- Department of Neurosurgery, Maastricht University Medical Centre, Maastricht, the Netherlands, Netherlands,
- Department of Radiology, King Fahad Hospital of Imam Abdulrahman Bin Faisal University, AL-Khobar, Saudi Arabia.
Correspondence Address:
Yasin Temel
Department of Neurosurgery, Maastricht University Medical Centre, Maastricht, the Netherlands, Netherlands,
DOI:10.25259/SNI-213-2019
Copyright: © 2019 Surgical Neurology International This is an open-access article distributed under the terms of the Creative Commons Attribution-Non Commercial-Share Alike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Mohammed Alahmari, Yasin Temel. Skull base chordoma treated with proton therapy: A systematic review. 07-Jun-2019;10:96
How to cite this URL: Mohammed Alahmari, Yasin Temel. Skull base chordoma treated with proton therapy: A systematic review. 07-Jun-2019;10:96. Available from: https://surgicalneurologyint.com/surgicalint-articles/9354/
Abstract
Background:Chordoma located in the skull base is usually a challenging surgical condition. It is often not possible to achieve gross total resection. Residual tumors have been treated with adjuvant focal radiation therapy employing high-energy particles most commonly through proton beam. In this review, we systematically analyzed indications and outcomes of this treatment with respect to local control rates of the lesion and factors determining recurrence of skull base chordomas. In addition, we collected data on treatment-associated radiation-induced side effects.
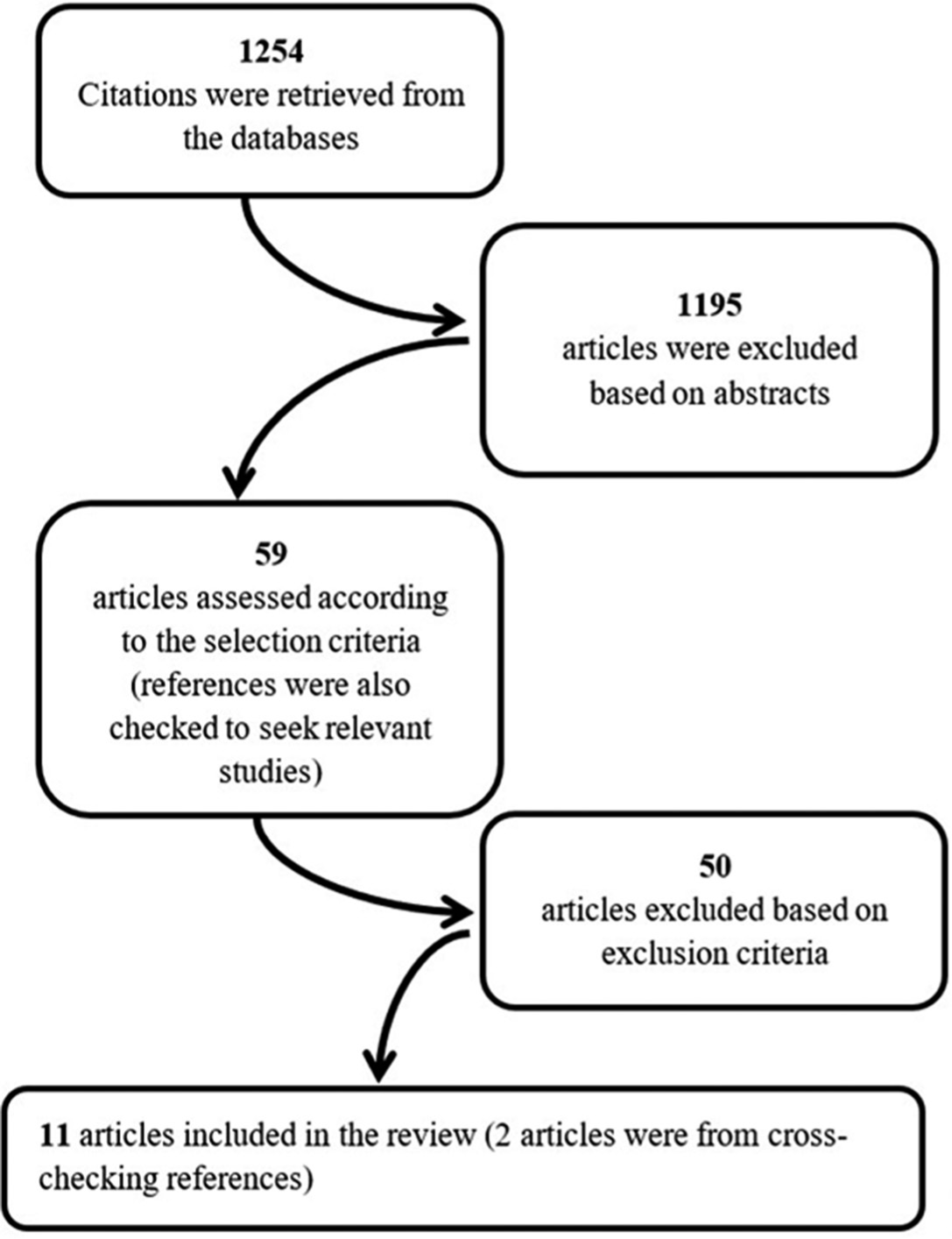
Methods:In line with the PRISMA guidelines, the authors performed a literature search algorithm for relevant articles using three databases: PubMed, Embase, and Cochrane. Inclusion and exclusion criteria were applied to evaluate all identified studies published between 1980 and 2018.
