- Department of Neurosurgery, Faculty of Medicine, Universitas Airlangga – Dr. Soetomo Academic General Hospital, Surabaya, Indonesia
Correspondence Address:
Tedy Apriawan, Department of Neurosurgery, Faculty of Medicine, Universitas Airlangga – Dr. Soetomo Academic General Hospital, Surabaya, Indonesia.
DOI:10.25259/SNI_629_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Vega Pangaribuan, Tedy Apriawan, Agus Turchan. Occurrence of malignant cerebral infarction following intracranial hematoma evacuation in traumatic brain injury: A case report. 27-Sep-2024;15:349
How to cite this URL: Vega Pangaribuan, Tedy Apriawan, Agus Turchan. Occurrence of malignant cerebral infarction following intracranial hematoma evacuation in traumatic brain injury: A case report. 27-Sep-2024;15:349. Available from: https://surgicalneurologyint.com/surgicalint-articles/13118/
Abstract
Background:Traumatic brain injury-related cerebral infarctions are well-documented in the literature. We want to report a case of malignant cerebral infarction that occurred at the contralateral location of evacuated epidural hematoma 3 days after surgery. The early-onset cerebral infarction’s clinical presentation was already evident during the initial clinical examination, and it resembled “Kernohan’s Notch Syndrome.”
Case Description:A 57-year-old male Indonesian was taken to our Academic General Hospital’s emergency room following a motorcycle accident. His primary complaints were reduced consciousness and left-sided hemiparesis. A head computed tomography (CT) scan revealed an intracerebral hematoma beneath an epidural hematoma (EDH) at the left temporal area. The EDH was surgically removed promptly. The patient’s Glasgow coma scale improved, and they were able to follow commands afterwards. The patient had a decreased consciousness 3 days after the surgery. A malignant infarction of the right middle cerebral artery region was identified from the head CT scan evaluation. He immediately had an emergency decompressive craniectomy and had an improvement of consciousness following the surgery.
Conclusion:It is imperative to reassess the initial clinical signs of Kernohan’s notch phenomenon to determine whether the offending mass was able to generate this clinical phenomenon. Initial cerebral infarction, which occurs concomitantly with traumatic intracranial hematoma, is a possible cause of clinical deterioration following the surgery.
Keywords: Case report, Malignant cerebral infarction, Postoperative, Traumatic brain injury
INTRODUCTION
In this case report, we would like to present a case of malignant middle cerebral artery (MCA) infarction that presented 3 days after the initial injury. The clinical signs have been presented at the emergency department; however, the clinical signs have been overshadowed by the occurrence of epidural hematoma at the contralateral side, mimicking a “Kernohan’s Notch Phenomenon.”
CASE ILLUSTRATION
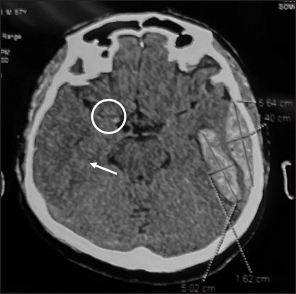
A 57-year-old Indonesian male was taken into the emergency department of our Academic General Hospital by ambulance with a main complaint of decreased consciousness and weakness of left extremities after a motor vehicle collision. At the primary survey, the airway, breathing, and circulation were clear. The Glasgow coma scale (GCS) was E2V1M4, anisocoric pupil right eye 2 mm and left eye 4 mm, positive light reflex on both eyes and left hemiparesis. The computed tomography (CT) scan revealed a 16 cc intracerebral hemorrhage in the temporal area and an epidural hematoma with a maximum thickness of 1.5 cm at the left temporal region [
Figure 1:
Non-contrast head computed tomography scan taken 40 min after the incidence, revealing a left temporal epidural hematoma with thickness of 1.5 cm and left temporal intracerebral hematoma with volume of ± 16 cc. In this slice, there was already a hypodense area (white arrow) and hyperdense middle cerebral artery sign (white circle).
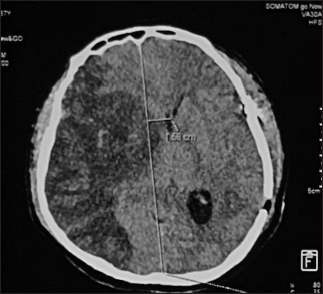
The patient had an immediate epidural hematoma (EDH) evacuation within 30 min after the CT scan was taken. The EDH was surgically removed, and the left temporal intracerebral hematoma (ICH) was not evacuated. Following the surgery, the patient was admitted to intensive care. The patient had improvement of GCS following the surgery with GCS of E4V2M6. Three days after the surgery, the patient had a decrease in consciousness with GCS of E2V2M5. He also had rapid shallow breathing, hypertension, and tachycardia. An electrocardiogram was done revealing a normal sinus rhythm. Since the patient also had multiple costae fractures, a chest X-ray was done, revealing infiltration in both lungs. The patient’s breathing patterns become irregular, with a Cheyne-stokes pattern. The patient was immediately put back on the ventilator. After the patient is stabilized, a non-contrast head CT scan is done. The patient had a malignant infarct of the right MCA region [
A decompressive craniectomy was done immediately after the diagnosis was made. The patient also had a tracheostomy following the decompressive craniectomy. Following the surgery, the patient had an improvement of GCS of E4VxM6. The patient had a chest X-ray evaluation followed by a chest CT scan since there is a suspicion of hemothorax. The diagnosis of the left hemothorax was made 11 days after the initial incidence; a chest tube was placed with an initial production hemorrhagic content of 110 cc. Laboratory examinations, such as the patient’s lipid profile and hemoglobin A1c, were within normal limits. The patient’s condition progressively improved, and he was discharged after 24 days in the hospital with GCS of E4VxM6 and persisted left-sided hemiparesis and motoric aphasia.
