- Department of Surgery, University of Baghdad, College of Medicine, Al Risafa, Baghdad, Iraq
- Department of Neurosurgery, Dow University of Health Sciences, Karachi, Pakistan
- Department of Neurosurgery, Faculty of Medicine, Zagazig University, Al-Sharqia Governorate, Zagazig, Egypt
- Department of Neurosurgery, Neurosurgery Teaching Hospital, Al Risafa, Baghdad, Iraq
Correspondence Address:
Mustafa Ismail, Department of Neurosurgery, Neurosurgery Teaching Hospital, Al Risafa, Baghdad, Iraq.
DOI:10.25259/SNI_368_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Ahmed Shakir Ali Al-Wassiti1, Danisha Kumar2, Toka Elboraay3, Mustafa Ismail4. Orbital varices: Epidemiology, clinical presentation, and treatment outcomes – A scoping review. 26-Jul-2024;15:258
How to cite this URL: Ahmed Shakir Ali Al-Wassiti1, Danisha Kumar2, Toka Elboraay3, Mustafa Ismail4. Orbital varices: Epidemiology, clinical presentation, and treatment outcomes – A scoping review. 26-Jul-2024;15:258. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13012
Abstract
Background: Orbital varices are vein dilations in the orbit presenting various symptoms. This scoping review synthesizes existing evidence on their epidemiology, clinical features, and treatment efficacy.
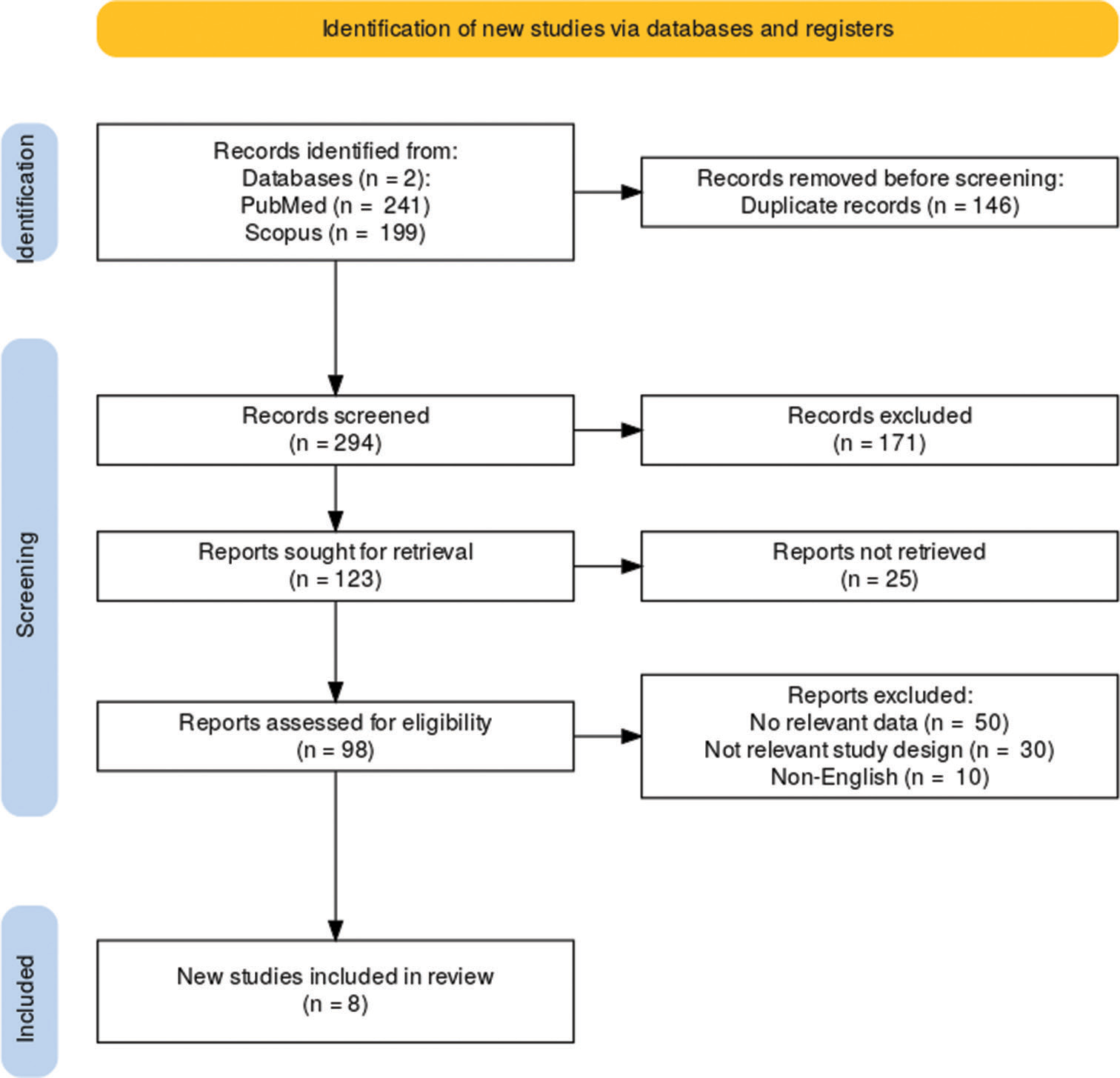
Methods: Literature was reviewed according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. PubMed and Scopus were searched until April 31, 2024, for articles on clinically diagnosed ocular varices detailing diagnostic methods, treatments, and outcomes. Exclusions were reviews, animal studies, and incomplete case reports. Data on study characteristics, diagnosis, management, and outcomes were extracted and assessed for quality and bias.