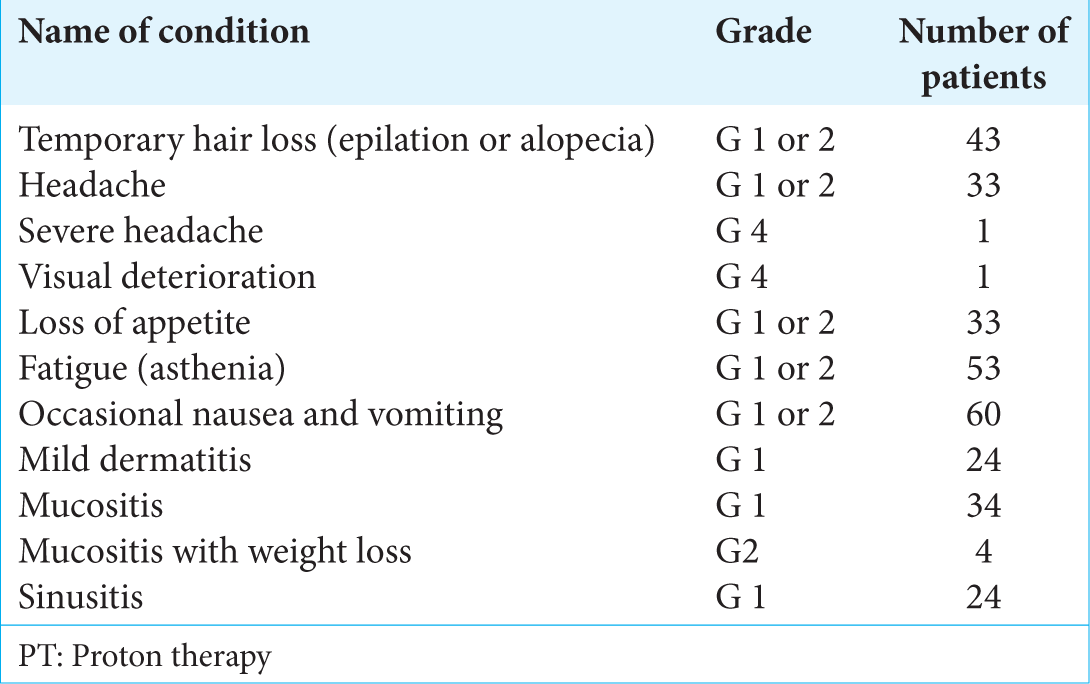
Results:Our review included 11 studies for analysis (n = 511 patients). The mean age of the study population was 47.3 ± 5.8 years. The mean dose of postsurgical irradiation at the time of initial treatment was 71.1 ± 3.1 Gy. The mean follow-up duration was 45.0 ± 17.5 months. Within this follow-up duration, recurrence occurred in 26.8% of the patients. The mean time to recurrence was 34.5 ± 15.2 months. A significant number of patients experienced side effects varying from Grade 1 (mild dermatitis) to Grade 4 (temporal lobe necrosis and visual disorders).
Conclusion:Despite advances in proton therapy, recurrence rates in skull base chordoma remain high. The toxicity of proton therapy may be more prevalent than generally thought. Unfortunately, there is substantial variation in the methods of data reporting.
