- College of Medicine, Jouf University, Sakaka, Saudi Arabia
- College of Medicine, King Saud Bin Abdulaziz University for Health Sciences, Jeddah, Saudi Arabia
- King Abdullah International Medical Research Center, Jeddah, Saudi Arabia
- College of Medicine, Alfaisal University, Riyadh, Saudi Arabia
- College of Medicine, Taif University, Taif, Saudi Arabia
- Department of Neurosurgery, King Faisal Specialist Hospital and Research Centre, Riyadh, Saudi Arabia
- Department of Neuroscience, Ministry of the National Guard Health Affairs, Jeddah, Saudi Arabia
Correspondence Address:
Abdulhadi Y. Algahtani, King Abdullah International Medical Research Center, Jeddah, Saudi Arabia.
DOI:10.25259/SNI_331_2024
Copyright: © 2024 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, transform, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Khalid M. Alanazi1, Abdulaziz M. Alghamdi2,3, Faisal H. Ghazal4, Faisal S. AlQurashi5, Ahmed Abdulaziz Alqerafi2, Khalid Talal Alghamdi6, Abdulhadi Y. Algahtani2,3,7. Risk factors associated with postoperative cerebrospinal fluid leak after endoscopic endonasal skull base surgery: A single-center retrospective cohort study. 02-Aug-2024;15:272
How to cite this URL: Khalid M. Alanazi1, Abdulaziz M. Alghamdi2,3, Faisal H. Ghazal4, Faisal S. AlQurashi5, Ahmed Abdulaziz Alqerafi2, Khalid Talal Alghamdi6, Abdulhadi Y. Algahtani2,3,7. Risk factors associated with postoperative cerebrospinal fluid leak after endoscopic endonasal skull base surgery: A single-center retrospective cohort study. 02-Aug-2024;15:272. Available from: https://surgicalneurologyint.com/?post_type=surgicalint_articles&p=13021
Abstract
Background: Over the past two decades, endoscopic endonasal skull base surgery (EESBS) has revolutionized the treatment of skull base tumors by enabling minimal access to resect significant pathologies such as meningiomas, pituitary adenomas, and chordomas. Despite its efficacy, complications such as cerebrospinal fluid (CSF) leak pose significant challenges, with an average incidence of 8.9% following EESBS. Therefore, our study aims to investigate the risk factors associated with postoperative CSF leak after employing an endoscopic endonasal approach for skull base surgery, focusing on patients treated at King Abdul-Aziz Medical City in Jeddah and King Abdullah Medical City in Makkah, Saudi Arabia.
Methods: A retrospective review of patients who underwent an endoscopic endonasal approach for the resection of intradural skull base pathology between January 2016 and December 2022 was performed with a total of 51 patients. Basic demographic data were collected, along with patient comorbidities, presenting symptoms, tumor pathology, tumor site, the extent of resection, and outcomes.
Results: 51 participants were analyzed, with a mean age of 43.41. Male participants comprised (58.8%), while headaches were the most common symptom (74.5%), followed by visual disturbances (51.0%). Nonsecretory tumors predominated, primarily located in the sellar and suprasellar regions (58.8%). Gross total resection was performed in the majority (56.9%), with a 9.8% incidence of postoperative CSF leak. Notably, all four patients with CSF leak experienced preoperative headaches. Hypertension was prevalent in Cases 1 and 4, with Case 4 having a history of neurological disease and radiation therapy. Anterior skull base tumors were most frequent in Cases 3 and 4.
Conclusion: The incidence of CSF leakage after surgery in this study was similar to that previously reported. It is worth noting that repeated surgeries may increase the risk of postoperative CSF leakage. Therefore, it is important to carefully evaluate the surgical approach for tumor removal and skull base reconstruction, considering the tumor characteristics and the patient’s overall condition.
Keywords: Cerebrospinal fluid leak, Endoscopic endonasal skull base surgery, Postoperative outcomes, Risk factors, Saudi Arabia, Skull base tumors
INTRODUCTION
Endoscopic endonasal skull base surgery (EESBS) has completely changed how skull base tumors are treated over the past two decades. This method has evolved to allow minimal access to the resection of significant skull bases tumors, such as meningiomas, pituitary adenomas, and chordomas.[
Few studies have compared the rates of postoperative CSF leakage in different tumor types. The postoperative repair can be affected by a variety of parameters depending on the type of tumor, including tumor size, location, and whether it requires subarachnoid dissection. After reconstruction of dural defects with a nasoseptal flap, endoscopic surgery for tumors located in the central skull base has been shown to have higher rates of CSF leakage than endoscopic surgery for tumors located in the anterior skull base.[
According to our knowledge, no studies have been conducted in Saudi Arabia in general or at our facility in particular to explore these issues. Therefore, in this study, we aimed to investigate the risk factors associated with postoperative CSF leakage after an endoscopic endonasal approach for skull base surgery.
