- Unit of Functional Neurosurgery, Stereotaxy and Radiosurgery, Mexico General Hospital, Mexico City, Mexico
- Department of Neuroscience and Psychophysiology, Anahuac University, Mexico City, Mexico
- Department of Neurosurgery, University Hospital of Cologne, Cologne, Germany
- Rehabilitation Clinic, Mexico General Hospital, Mexico City, Mexico
Correspondence Address:
José D. Carrillo-Ruiz
Unit of Functional Neurosurgery, Stereotaxy and Radiosurgery, Mexico General Hospital, Mexico City, Mexico
DOI:10.4103/sni.sni_258_17
Copyright: © 2017 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: José D. Carrillo-Ruiz, Pablo Andrade, Mary Fonseca, Fiacro Jiménez, María L. Montes-Castillo, Francisco Velasco. Three consecutive neurotomies in one patient for the treatment of spastic hemiplegia: Spinal, median, and foot toes common flexor. 01-Nov-2017;8:267
How to cite this URL: José D. Carrillo-Ruiz, Pablo Andrade, Mary Fonseca, Fiacro Jiménez, María L. Montes-Castillo, Francisco Velasco. Three consecutive neurotomies in one patient for the treatment of spastic hemiplegia: Spinal, median, and foot toes common flexor. 01-Nov-2017;8:267. Available from: http://surgicalneurologyint.com/surgicalint-articles/three-consecutive-neurotomies-in-one-patient-for-the-treatment-of-spastic-hemiplegia-spinal-median-and-foot-toes-common-flexor/
Abstract
Background:Neurotomies were one of the first procedures performed in the field of functional neurosurgery. Microstimulators and microscopes facilitate the performance of neurotomies to treat focal spasticity. This report shows how three different consecutive neurotomies were performed in one patient with chronic left upper/lower extremity spasticity.
Case Description:A 65-year-old male with intractable epilepsy underwent a right temporal lobectomy for seizure control. Postoperatively, he developed left upper/lower extremity spasticity attributed to a postoperative right internal capsule infarct. The severe spasticity persisted despite the administration of conventional drugs, rehabilitation efforts, and botulinic toxin injections. Three sequential selective neurotomies (e.g., spinal, median, and foot common flexor nerves) were next performed. Postoperatively, the neurotomies resulted in significant symptomatic long-term improvement, 6 years after spinal neurotomy, 7 years after median neurotomy, and 9 years after common flexor neurotomy. Spasticity scores diminished from 4 to 0 points on the Ashworth scale and from 4 to 0 points on the Held–Tardieu scale for each muscular region.
Conclusion:Multiple regional neurotomies were effective in the management of left-sided postoperative spasticity in a patient who underwent a temporal lobectomy for seizure control with a resultant postoperative right internal capsule infarct.
Keywords: Flexor common of the foot, hemiplegia, median nerve, neurotomy, spasticity, spinal nerve
INTRODUCTION
Neurotomy is defined as cutting peripheral or cranial nerves. It was originally described by Lorenz in 1897 to treat spastic adductors muscles. Neurotomies were one of the first procedures performed in the field of functional neurosurgery.
Improvement in surgical techniques has led to more neurotomies to treat focal spasticity. Supraselective neurotomies can now be performed as microstimulators can differentiate the motor from the sensitive nerve fibers and help differentiate spastic from healthy muscular tissue.[
This report shows how three different consecutive neurotomies performed in the same patient were utilized to treat left-sided spasticity (e.g., winged scapula, a flexed hand over the forearm, spastic claw foot) in a patient who underwent a temporal lobectomy for seizure control that resulted in an infarct of the internal capsule.