Keywords: Analysis, Chordoma, Proton, Recurrence, Safety, Skull base
INTRODUCTION
Cranial chordoma is a rare skull neoplasm which is thought to arise from remnants of the embryonic notochord. It represents about 1%–4% of primary bone tumors.[
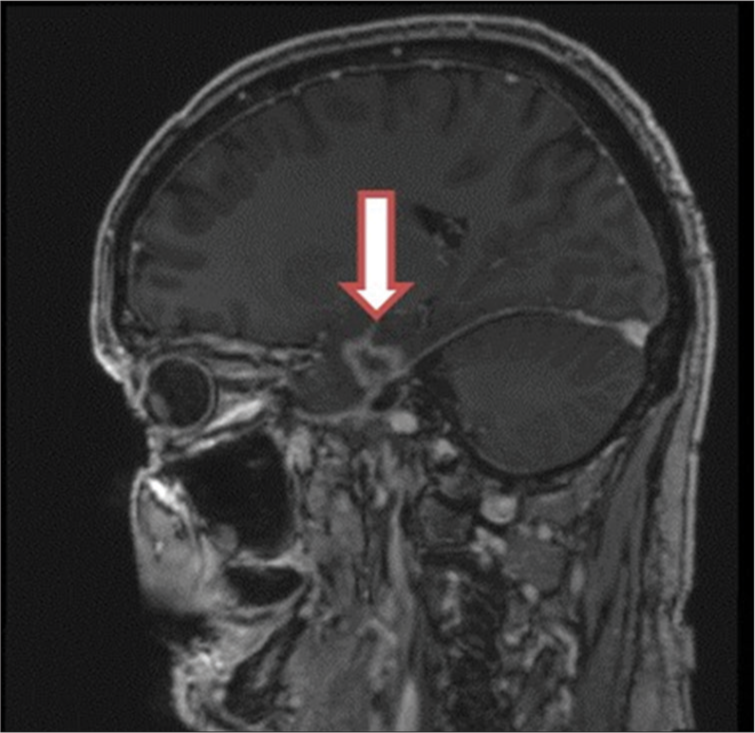
Skull base chordomas destroy bone and infiltrate to adjacent soft tissue. Neural and vascular structures such as cranial nerves, brainstem, carotid, and basilar artery can be compressed and/or encased by the expanding tumor. Since chordomas have no distinctly formed fibrous capsule, it is frequently difficult to identify tumor margins on magnetic resonance images.[
Subtotal resections are, therefore, common and residual tumors are meant to be treated by radiation therapy.[
Over the past few years, more information has become available on the effects of PT in patients with residual skull base chordomas. After PT, progression of residual tumor is often observed. In this review, we systematically analyzed the details of recurrence of skull base chordomas after PT therapy and collected data on side effects.
METHODS
We performed a literature search for relevant articles using three databases: PubMed, Embase, and Cochrane. The search covered English language publications between 1980 and 2018 (the last search was conducted on January 8, 2018). The strategy and keywords used for the search were [(Chordoma*)] AND [(Proton) OR (Particles)] AND [(Radiotherapy) OR (Therapy) OR (Beam)]. Inclusion criteria were peer-reviewed original articles in patients reporting the recurrence of skull base chordoma who had undergone PT and/or combined photon-PT after surgery. The exclusion criteria were single case studies, review articles, abstracts, animal or phantom studies, questionnaires, and pediatric studies. In case of possible double reporting of patients by the same research groups in different publications, we included the report with the highest sample size and/or longest follow-up period. Authors’ names, characteristics of patients, period, and place of treatment were all cross-checked. Papers not reporting recurrence were excluded. Furthermore, some studies included different groups of patients who had received different types of radiation therapy. Hence, if recurrence was reported as overall without considering the type of radiation therapy, the paper was excluded as well.
