bauer DF, Razdan SN, Bartolucci AA, Markert JM. Meta-analysis of hemorrhagic complications from ventriculostomy placement by neurosurgeons. Neurosurgery. 2011. 69: 255-60
2. Binz DD, Toussaint LG, Friedman JA. Hemorrhagic complications of ventriculostomy placement: A meta-analysis. Neurocrit Care. 2009. 10: 253-6
3. Chen Z, Zhang J, Miao H, Niu Y, Feng H, Zhu G. Delayed rupture of iatrogenic cerebral pseudoaneurysms after neurosurgical procedures: Report of two cases. Clin Neurol Neurosurg. 2013. 115: 1552-4
4. Choudhri O, Gupta M, Feroze AH, Heit JJ, Do HM. Endovascular management of external ventricular drain-associated cerebrovascular injuries. Surg Neurol Int. 2014. 5: 167-
5. Ciceri EF, Regna-Gladin C, Erbetta A, Chiapparini L, Nappini S, Savoiardo M. Iatrogenic intracranial pseudoaneurysms: Neuroradiological and therapeutical considerations, including endovascular options. Neurol Sci. 2006. 27: 317-22
6. Dario A, Dorizzi A, Scamoni C, Cerati M, Balcone Grimaldi G. Iatrogenic intracranial aneurysm. Case report and review of the literature. J Neurosurg Sci. 1997. 41: 195-202
7. deSouza RM, Shah M, Koumellis P, Foroughi M. Subarachnoid haemorrhage secondary to traumatic intracranial aneurysm of the posterior cerebral circulation: Case series and literature review. Acta Neurochir (Wien). 2016. 158: 1731-40
8. Gardner PA, Engh J, Atteberry D, Moossy JJ. Hemorrhage rates after external ventricular drain placement. J Neurosurg. 2009. 110: 1021-5
9. Holmes B, Harbaugh RE. Traumatic intracranial aneurysms: A contemporary review. J Trauma. 1993. 35: 855-60
10. Horowitz M, Sharts M, Levy E, Albright AL, Pollack I. Endovascular management of ventricular catheter-induced anterior cerebral artery false aneurysm: Technical case report. Neurosurgery. 2005. 57: E374-
11. Jenkinson MD, Basu S, Broome JC, Eldridge PR, Buxton N. Traumatic cerebral aneurysm formation following ventriculoperitoneal shunt insertion. Childs Nerv Syst. 2006. 22: 193-6
12. Kieck CF, de Villiers JC. Vascular lesions due to transcranial stab wounds. J Neurosurg. 1984. 60: 42-6
13. Kosty J, Pukenas B, Smith M, Storm PB, Zager E, Stiefel M. Iatrogenic vascular complications associated with external ventricular drain placement: A report of 8 cases and review of the literature. Neurosurgery. 2013. 72: ons208-13
14. Larson PS, Reisner A, Morassutti DJ, Abdulhadi B, Harpring JE. Traumatic intracranial aneurysms. Neurosurg Focus. 2000. 8: e4-
15. Lassman LP, Ramani PS, Sengupta RP. Aneurysms of peripheral cerebral arteries due to surgical trauma. Vasc Surg. 1974. 8: 1-5
16. McElroy KM, Malone RJ, Freitag WB, Keller I, Shepard S, Roychowdhury S. Traumatic pseudoaneurysm of the basilar artery. Am J Phys Med Rehabil. 2008. 87: 690-1
17. McLaughlin MR, Wahlig JB, Kaufmann AM, Albright AL. Traumatic basilar aneurysm after endoscopic third ventriculostomy: Case report. Neurosurgery. 1997. 41: 1400-3
18. Overton MC, Calvin TH. Iatrogenic cerebral cortical aneurysm. Case report. J Neurosurg. 1966. 24: 672-5
19. Raygor KP, Mooney MA, Snyder LA, Levitt MR, Albuquerque FC, Spetzler RF. Pseudoaneurysm of distal anterior cerebral artery branch following external ventricular drain placement. Oper Neurosurg (Hagerstown). 2016. 12: 77-82
20. Rosenbaum BP, Vadera S, Kelly ML, Kshettry VR, Weil RJ. Ventriculostomy: Frequency, length of stay and in-hospital mortality in the United States of America, 1988-2010. J Clin Neurosci. 2014. 21: 623-32
21. Shirane R, Kondo T, Yoshida YK, Furuta S, Yoshimoto T. Ruptured cerebral pseudoaneurysm caused by the removal of a ventricular catheter. Case report. J Neurosurg. 1999. 91: 1031-3
22. Tubbs RS, Acakpo-Satchivi L, Blount JP, Oakes WJ, Wellons JC. Pericallosal artery pseudoaneurysm secondary to endoscopic-assisted ventriculoperitoneal shunt placement. Case report. J Neurosurg. 2006. 105: 140-2