- Department of Neurosurgery, Hospital Municipal Pimentas Bonsucesso, Guarulhos, Brazil
Correspondence Address:
Juliano Nery Navarro
Department of Neurosurgery, Hospital Municipal Pimentas Bonsucesso, Guarulhos, Brazil
DOI:10.4103/2152-7806.181982
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Navarro JN, Alves RV. Vertex epidural hematoma: A rare cause of post-traumatic headache and a diagnostic challenge. Surg Neurol Int 06-May-2016;7:
How to cite this URL: Navarro JN, Alves RV. Vertex epidural hematoma: A rare cause of post-traumatic headache and a diagnostic challenge. Surg Neurol Int 06-May-2016;7:. Available from: http://surgicalneurologyint.com/surgicalint_articles/vertex-epidural-hematoma-a-rare-cause-of-post-traumatic-headache-and-a-diagnostic-challenge/
Abstract
Background:Vertex epidural hematomas (VEH) account for only 8% of all epidural hematomas. However, these traumatic injuries may be underestimated or overlooked altogether when only computed tomography (CT) scans are used for diagnosis. The vertex may be a potential anatomic “blind spot” on this radiological method. In such cases, magnetic resonance (MRI) offers a great diagnostic aid.
Case Description:This manuscript reports a patient of a head trauma who developed progressive and intractable headache. MRI made the diagnosis of progressive VEH and highlighted the detachment of the superior sagittal sinus by the hematoma. Surgical treatment, because of the refractory clinical findings, was performed with good postoperative recovery.
Conclusion:Multiple trauma patients with progressive and refractory headache should have their head CT thoroughly reviewed and, if necessary, be investigated with MRI.
Keywords: Cranial epidural hematoma, cranial sutures, tomography
INTRODUCTION
Only 8% of all epidural hematomas are located at the cranial vertex, with a reported mortality rate of 50% if these lesions are misdiagnosed.[
CASE DESCRIPTION
Patient was a 28-year-old victim of multiple trauma caused by a high-energy automobile accident. In the emergency room, the patient was lucid (15 on Glasgow Coma Scale), with mild headache [1 on verbal numerical pain scale (VNS)] and without neurological deficits.
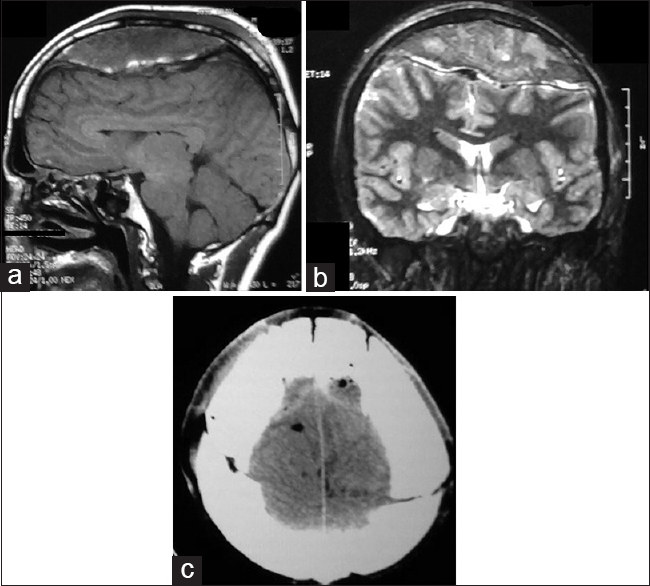
Because of the high kinetic energy of the trauma, a CT scan was performed [
Within 5 days following admission, the patient presented fluctuations in the pain's pattern and intensity, and on the sixth day, the pain became unbearable (9 on the VNS). Subsequently, a head MRI was performed which revealed the real magnitude of the VEH that was provoking extensive detachment of the superior sagittal sinus by the hematoma [Figure
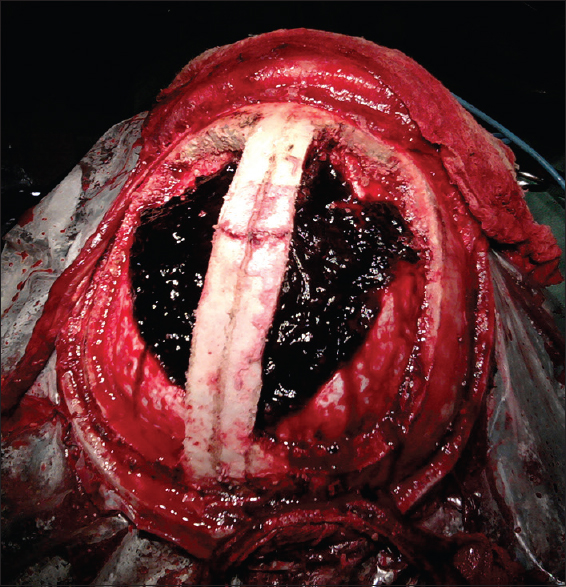
An emergency craniotomy was performed immediately for hematoma drainage. On the immediate postoperative day, the patient was asymptomatic and the CT showed complete evacuation of the hematoma [
DISCUSSION
The vertex hematoma is a potential “blind spot” on CT. It is difficult to diagnose because the hematoma is in near isodensity with the adjacent bone, the vertex may fall outside the scanning plane, and VEH may be relatively small to be detected by the CT.[
The extradural hematoma of the vertex overlies and compresses the superior sagittal sinus and venous lacunae. It compromises the venous drainage of the cerebral hemispheres superiorly, and impairs the absorption of the cerebrospinal fluid. Hence, such cases present mainly with features of intracranial hypertension.[
Miller et al. described that VEH may resolve spontaneously with time, and conservative treatment should be considered on a case-by-case basis.[
The surgery confirmed the extensive detachment of the superior sagittal sinus by the hematoma [
CONCLUSION
CT scans play a central role in the initial evaluation of traumatic brain injury patients. However, we must be aware of the possible tomographic “blind spots” and limitations of this method so that, if necessary, we can supplement this radiological investigation with other methods. VEH is a rare diagnosis, but potentially severe, that must be followed strictly.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Cikla U, Gürer B, Coskun I. Vertex epidural hematoma and triplegia. Neurol India. 2014. 62: 443-4
2. Datta SG. Bilateral vertex extradural hematomas: A case report. Indian J Neurotrauma. 2008. 5: 109-11
3. Harbury OL, Provenzale JM, Barboriak DP. Vertex epidural hematomas: Imaging findings and diagnostic pitfalls. Eur J Radiol. 2000. 36: 150-7
4. Jones TL, Crocker M, Martin AJ. A surgical strategy for vertex epidural haematoma. Acta Neurochir. 2011. 153: 1819-20
5. Lapadula G, Caporlingua F, Paolini S, Missori P, Domenicucci M. Epidural hematoma with detachment of the dural sinuses. J Neurosci Rural Pract. 2014. 5: 191-4
6. Miller DJ, Steinmetz M, McCutcheon IE. Vertex epidural hematoma: Surgical versus conservative management: Two case reports and review of the literature. Neurosurgery. 1999. 45: 621-4
7. Ramesh VG, Sivakumar S. Extradural hematoma at the vertex: A case report. Surg Neurol. 1995. 43: 138-9
8. Wylen EL, Nanda A. Vertex epidural hematoma with coronal suture diastasis presenting with paraplegia. J Trauma. 1998. 45: 413-5
9. Zuccarello M, Fiore DL, Trincia G, Pardatscher K, Andrioli GC. Epidural haematoma at the vertex. Acta Neurochir. 1982. 66: 195-206