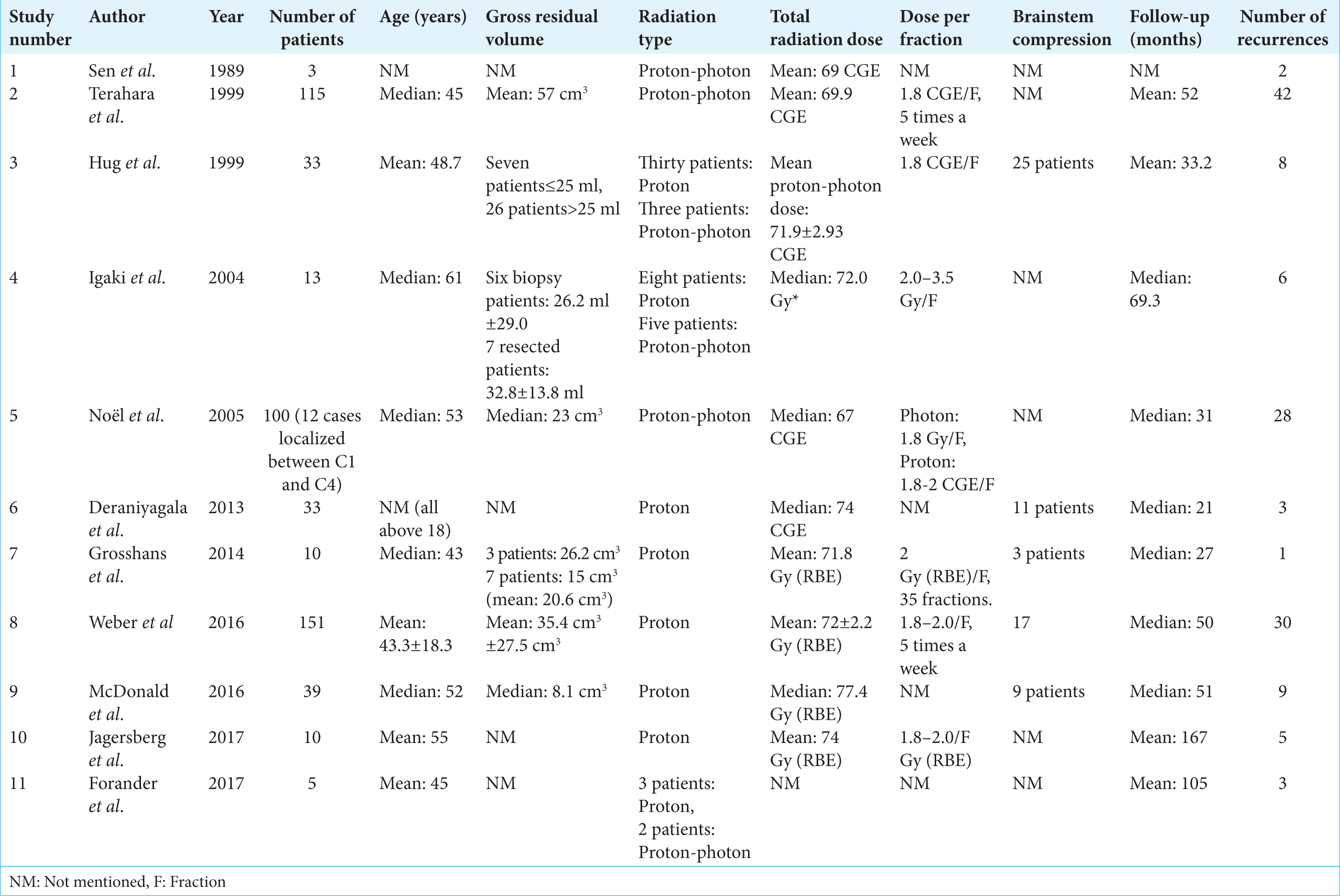
The following details were extracted from the included papers: authors, year of publication, number of patients, gender, age, follow-up period, type of radiation therapy, volume of residual tumor postsurgery, radiation dose applied, dose per fraction, radiation-induced side effects, rate of recurrences, number of deaths, and control rates. The variations found in units of PT dosage were kept as reported. The dosage of PT in old studies is usually expressed as cobalt gray equivalent (CGE) units, which is a factor of 1.1 compared to photon dose (60Co). Recent reports used the units of Gy RBE (with 1.1 relative to that of 60Co) more frequently as required by the International Commission on Radiation Units and Measurements.[
Data presentation
Eleven studies qualified for the final overall analysis. These studies will be briefly discussed in the next paragraphs. All mean values and standard deviations were analyzed using the IBM Statistical Package for the Social Science software, version 24.
RESULTS
First, we will provide a summary of included papers. These studies are described chronologically. Then, we will describe the results of the overall analysis.
1980–1989
In 1989, Sen et al. published on the treatment of eight patients with skull base chordoma.[
1990–1999
In 1999, Terahara et al. described the outcome of 115 patients with skull base chordomas.[
In the same year, another group described the results of their treatment of 33 chordoma patients.[
2000–2009
In 2004, Igaki et al. evaluated 13 cases of skull base chordomas who underwent either combined proton-photon therapy or PT alone.[
Recurrences were noticed more frequently in females than in males. Patterns of failure were local recurrences outside the clinical target volumes in two patients, local recurrence at dose-limited regions near radiation-sensitive structures in two patients, and in-field local recurrence within the gross tumor volume in one patient as well as out-of-field regional nodal recurrence in one patient.