MATERIALS AND METHODS
We carried out a retrospective study from January 01, 2016, to December 31, 2022, at King Abdul-Aziz Medical City, Jeddah, and King Abdullah Medical City, Makkah . Fifty-one patient profiles diagnosed with skull base pathology and treated using an endoscopic endonasal approach to resect the tumor, who were followed up for at least 3 months, were reviewed. Meanwhile, incomplete medical records or patients with other causes of CSF leakage, such as skull base trauma, were excluded.
The information obtained included patient demographics such as age, sex, and body mass index (BMI). We also collected comprehensive clinical data for our cases, encompassing the duration of symptoms, presence of co-morbidities, history of skull base trauma, utilization of perioperative lumbar drainage, and the presence of any clinical or radiological indicators of preoperative hydrocephalus. In addition, we ensured that tumor data such as location, surgical indication, size of the dural defect, and tumor pathology were available. For the outcome, we obtained the surgical location and reconstruction technique as well as postoperative complications.
RESULTS
A total of 51 participants were included in the study, with a mean age of 43.41 (standard deviation = 15.404). Most participants were from King Abdul-Aziz Medical City, Jeddah (80.4%), and the rest were from King Abdullah Medical City, Makkah (19.6%). Male participants outnumbered female participants, 58.8% and 41.2%, respectively. The most common symptom among the participants was a headache (74.5%). Visual disturbances were prevalent (51.0%). A smaller percentage of participants reported other symptoms, such as nausea/vomiting (27.5%), disturbed sensation (19.6%), and weakness (11.8%). Seizures, loss of consciousness, and hydrocephalus were relatively rare, experienced by <10% of the participants. A family history of the disease and a history of other tumors were reported by 17.6% of the participants [
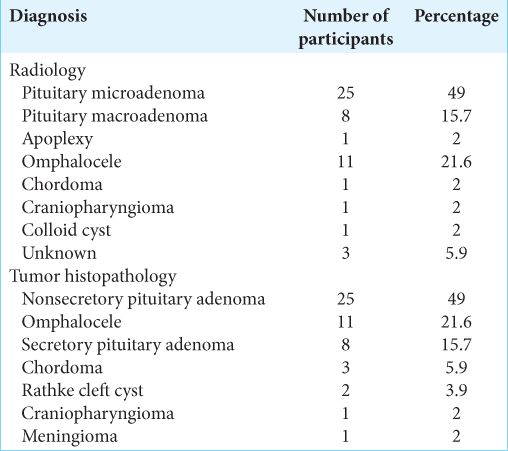
All cases were of primary origin. The radiological diagnosis varied among participants, with the most common being pituitary microadenoma (49.0%), followed by omphalocele (21.6%) and pituitary macroadenoma (15.7%). Similarly, the tumor histopathology varied, with nonsecretory tumors being the most common (49.0%) [
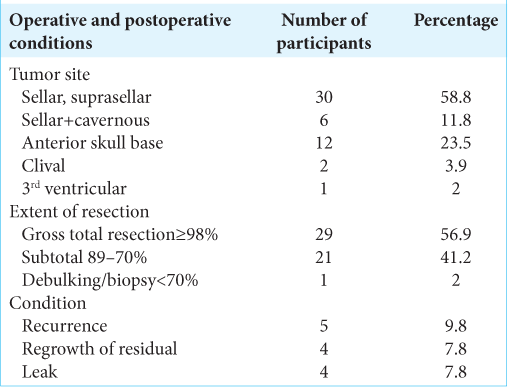
The sellar and suprasellar regions were the most common sites for tumors (58.8%), followed by the anterior skull base (23.5%) and sellar with extension to cavernous regions (11.8%). Regarding the extent of resection, the majority of the participants underwent gross total resection (56.9%), followed by subtotal resection (41.2%). Finally, regarding postsurgical complications, recurrence was reported in 9.8% of the cases, while a leak was reported in four patients (7.8%) [
To provide a thorough summary of the medical profiles and tumor characteristics of the four patients who experienced postoperative CSF leak, all four patients experienced headaches as a symptom before their diagnosis. For cases 1 and 4, hypertension was a common chronic condition. Case 4 had a history of neurological diseases, specifically bilateral sensorineural hearing loss/chronic suppurative otitis media (SNHL/CSOM), and had undergone radiation therapy. The most common tumor site was the anterior skull base, as identified in cases 3 and 4 [
DISCUSSION
EESBS is a well-established surgical approach that adds significantly to the neurosurgery field for approaching anterior skull base tumors. However, this approach has been limited by complications such as CSF leaks, and the risk factors for these complications can be divided into pre-, intra, and postoperative risk factors.