CASE REPORT
Clinical data
A 65-year-old male with a history of drug-resistant temporal epilepsy for 25 years underwent a right temporal lobectomy. Postoperatively, although the patient was seizure-free (e.g. with the addition of antiepileptic drugs), he developed a left-sided hemiplegia attributed to an infarct of the right internal capsule [documented on computed tomography (CT)]. Within 5 postoperative days, left-sided function began to return, and he was discharged 15 days later without further complications. Nevertheless, he developed a progressive pyramidal syndrome characterized by high-grade spasticity in the left upper and lower extremities that did not respond to anti-spasmodic medications (tizanidine 2 mg/day and baclofen 30 mg/day). He also received botulinic toxin injections at following three sites to treat spasticity: (1) lower extremity, a spastic claw foot with plantar pain; (2) upper extremity, a flexed hand; (3) high grade spastic “winged scapula” [
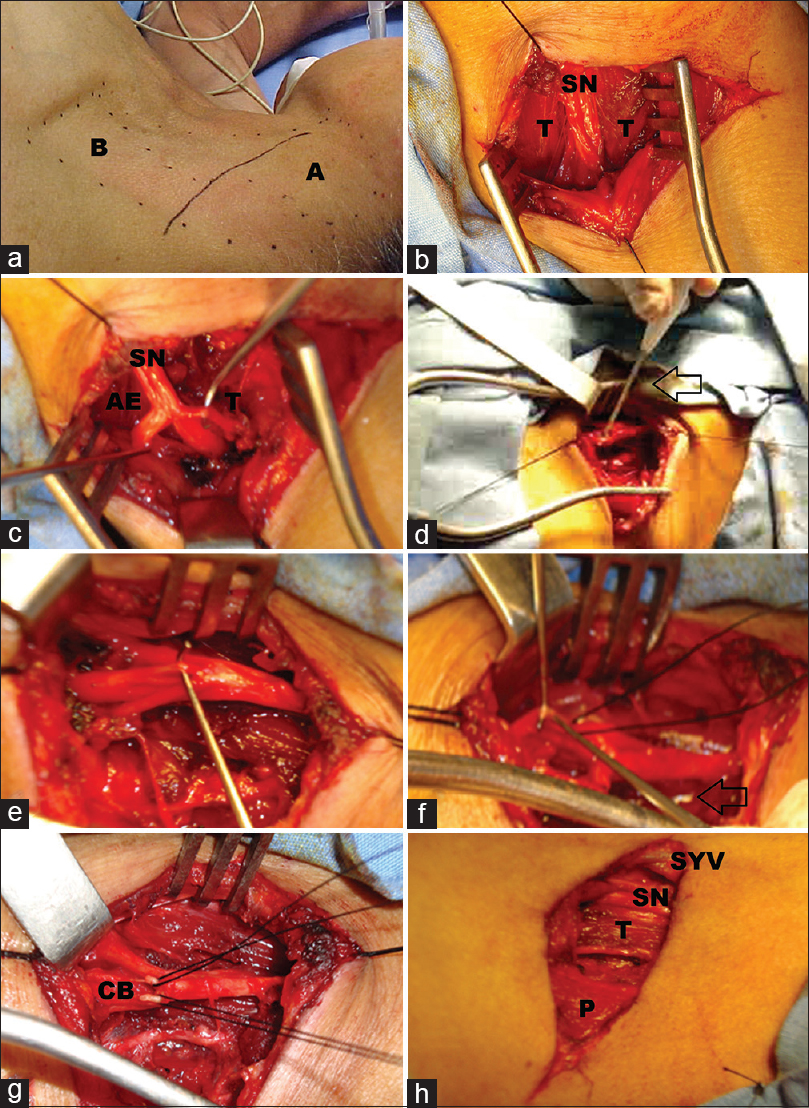
Figure 1
Presurgical and postsurgical evaluation. Clinical improvement after surgery: the upper pictures (a and b) correspond to the clinical presentation of claw fingers. On the left foot, an arrow shows the claw fingers before and after surgery. The lower pictures (c and d) indicate the clinical presentation before and after spinal neurotomy. On the left image, the patient presents an evident winged scapula, and on the right image (4 years after surgery) it shows a normal symmetry of the scapula
Surgery at three sites
Every procedure was indicated after a nerve test block with lidocaine (1%) was considered as positive. The patient ultimately underwent three neurotomies. Aneurotomy of the angle elevator of the scapula muscle was performed [
Figure 2
(a) Anterior (A) and posterior (B) neck triangles, crossed by an oblique line corresponding to the spinal nerve location. (b) Skin incision at the posterior triangle. Between the trapezoid (T) muscle fascicles, the spinal nerve (SN) at the beginning of the dissection. (c) The trapezoid muscle with the angular elevator of the scapula (AE) muscle. (d) Stimulation of the spinal nerve (arrow). (e, f) Dissection, traction, and cut-off the SN. (f) The arrow marks the scalpel during the neurotomy. (g) Sectioned by cut branches, to be harmonic with the figures abbreviations (CB). (h) At closure, the SN, T, superficial yugular vein (SYV) and platysma muscle (P)