In 2005, Noël. et al. reported their data of 100 irradiated patients with chordomas in the base of the skull or upper cervical spine.[
2010–2017
In 2013, Deraniyagala et al. published their results of a cohort of 33 chordoma patients who had undergone adjuvant PT with a mean dose of 78.4 CGE.[
Grosshans et al. published, in 2014, the results of 15 patients who were treated by PT following surgery.[
In 2016, Weber et al. reported the outcome of utilizing PT in 151 cases of skull base chordomas.[
In the same year, McDonald et al. demonstrated that larger residual tumors and tumors receiving a lower dose were associated with poor control.[
In 2017, Jägersberg et al. published the analysis of 13 skull base chordomas treated between 2005 and 2015.[
Another recent study described the treatment of 22 clival chordomas.[
Overall statistical analysis
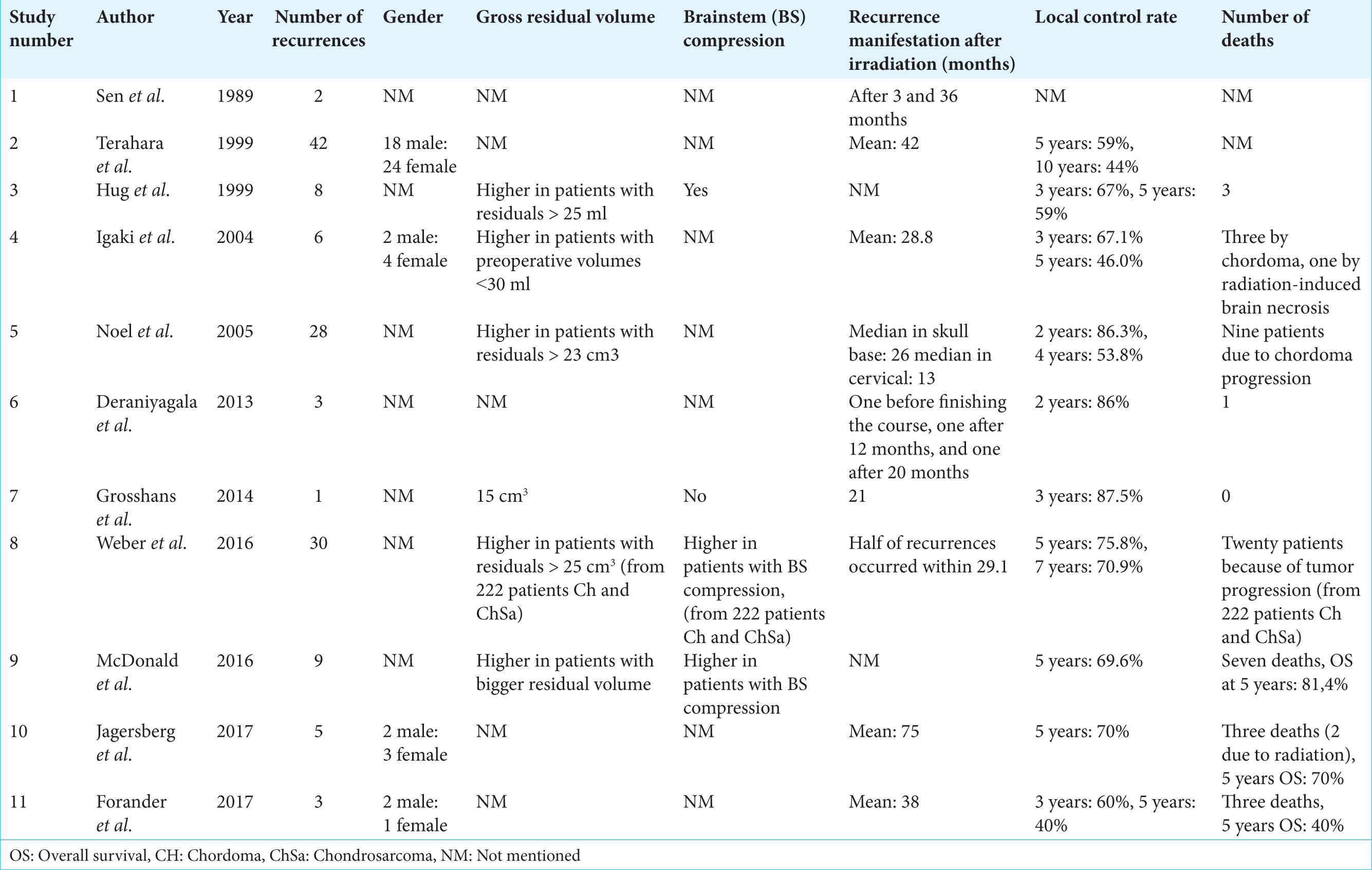
Our review resulted in a total of 511 patients which could be included for pooled analysis. The mean age of the study population was 47.3 ± 5.8 years. The mean dose of irradiation was 71.1 ± 3.1 Gy (RBE). The mean follow-up duration was 45.0 ± 17.5 months. Within this follow-up duration, recurrence was reported in 137 patients (26.8%). The mean time to recurrence was 34.5 ± 15.2 months. Forty-seven patients died due to their chordoma, and three deaths found to be due to radiation-induced side effects. From the dataset collected, we could not reconstruct a Kaplan–Meier plot illustrating local control rate. This is largely due to the lack of a given end time which is required for any survival analysis and which was missing here for individual patients in whom no recurrences were reported. Too many missing observations made it impossible to compute the Chi-squared contingency test to test for associations between recurrence and either the gross residual tumor volume, radiotherapy type, radiation dose, or gender.