Preoperative risk factors in individual patients compared to existing literature
The preoperative phase is pivotal in assessing the risk profiles of patients undergoing EESBS. After reviewing the literature, we identified several preoperative risk factors.
The age range of our patients, from 33 to 57 years, with an equal distribution between males and females, offers a demographic representation that is less discussed in early literature, such as Jho and Carrau,[
The duration of symptoms, ranging from 4 months to 2 years in our patients, may indicate the progressive nature of the underlying pathology. Ozawa et al.[
In the context of EESBS, obesity is acknowledged as a risk factor for the development of postoperative CSF leaks, which were not directly measured in the current study. The correlation between a higher BMI and increased rates of CSF leak post-surgery is underscored in the findings of Fraser et al.[
A history of smoking is a critical preoperative factor to consider because of its well-established association with poor healing outcomes. A history of smoking has been linked to an increased risk of surgical site infections, impaired wound healing, and other complications that can adversely affect postoperative recovery.[
Intraoperative risk factors in individual patients compared to existing literature
Intraoperatively, the location and nature of the lesion are among the most significant factors influencing surgical strategy and associated risks. Primary versus metastatic lesions are crucial, as Patel et al.[
The radiological diagnosis of pituitary macroadenoma, clivus chordoma, and frontoethmoidal encephalocele, along with the associated histopathological diagnoses of nonsecretory pituitary adenoma, chordoma, and CSF rhinorrhea, presents a spectrum of surgical challenges. Batra et al.,[
The tumor site, particularly in the anterior skull base, as seen in two of our patients, requires a nuanced surgical approach to manage the complex anatomy and achieve effective dural reconstruction. Gruss et al.[
Factors that increase the risk of CSF leakage following transsphenoidal surgery for pituitary adenomas include tumor size, adenoma consistency, and intraoperative CSF leakage.[
A detailed comparison of preoperative and intraoperative risk factors with established literature underscores the importance of individualized patient assessment. The distinct profiles presented by our patients highlight the necessity of a tailored approach to EESBS to manage the complex interplay between factors that can influence surgical outcomes. This discussion adds to the body of knowledge by clarifying the impact of these risk factors in the context of current surgical practices.
Postoperative risk factors associated with CSF leak
When comparing endoscopic and microscopic approaches in transsphenoidal surgery, the endoscopic method seems to offer a slight advantage in reducing CSF leakage.[
A review was conducted on delayed CSF leaks following the treatment of skull base tumors. Nine patients who experienced CSF leak at least 3 months after treatment were examined. These findings indicate that individuals with delayed CSF leaks were more likely to have a history of radiation exposure and might exhibit symptoms of meningitis. The study recommends maintaining a high level of suspicion for CSF rhinorrhea in patients with a history of skull base tumors even years after treatment[
Preventive and management strategies for CSF leakage
Placement of a postoperative lumbar drain is commonly employed to address temporary spikes in ICP or to create lower-than-normal pressure during the initial healing period. In this series, not all drains were utilized to prevent leaks during surgery but to deter leaks after surgery, specifically in patients with high-flow leaks where they were placed after the procedure. While lumbar drains can be effective in preventing intraoperative leaks, they are not typically applicable to high-flow leaks stemming from significant dural defects resulting from tumor resection or surgical access to the tumor.[