Results: Eight studies met the inclusion criteria, with sample sizes ranging from 4 to 30 and ages from 1 to 87 years. Diagnostic tools included magnetic resonance imaging and computed tomography, while treatments ranged from conservative methods to invasive procedures and radiosurgery. Notably, higher symptom resolution rates were associated with observational strategies and minimally invasive surgeries. However, Gamma Knife radiosurgery, although promising, posed risks of vision impairment in some cases.
Conclusion: The management of orbital varices has evolved significantly with newer, less invasive techniques improving outcomes and reducing recovery times. Despite advancements, challenges such as disease recurrence and the need for personalized treatment regimens persist, underscoring the ongoing need for research to refine and standardize treatment approaches.
Keywords: Minimally invasive surgery, Orbit, Orbital varices, Radiosurgery, Venous varix
INTRODUCTION
Orbital varices are a specific type of aberrant blood vessels in the orbit. They are characterized by venous enlargements that are unusually uncommonly large, showing different symptoms due to their size, situation, and the presence of phlebectasia.[
Recent studies point to the varying presentations and the managements available in dealing with orbital varices. For example, Mokhtarzadeh et al.[
Understanding and correlating the clinical presentation of a patient with the response to treatment is important to alter the management strategy for orbital varices optimally. This review aims to provide clinicians with a consolidated source of information on the epidemiology, clinical features, diagnostic approaches, and treatment outcomes of orbital varices, thereby aiding in the recognition and effective management of this complex entity.
MATERIALS AND METHODS
Literature search
A comprehensive literature search was conducted following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.[
Study selection
Inclusion and exclusion criteria were carefully defined in an effort to ensure that the data retrieved for the study were relevant and accurate. The studies were included if they involved patients with clinically diagnosed orbital varices and had described in detail the methods of diagnosis, the different types of approaches to treatment adopted, and the outcomes post-treatment, with the consideration that all the studies must be published in English. Exclusion criteria were as follows: Reviews of the literature, chapters in books, and studies that had included animal models or cadaveric data. Further, exclusion included studies not directly related to orbital varices, studies in which precise clinical data regarding diagnosis and treatment outcomes were not described, and case reports involving a small number of cases with an inadequate sample or not having enough detailed clinical follow-up. This stringent selection process was devised to obtain the most accurate and applicable information on the subject of orbital varices.
Two reviewers (M.I. and D.K.) independently screened the titles and abstracts of the articles retrieved. Discrepancies were resolved through discussion or, if needed, by consulting a third reviewer (A.A.). Full texts of potentially relevant studies were then assessed for eligibility based on the predefined criteria. References of selected articles were hand searched to identify additional studies that met the inclusion criteria.