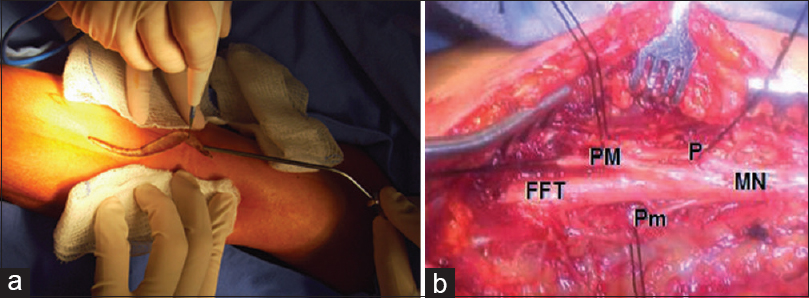
For the median nerve, each branch was exposed [pronator teres, palmar mayor, palmar minor, and the trunk of the muscular flexors (superficial and profound) of the hand [
Figure 3
Neurotomy of left median nerve. Left image (a) shows the longitudinal skin incision over the arm and forearm on the anterior face at the elbow level (observe the sinusoidal shape of the incision). Right image (b) demonstrates the dissection details of the surgery including the Median Nerve (MN) with its different nerve branches: P (pronator teres), Palmaris Mayor (PM), Palmaris minor (Pm), Fingers Flexor Trunk (FFT)
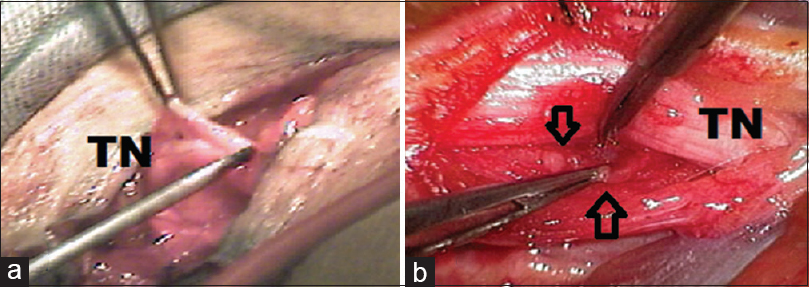
For the claw foot/toes spasticity, a tibial posterior neurotomy through a trans-popliteal incision [
Figure 4
Left foot fingers flexors nerves. Left image (a) exemplifies the dissection of the tibial posterior nerve trunk (TN) using a trans-popliteal approach (observe the isolation of its different divisions). Right image (b) illustrates the microscopic approach of the flexor branches dissection that are located deeper to the tibial nerve trunk (TN) and the dissection of them (arrows)
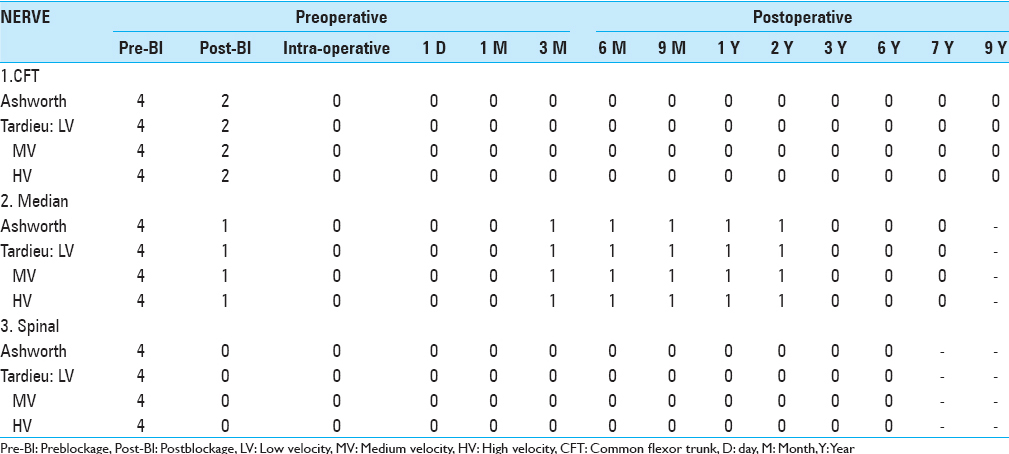
All neurotomies were performed on the left side using the same stimulation parameters to differentiate motor from sensitive nerves (5 Hz, 2–3 V with square pulses). The degree of spasticity was monitored intraoperatively, postoperatively, and at the following intervals; 1, 3, 6, 9, and 12 months, and up to 9 years postoperatively depending on the site of the surgery (for the spinal nerve 6 years, for the median nerve 7 years, and for the claw foot/toes 9 years). During this time, the patient's spasticity improved considerably according to the Ashworth and Tardieu scales [
DISCUSSION
The neurotomies performed in this patient were highly effective regarding the treatment of focal spasticity. According to previous literature, tibial posterior neurotomies reduced the varus and equinnus spastic position in approximately 82% of the cases over the long-term.[
Previously, Decq et al. reported the successful treatment of five hemiplegic patients with spasticity involving the shoulder and upper limb.[