Analysis of postoperative CSF leakage rates over time has declined in recent years. This reduction in incidence is attributed to several factors, including the introduction of a nasoseptal flap and the increased expertise of surgeons. The latter signifies the learning curve associated with adopting these relatively new approaches and techniques, which is distinct from the vascularized reconstruction in multivariate analysis. This underscores the significance of clinical experience and the concentration of such cases at specialized centers in mitigating complication rates.[
As vascularized flaps in EESBS have progressed, the use of pedicled nasoseptal flaps for skull base reconstruction has also increased. A systematic review revealed that vascularized flaps are associated with a reduced occurrence of postoperative CSF leaks.[
Perioperative lumbar drainage is frequently employed to alleviate ICP and prevent postoperative CSF leaks subsequent to EESBS for skull base lesions.[
The primary methods used to prevent postoperative CSF leaks include free tissue grafts, vascularized flaps, gasket sealing, and lumbar drains.[
Another study[
A systematic review addressed the prevention of postoperative CSF leakage after the endoscopic endonasal approach. This review included 34 case–control and cohort studies with 9144 patients who underwent transsphenoidal surgery for pituitary adenoma. This review identified several risk factors for postoperative CSF leakage, including tumor size, adenoma consistency, revision surgery, and intraoperative CSF leakage. In addition, the review showed that the endoscopic approach had a slight protective benefit compared to the microscopic approach in preventing CSF leakage. This suggests that screening for these risk factors and considering the endoscopic approach may help reduce complications related to CSF leakage.[
A meta-analysis[
The dural flap technique for dural opening and closure during endoscopic pituitary surgery helped restore normal anatomy after tumor removal and provided a better physiological barrier between the sinonasal cavity and intrasellar compartment. A previous study reported no postoperative CSF leakage in cases in which the dural flap technique was used.[
Overall, the literature supports the use of the endoscopic endonasal approach for managing CSF leaks, with high success rates and low morbidity. The dural flap technique and pedicled nasoseptal flap are effective methods for dural opening and closure, providing optimal anatomical reconstruction and preventing postoperative leakage.
A study evaluated a method for preventing postoperative CSF leakage using autologous fascia lata grafts and pressure-controlled spinal drainage in patients with skull base lesions requiring a wide opening of the ventral dura. The researchers retrospectively analyzed data from 50 cases, including recurrent cases, and found that the multilayer closure method with pressure-controlled spinal drainage is simple, safe, and effective for preventing postoperative CSF leakage.[
A study[
Based on a systematic review, endoscopic repair techniques can be effective in managing postoperative CSF leaks following an endoscopic endonasal approach. However, the specific management strategy may vary depending on the individual case, with vascularized mucosal flap repair being a commonly used technique.[
CONCLUSION
This study provides a comprehensive analysis of the risk factors that contribute to CSF leakage following EESBS. It assesses preoperative conditions, such as hypertension and neurological disorders, intraoperative challenges, including lesion characteristics and surgical techniques, and postoperative complications, emphasizing the significance of individualized patient assessments. Through a meticulous comparison with global studies, this study enhances our understanding of effective management strategies, advocating the adoption of vascularized flaps, meticulous lumbar drainage practices, and precise endoscopic repair methods. These insights are pivotal for refining surgical protocols to reduce the incidence of CSF leaks and improve patient outcomes. This study plays an important role in advancing patient care standards by bridging the gaps in the existing literature and introducing novel findings.