Data extraction
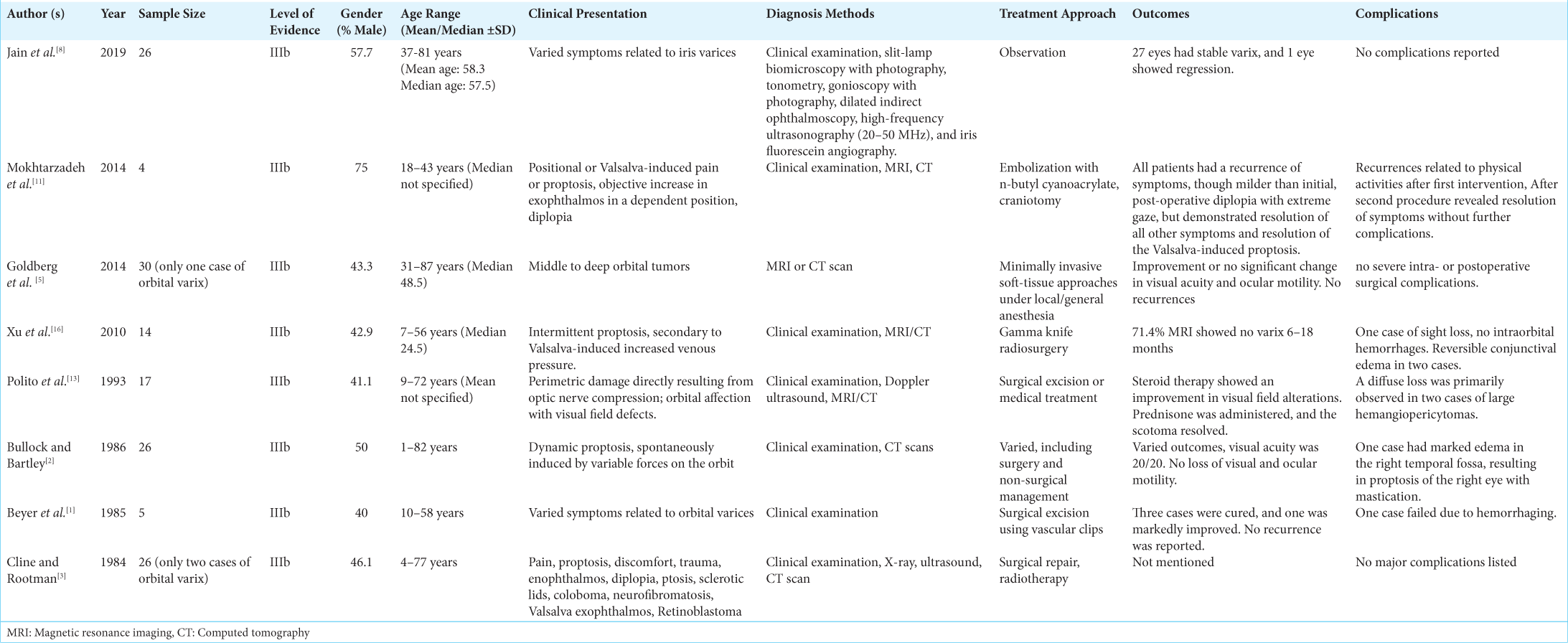
Data extraction was performed by one reviewer (D.K.) and verified independently by two other reviewers (M.I. and A.A.) Extracted information included authors, year of publication, sample size, patient demographics (age and gender), clinical presentation, methods of diagnosis, treatment modalities employed, clinical outcomes, and any reported complications. Details regarding the type and frequency of follow-up assessments, as well as any long-term care plans, were also collected.
Data synthesis and quality assessment
The primary outcomes of interest were the clinical efficacy of treatment modalities and patient outcomes following interventions for orbital varices. Each study’s level of evidence was assessed according to the Oxford Center for Evidence-Based Medicine 2011 guidelines. The risk of bias for each included study was evaluated independently by two authors (M.I. and D.K.) using the Joanna Briggs Institute’s checklists for observational studies and it showed an overall low bias [Supplementary File 1].[
RESULTS
Study selection and characteristics
A comprehensive search and review process resulted in the inclusion of eight pivotal studies out of 440, spanning from 1984 to 2019, each contributing unique insights into the management of orbital varices. These studies encompass a variety of methodologies ranging from case series to observational cohorts, with sample sizes varying from as few as 4 to as many as 30 subjects [
Diagnostic and management approaches
The diagnostic tools used in all studies included only advanced imaging modalities, such as magnetic resonance imaging (MRI) and computed tomography scans, with clinical evaluations and some tests, such as high-frequency ultrasonography and fluorescein angiography. Treatment approaches showed a high level of variation and, in doing so, showed an increasingly conservative and technological advancement in approach over time, with significant differences between each study. Particularly, Jain et al.[
Treatment outcomes
In most of the studies mentioned, the results of treatment applied in the case of orbital varices were favorable, and improvement of symptoms was noticed in the majority of cases. For example, Jain et al.[
Complications
In all studies, complications were rare and mostly minor, with exceptions like the reported vision loss in Xu et al.[
DISCUSSION
The management of orbital varices poses significant challenges due to the complex anatomical and physiological characteristics of the orbit. Recent literature and case studies reflect a diversity of management strategies and outcomes, highlighting the importance of tailored approaches based on individual patient presentations.
Surgical, non-surgical, and observational management
In earlier interventions, surgical excision was often considered a primary treatment for symptomatic orbital varices. Beyer et al.[
Role of embolization
Embolization techniques have also evolved, offering a less invasive alternative or adjunct to surgery. Xiao et al.[
Advances in radiosurgery
The development of radiosurgical techniques has opened a more optimistic view. Xu et al.[
Case report insights
Individual case reports provide deeper insights into unique presentations and management challenges. For example, Tsai et al.[
Furthermore, other complications can include thrombosis, leading to embolic events such as retinal artery occlusion, spontaneous hemorrhage causing acute proptosis and vision loss, and infection leading to orbital cellulitis.[
Limitations
Inherent, however, are some limitations given the variation in research designs and the variation in methods of treatment: It uses retrospective data and is based on data that are already accessible. Much stronger prospective study designs are needed for further enlightenment on this and in techniques for the management of orbital varices, more so in their long-term efficacy and recurrence post-treatment.