Decq et al. also discussed performing neurotomies on the brachial plexus branches for spasticity of the shoulder in 5 patients, showing 86% improvement.[
Two main scales are used to assess spasticity; the Ashworth and Tardieu scales [
We can conclude that multiple consecutive neurotomies performed at crucially affected areas are a feasible alternative to treat high-grade hemiparesia.
Funding and Disclosure
This work did not receive any specific support from public funding agencies or commercial industries. The authors have no financial interests to disclose related to this article.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Carrillo-Ruiz JD, Andrade P, Godinez-Cubillos N, Montes-Castillo ML, Jiménez F, Velasco AL. Coupled obturator neurotomies and lidocaine intrathecal infusion to treat bilateral adductors spasticity and drug-refractory pain. J Neurosurgery. 2010. 113: 528-31
2. Decq P, Filipetti P, Feve A, Djindjian M, Saraoui A, Kéravel Y. Peripheral selective neurotomy of the brachial plexus collateral branches for treatment of the spastic shoulder: Anatomical study and clinical results of five patients. Neurosurgery. 1997. 4: 648-53
3. Decq P, Shin M, Carrillo-Ruiz J. Surgery in the peripheral nerves for lower limb spasticity. Oper Tech Neurosurg. 2004. 7: 136-46
4. Fukamachi K, Taira T, Kawasaki H, Hori T. Selective peripheral neurectomy of the median nerve for poststroke flexion spasticity of the hand. Stereotact Funct Neurosurg. 2000. 74: 223-4
5. Kim SH, Bae JH, Kim OL, Choi BY, Cho SH. Microsurgical selective peripheral neurotomy for focal spasticity. Stereotact Funct Neurosurg. 2000. 74: 224-
6. Maarrawi J, Mertens P, Luaute J, Vial C, Chardonnet N, Cosson M. Long-term functional results of selective peripheral neurotomy for the treatment of spastic upper limb: Prospective study in 31 patients. J Neurosurg. 2006. 104: 215-25
7. Sindou M, Abdennebi B, Sharkey P. Microsurgical selective procedures in peripheral nerves and the potential root spinal cord junction for spasticity. Appl Neurophysiol. 1985. 48: 97-104
8. Sindou M, Mertens P. Selective neurotomy of the tibial nerve for treatment of the spastic foot. Neurosurgery. 1988. 23: 738-44
9. Taira T, Hori T. The role of neurosurgical interventions for control of spasticity in neurorehabilitation: New findings on functional microanatomy of the tibial nerve. Acta Neurochir Suppl. 2003. 87: 103-5