Ethical approval
The research/study was approved by the Institutional Review Board at King Abdullah International Medical Research Center, number NRJ23J/184/07, dated October 09, 2023.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
References
1. Allen KP, Isaacson B, Purcell P, Kutz JW, Roland PS. Lumbar subarachnoid drainage in cerebrospinal fluid leaks after lateral skull base surgery. Otol Neurotol. 2011. 32: 1522-4
2. Berker M, Aghayev K, Yücel T, Hazer DB, Onerci M. Management of cerebrospinal fluid leak during endoscopic pituitary surgery. Auris Nasus Larynx. 2013. 40: 373-8
3. Borg A, Kirkman MA, Choi D. Endoscopic endonasal anterior skull base surgery: A systematic review of complications during the past 65 years. World Neurosurg. 2016. 95: 383-91
4. Cohen S, Jones SH, Dhandapani S, Negm HM, Anand VK, Schwartz TH. Lumbar drains decrease the risk of postoperative cerebrospinal fluid leak following endonasal endoscopic surgery for suprasellar meningiomas in patients with high body mass index. Oper Neurosurg (Hagerstown). 2018. 14: 66-71
5. Fang J, Xie S, Li N, Jiang Z. Postoperative complications of endoscopic versus microscopic transsphenoidal pituitary surgery: A meta-analysis. J Coll Physicians Surg Pak. 2018. 28: 554-9
6. Fraser S, Gardner PA, Koutourousiou M, Kubik M, Fernandez-Miranda JC, Snyderman CH. Risk factors associated with postoperative cerebrospinal fluid leak after endoscopic endonasal skull base surgery. J Neurosurg. 2018. 128: 1066-71
7. Gruss CL, Al Komser M, Aghi MK, Pletcher SD, Goldberg AN, McDermott M. Risk factors for cerebrospinal leak after endoscopic skull base reconstruction with nasoseptal flap. Otolaryngol Head Neck Surg. 2014. 151: 516-21
8. Hasegawa H, Shin M, Kondo K, Saito N. Reconstruction of Dural defects in endoscopic transnasal approaches for intradural lesions using multilayered fascia with a pressure-control spinal drainage system. World Neurosurg. 2018. 114: e1316-24
9. Hegazy HM, Carrau RL, Snyderman CH, Kassam A, Zweig J. Transnasal endoscopic repair of cerebrospinal fluid rhinorrhea: A meta-analysis. Laryngoscope. 2000. 110: 1166-72
10. Jho HD, Carrau RL. Endoscopy assisted transsphenoidal surgery for pituitary adenoma. Technical note. Acta Neurochir (Wien). 1996. 138: 1416-25
11. Jiam NT, David AP, Formeister EJ, Gurrola J 2nd, Aghi M, Theodosopoulos P. Presentation and management of post-operative cerebrospinal fluid leaks after sphenoclival expanded endonasal surgery: A single institution experience. J Clin Neurosci. 2021. 91: 13-9
12. Kawsar KA, Land T, Tsermoulas G, Paluzzi A, Ahmed S. Novel surgical treatment of recurrent CSF leak by temporoparietal temporalis myofascial flap: A series of 6 cases. World Neurosurg. 2021. 147: 1-6
13. Khan DZ, Ali AM, Koh CH, Dorward NL, Grieve J, Horsfall HL. Skull base repair following endonasal pituitary and skull base tumour resection: A systematic review. Pituitary. 2021. 24: 698-713
14. Lee JJ, Kim HY, Dhong HJ, Chung SK, Kong DS, Nam DH. Delayed cerebrospinal fluid leakage after treatment of skull base tumors: Case series of 9 patients. World Neurosurg. 2019. 132: e591-8
15. Ozawa H, Sekimizu M, Saito S, Nakamura S, Mikoshiba T, Watanabe Y. Risk factors for cerebrospinal fluid leak after endoscopic endonasal skull base surgery: A single-center experience. Acta Otolaryngol. 2021. 141: 621-5
16. Patel MR, Stadler ME, Snyderman CH, Carrau RL, Kassam AB, Germanwala AV. How to choose? Endoscopic skull base reconstructive options and limitations. Skull Base. 2010. 20: 397-404
17. Sørensen LT. Wound healing and infection in surgery. The clinical impact of smoking and smoking cessation: A systematic review and meta-analysis. Arch Surg. 2012. 147: 373-83
18. Soudry E, Turner JH, Nayak JV, Hwang PH. Endoscopic reconstruction of surgically created skull base defects: A systematic review. Otolaryngol Head Neck Surg. 2014. 150: 730-8
19. Spitaels J, Moore J, Zaidman N, Arroteia IF, Appelboom G, Barrit S. Fibrin-coated collagen fleece versus absorbable Dural sealant for sellar closure after transsphenoidal pituitary surgery: A comparative study. Sci Rep. 2022. 12: 7998
20. Zhou Z, Zuo F, Chen X, Zhao Q, Luo M, Jiang X. Risk factors for postoperative cerebrospinal fluid leakage after transsphenoidal surgery for pituitary adenoma: A meta-analysis and systematic review. BMC Neurol. 2021. 21: 417
21. Zwagerman NT, Wang EW, Shin SS, Chang YF, Fernandez-Miranda JC, Snyderman CH. Does lumbar drainage reduce postoperative cerebrospinal fluid leak after endoscopic endonasal skull base surgery? A prospective, randomized controlled trial. J Neurosurg. 2019. 131: 1172-8