Included studies and radiotherapy approach
Chordoma recurrence
The incidences of chordoma recurrence are presented in
Studies reporting on radiation-induced side effects
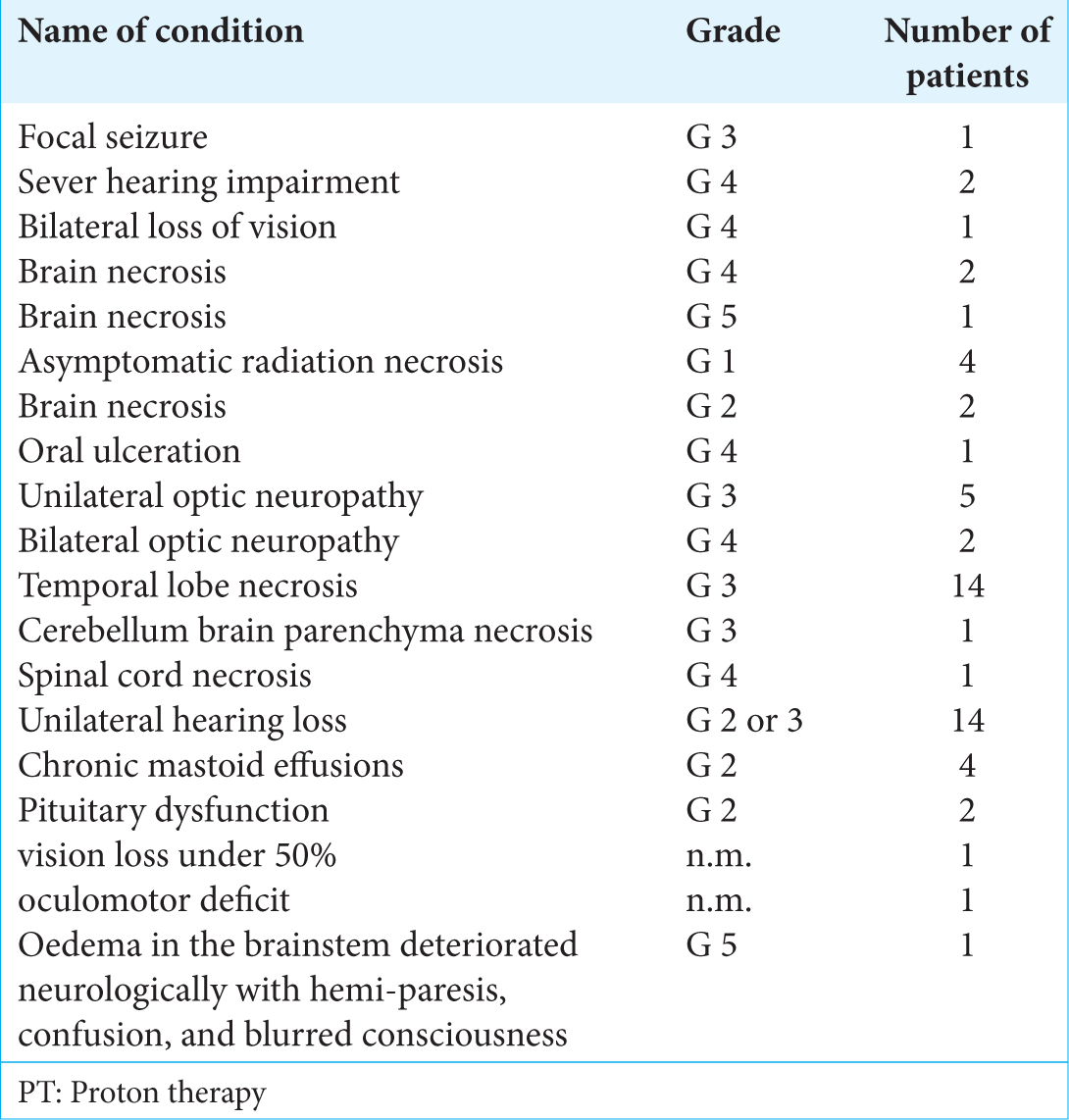
A summary of the reported acute and late radiation-induced effects, number of occurrences, and their toxicity grading levels are shown in
DISCUSSION
This study confirms that radiation therapy of skull base chordomas suffers from high recurrence rates despite high-intensity treatments.[
The reported local control rate at 5 years after surgery and either combined therapy or PT alone ranges between 40% and 75.8%.[
As an alternative to PT, modern technology in conformal photon irradiation can offer encouraging control rates which can be compared with those reported by PT. The intensity-modulated radiotherapy (IMRT) and image-guided radiotherapy (IGRT) are developed to escalate, shape, and deliver the respective dose more effectively and more conformally toward the targeted disease.[
The phenomenon of Bragg peak in PT has generated the hypothesis of minimizing treatment-related side effects. This assumption will be tested more thoroughly now with the increase in a number of available PT facilities. The question arises whether secondary malignant neoplasms can occur. The current follow-up durations are insufficient to answer this question, and longer follow-up data are required (at least 10–15 years after treatment).[
We summarized the most frequently observed acute toxicities (Grade 1 or 2) within the duration of 6 months after PT. These included nausea and vomiting, fatigue, temporary hair loss, mucositis, headache, and loss of appetite [
Of note, during the review process, we have encountered difficulties which may limit the interpretation of our data. First, in some of the early studies, protons were combined with photon-based radiation. Second, missing data and not reporting data systematically limit performing a more extensive analysis.
CONCLUSION
Despite advances in PT, recurrence rates in skull base chordoma remain high. The toxicity of PT may be more prevalent than generally thought.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors are grateful to Mr. Gil Stevenson for his support in the analysis of the data.