In conclusion, ocular varices have evolved from conventional surgical techniques to less invasive ones, including radiosurgery options; all this contributes to better outcomes with less complication. While surgical intervention remains a cornerstone in the management of orbital varices, observational and less invasive approaches are gaining recognition. However, the problem is likely to be a recurring one and, thus, calls for a tailor-made, patient-centered approach to optimize the quality of care administered to these individuals.
CONCLUSION
The management of orbital varices has evolved significantly from classical and invasive surgical techniques toward minimally invasive approaches, aided by adjunctive embolization and radiosurgery. Our review and analysis of the literature illustrate this evolution, with studies highlighting that by the effectiveness of Gamma Knife radiosurgery in reducing varices with minimal complications, compared to traditional surgical approaches. This shift reflects a broader trend toward less invasive interventions, reducing the risk of morbidity and improving recovery times. However, despite these advancements, the risk of recurrence remains, underscoring the need for a patient-centered approach based on individual factors. Future research should focus on long-term outcomes and the development of standardized protocols to further optimize the management of this complex condition.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
SUPPLEMENTARY FILE
References
1. Beyer R, Levine MR, Sternberg I. Orbital varices: A surgical approach. Ophthalmic Plast Reconstr Surg. 1985. 1: 205-10
2. Bullock JD, Bartley GB. Dynamic proptosis: Asign of orbital varices. Arch Ophthalmol. 1986. 104: 1512-6
3. Cline RA, Rootman J. Enophthalmos: A clinical review. Ophthalmology. 1984. 91: 229-37
4. Couch SM, Garrity JA, Cameron JD, Cloft HJ. Embolization of orbital varices with N-butyl cyanoacrylate as an aid in surgical excision: Results of 4cases with histopathologic examination. Am J Ophthalmol. 2009. 148: 614-8.e1
5. Goldberg RA, Rootman DB, Nassiri N. Orbital tumors excision without bony marginotomy under local and general anesthesia. J Ophthalmol. 2014. 2014: 424852
6. Hayreh SS, Podhajsky PA, Zimmerman MB. Retinal artery occlusion: Associated systemic and ophthalmic abnormalities. Ophthalmology. 2009. 116: 1928-36
7. Howick JChalmers IGlasziou PGreenhalgh THeneghan CLiberati A. Explanation of the 2011 Oxford Centre for evidence-based medicine (OCEBM) levels of evidence (background document). Available from: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence [Last accessed on 2024 May 07].
8. Jain S, Desai RU, Charalel RA, Quencer K, Doshi AH, Feuer W. The efficacy and safety of propranolol as first-line treatment for infantile hemangiomas. Pediatrics. 2019. 143: e20183224
9. Joanna Briggs Institute. Checklist for case series. Available from: https://jbi.global/critical-appraisal-tools [Last accessed on 2024 May 07].
10. Lizana J, Reinoso CM, Aliaga N, Marani W, Montemurro N. Bilateral central retinal artery occlusion: An exceptional complication after frontal parasagittal meningioma resection. Surg Neurol Int. 2021. 12: 397
11. Mokhtarzadeh A, Garrity JA, Cloft HJ. Recurrent orbital varices after surgical excision with and without prior embolization with n-butyl cyanoacrylate. Am J Ophthalmol. 2014. 157: 447-50
12. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ. 2021. 372: n71
13. Polito E, Burroni L, Pichierri P, Loffredo A, Vattovani O. Choroidal nevi: A comparison of the clinical and histopathological features with age. Arch Ophthalmol. 1993. 111: 645-50
14. Tsai A, Fong K, Lim W, Al Jajeh I, Chuah CT, Rootman J. Bilateral orbital varices: An approach to management. Ophthalmic Plast Reconstr Surg. 2008. 24: 486-8
15. Xiao LH, Lu XZ, Wang Y, Yang XJ, Wei HF, Zhu H. Preliminary observations of embolization treatment of orbital varices with Glubran 2 acrylic glue. [Zhonghua Yan Ke Za Zhi] Chin J Ophthalmol. 2009. 45: 436-40
16. Xu D, Liu D, Zhang Z, Zhang Y, Song G. Gamma knife radiosurgery for primary orbital varices: A preliminary report. Br J Ophthalmol. 2010. 95: 1264-7