Six months following the surgery, the patient’s condition improved. The patient has left hemiparesis and motor aphasia at the time of follow-up, with a Glasgow outcome scale of 3 (dependent on daily support).
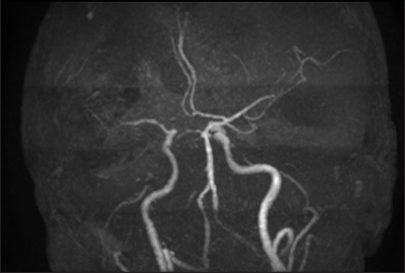
The patient also had magnetic resonance angiography, resulting in decreasing of distal flow of M2 and M3 of the right MCA. There was no appearance of an aneurysm or vascular malformation [
DISCUSSION
In this case report, the patient presented with a clinical presentation of dilated left pupil, left hemiparesis, and decreased consciousness. The patient’s non-contrast head CT scan revealed an epidural hematoma on the left temporal lobe with intracerebral hematoma underneath the lesion. A “Kernohan’s Notch Syndrome” diagnosis due to intracranial hematoma was soon made, and emergency evacuation of epidural hematoma was done. The patient had an improvement in consciousness postoperatively; however, signs of elevated intracranial pressure soon manifested. As the non-contrast head CT scan revealed a malignant MCA infarction, decompressive craniectomy was done, and the patient had immediate improvement following the decompression. A re-evaluation of the presenting clinical and radiological signs was done, resulting in the suspicion of pre-existing cerebral infarction. There was evidence of the right hyperdense MCA sign and hypodense area in MCA territory at the preoperative CT scan, a clinical presentation of left-sided hemiparesis, and decreasing in consciousness 3 days after the hematoma evacuation.
In the acute setting of cerebral infarction, the M1 of the MCA may exhibit localized hyperattenuation, which is indicative of the hyperdense MCA sign. It can appear within 90 min of the start of the stroke; it is among the first radiological indicators of an acute ischemic stroke that is apparent.[
The clinical presentation of acute MCA infarction includes contralateral hemiparesis, contralateral facial palsy, aphasia, and sudden blindness. The risk factors for ischemic stroke include diabetes mellitus, hypertension, and heart disease. Interestingly, in a study by Alshoabi et al., no obvious risk factors were found in 70% of cases with MCA infarction.[
This patient had no clinical risk factors for cerebral infarction. Thus, the presenting left hemiparesis was considered due to “Kernohan’s Notch Syndrome” from the offending intracranial hematoma.
In the setting of a large intracranial hematoma, the temporal lobe’s side-to-side mass effect can result in temporal uncus herniation, significant brainstem displacement, and ultimately, compression of the contralateral cerebral peduncle against the cerebellar tentorium’s free edge. When this condition occurs, injury to the contralateral corticospinal tract that runs through the cerebral peduncle causes patients to have a “paradoxical” motor deficiency ipsilateral to the side of the lesion.[
On re-evaluation, the EDH and ICH at the left temporal lobe were not the cause of the initial clinical presentation of the left hemiparesis. The presence of a hyperdense right MCA sign and hypodense area at the right temporal lobe in the initial head CT Scan support the possibility of cerebral infarction as the cause of the left hemiparesis. The deteriorating condition 2 days following the intracranial hematoma evacuation and the presence of malignant right MCA infarction further support this diagnosis.
In patients with an early onset isolated ischemic stroke, intravenous alteplase or mechanical thrombectomy is a recommended treatment. However, one of the exclusion criteria for fibrinolysis is significant head trauma 3 months prior to the stroke onset.[
CONCLUSION
Cerebral infarction can present concomitantly with contralateral intracranial hematoma, and it may mimic “Kernohan’s Notch Syndrome.” Re-evaluation of the preoperative clinical presentation and imaging may aid in the diagnosis of pre-existing cerebral infarction.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Albano S, Bacani MG, Omuro A. A case report examining a contraindication for mechanical thrombectomy in the setting of a large vessel occlusion and a concurrent contralateral intracranial hemorrhage. Cureus. 2021. 13: e13956
2. Alshoabi S, Alnajmani R, Shamsuddin M, Gameraddin M. Early signs of middle cerebral artery infarction on multidetector computed tomography: Review of 20 cases. Brain Circ. 2019. 5: 27-31
3. Beucler N, Cungi PJ, Baucher G, Coze S, Dagain A, Roche PH. The Kernohan-Woltman notch phenomenon: A systematic review of clinical and radiologic presentation, surgical management, and functional prognosis. J Korean Neurosurg Soc. 2022. 65: 652-64
4. Chieng JS, Singh DR, Chawla A, Peh WC. The hyperdense vessel sign in cerebral computed tomography: Pearls and pitfalls. Singapore Med J. 2020. 61: 230-7
5. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019. 50: e344-418