References
1. Ahmed SK, Brown PD, Foote RL. Protons vs photons for brain and skull base tumors. Semin Radiat Oncol. 2018. 28: 97-107
2. al-Mefty O, Borba LA. Skull base chordomas: A management challenge. J Neurosurg. 1997. 86: 182-9
3. Amichetti M, Amelio D, Minniti G. Radiosurgery with photons or protons for benign and malignant tumours of the skull base: A review. Radiat Oncol. 2012. 7: 210-
4. Ares C, Hug EB, Lomax AJ, Bolsi A, Timmermann B, Rutz HP. Effectiveness and safety of spot scanning proton radiation therapy for chordomas and chondrosarcomas of the skull base: First long-term report. Int J Radiat Oncol Biol Phys. 2009. 75: 1111-8
5. Barnett GC, West CM, Dunning AM, Elliott RM, Coles CE, Pharoah PD. Normal tissue reactions to radiotherapy: Towards tailoring treatment dose by genotype. Nat Rev Cancer. 2009. 9: 134-42
6. Baskar R, Dai J, Wenlong N, Yeo R, Yeoh KW. Biological response of cancer cells to radiation treatment. Front Mol Biosci. 2014. 1: 24-
7. . 2009. Available from https://www.ctep.cancer.gov/protocoldevelopment/electronic_applications/ctc.htm#ctc 40. [Last cited on 2018 Jan 09].
8. Deraniyagala RL, Yeung D, Mendenhall WM, Li Z, Morris CG, Mendenhall NP. Proton therapy for skull base chordomas: An outcome study from the university of florida proton therapy institute. J Neurol Surg B Skull Base. 2014. 75: 53-7
9. Di Maio S, Rostomily R, Sekhar LN. Current surgical outcomes for cranial base chordomas: Cohort study of 95 patients. Neurosurgery. 2012. 70: 1355-60
10. Di Maio S, Yip S, Al Zhrani GA, Alotaibi FE, Al Turki A, Kong E. Novel targeted therapies in chordoma: An update. Ther Clin Risk Manag. 2015. 11: 873-83
11. Fagundes MA, Hug EB, Liebsch NJ, Daly W, Efird J, Munzenrider JE. Radiation therapy for chordomas of the base of skull and cervical spine: Patterns of failure and outcome after relapse. Int J Radiat Oncol Biol Phys. 1995. 33: 579-84
12. Fernandez-Miranda JC, Gardner PA, Snyderman CH, Devaney KO, Mendenhall WM, Suárez C. Clival chordomas: A pathological, surgical, and radiotherapeutic review. Head Neck. 2014. 36: 892-906
13. Fletcher CDM, Bridge JA, Hogendoorn P, Mertens F. WHO Classification of Tumours of Soft Tissue and Bone. IARC Press: Lyon. 2013. p. 328-329
14. Förander P, Bartek J, Fagerlund M, Benmaklouf H, Dodoo E, Shamikh A. Multidisciplinary management of clival chordomas; long-term clinical outcome in a single-institution consecutive series. Acta Neurochir (Wien). 2017. 159: 1857-68
15. Grosshans DR, Zhu XR, Melancon A, Allen PK, Poenisch F, Palmer M. Spot scanning proton therapy for malignancies of the base of skull: Treatment planning, acute toxicities, and preliminary clinical outcomes. Int J Radiat Oncol Biol Phys. 2014. 90: 540-6
16. Gui S, Zong X, Wang X, Li C, Zhao P, Cao L. Classification and surgical approaches for transnasal endoscopic skull base chordoma resection: A 6-year experience with 161 cases. Neurosurg Rev. 2016. 39: 321-32
17. Hug EB, Loredo LN, Slater JD, DeVries A, Grove RI, Schaefer RA. Proton radiation therapy for chordomas and chondrosarcomas of the skull base. J Neurosurg. 1999. 91: 432-9
18. Igaki H, Tokuuye K, Okumura T, Sugahara S, Kagei K, Hata M. Clinical results of proton beam therapy for skull base chordoma. Int J Radiat Oncol Biol Phys. 2004. 60: 1120-6
19. Jägersberg M, El Rahal A, Dammann P, Merkler D, Weber DC, Schaller K. Clival chordoma: A single-centre outcome analysis. Acta Neurochir (Wien). 2017. 159: 1815-23
20. Jian BJ, Bloch OG, Yang I, Han SJ, Aranda D, Parsa AT. A comprehensive analysis of intracranial chordoma and survival: A systematic review. Br J Neurosurg. 2011. 25: 446-53
21. Kano H, Iqbal FO, Sheehan J, Mathieu D, Seymour ZA, Niranjan A. Stereotactic radiosurgery for chordoma: A report from the north american gamma knife consortium. Neurosurgery. 2011. 68: 379-89
22. Lühr A, von Neubeck C, Krause M, Troost EGC. Relative biological effectiveness in proton beam therapy current knowledge and future challenges. Clin Transl Radiat Oncol. 2018. 9: 35-41
23. Luxton G, Petrovich Z, Jozsef G, Nedzi LA, Apuzzo ML. Stereotactic radiosurgery: Principles and comparison of treatment methods. Neurosurgery. 1993. 32: 241-59
24. McDonald MW, Linton OR, Calley CS. Dose-volume relationships associated with temporal lobe radiation necrosis after skull base proton beam therapy. Int J Radiat Oncol Biol Phys. 2015. 91: 261-7
25. McDonald MW, Linton OR, Moore MG, Ting JY, Cohen-Gadol AA, Shah MV. Influence of residual tumor volume and radiation dose coverage in outcomes for clival chordoma. Int J Radiat Oncol Biol Phys. 2016. 95: 304-11
26. McMaster ML, Goldstein AM, Bromley CM, Ishibe N, Parry DM. Chordoma: Incidence and survival patterns in the United States, 1973-1995. Cancer Causes Control. 2001. 12: 1-1
27. Munzenrider JE, Liebsch NJ. Proton therapy for tumors of the skull base. Strahlenther Onkol. 1999. 175: 57-63
28. Nath Sen C, Sekhar LN, Schramm VL, Janecka IP. Chordoma and chrondrosarcoma of the cranial base: An 8-year experience. Neurosurgery. 1989. 25: 931-41
29. Nikoghosyan AV, Karapanagiotou-Schenkel I, Münter MW, Jensen AD, Combs SE, Debus J. Randomised trial of proton vs. Carbon ion radiation therapy in patients with chordoma of the skull base, clinical phase III study HIT-1-study. BMC Cancer. 2010. 10: 607-
30. Noël G, Feuvret L, Calugaru V, Dhermain F, Mammar H, Haie-Méder C. Chordomas of the base of the skull and upper cervical spine. One hundred patients irradiated by a 3D conformal technique combining photon and proton beams. Acta Oncol. 2005. 44: 700-8
31. Noël G, Feuvret L, Ferrand R, Boisserie G, Mazeron JJ, Habrand JL. Radiotherapeutic factors in the management of cervical-basal chordomas and chondrosarcomas. Neurosurgery. 2004. 55: 1252-60
32. Noël G, Gondi V. Proton therapy for tumors of the base of the skull. Chin Clin Oncol. 2016. 5: 51-
33. Noël G, Habrand JL, Jauffret E, de Crevoisier R, Dederke S, Mammar H. Radiation therapy for chordoma and chondrosarcoma of the skull base and the cervical spine. Prognostic factors and patterns of failure. Strahlenther Onkol. 2003. 179: 241-8
34. Noël G, Habrand JL, Mammar H, Pontvert D, Haie-Méder C, Hasboun D. Combination of photon and proton radiation therapy for chordomas and chondrosarcomas of the skull base: The centre de protonthérapie D’orsay experience. Int J Radiat Oncol Biol Phys. 2001. 51: 392-8
35. Paganetti H. Relative biological effectiveness (RBE) values for proton beam therapy. Variations as a function of biological endpoint, dose, and linear energy transfer. Phys Med Biol. 2014. 59: R419-72
36. Pehlivan B, Ares C, Lomax AJ, Stadelmann O, Goitein G, Timmermann B. Temporal lobe toxicity analysis after proton radiation therapy for skull base tumors. Int J Radiat Oncol Biol Phys. 2012. 83: 1432-40
37. Sahgal A, Chan MW, Atenafu EG, Masson-Cote L, Bahl G, Yu E. Image-guided, intensity-modulated radiation therapy (IG-IMRT) for skull base chordoma and chondrosarcoma: Preliminary outcomes. Neuro Oncol. 2015. 17: 889-94
38. Smoll NR, Gautschi OP, Radovanovic I, Schaller K, Weber DC. Incidence and relative survival of chordomas: The standardized mortality ratio and the impact of chordomas on a population. Cancer. 2013. 119: 2029-37
39. Stacchiotti S, Sommer J. Building a global consensus approach to chordoma: A position paper from the medical and patient community. Lancet Oncol. 2015. 16: e71-83
40. Terahara A, Niemierko A, Goitein M, Finkelstein D, Hug E, Liebsch N. Analysis of the relationship between tumor dose inhomogeneity and local control in patients with skull base chordoma. Int J Radiat Oncol Biol Phys. 1999. 45: 351-8
41. Tzortzidis F, Elahi F, Wright D, Natarajan SK, Sekhar LN. Patient outcome at long-term follow-up after aggressive microsurgical resection of cranial base chordomas. Neurosurgery. 2006. 59: 230-7
42. Weber DC, Badiyan S, Malyapa R, Albertini F, Bolsi A, Lomax AJ. Long-term outcomes and prognostic factors of skull-base chondrosarcoma patients treated with pencil-beam scanning proton therapy at the paul scherrer institute. Neuro Oncol. 2016. 18: 236-43
43. Weber DC, Malyapa R, Albertini F, Bolsi A, Kliebsch U, Walser M. Long term outcomes of patients with skull-base low-grade chondrosarcoma and chordoma patients treated with pencil beam scanning proton therapy. Radiother Oncol. 2016. 120: 169-74
44. Weber DC, Rutz HP, Pedroni ES, Bolsi A, Timmermann B, Verwey J. Results of spot-scanning proton radiation therapy for chordoma and chondrosarcoma of the skull base: The paul scherrer institut experience. Int J Radiat Oncol Biol Phys. 2005. 63: 401-9
45. Yakkioui Y, van Overbeeke JJ, Santegoeds R, van Engeland M, Temel Y. Chordoma: The entity. Biochim Biophys Acta. 2014. 1846: 655-69