- Department of Neurosurgery, Tokyo Rosai Hospital, Tokyo, Japan
- Department of Pathology, Tokyo Rosai Hospital, Tokyo, Japan
- Department of Neurosurgery, Tokyo Women's Medical University, Tokyo, Japan
Correspondence Address:
Taiichi Saito
Department of Neurosurgery, Tokyo Rosai Hospital, Tokyo, Japan
DOI:10.4103/2152-7806.159375
Copyright: © 2015 Saito T. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.How to cite this article: Saito T, Ujiie H, Kadoyama S, Higa T, Shiono S, Teramoto A. Brain metastasis from a lung mucoepidermoid carcinoma mimicking a brain abscess. Surg Neurol Int 25-Jun-2015;6:
How to cite this URL: Saito T, Ujiie H, Kadoyama S, Higa T, Shiono S, Teramoto A. Brain metastasis from a lung mucoepidermoid carcinoma mimicking a brain abscess. Surg Neurol Int 25-Jun-2015;6:. Available from: http://surgicalneurologyint.com/surgicalint_articles/brain-metastasis-from-a-lung-mucoepidermoid-carcinoma-mimicking-a-brain-abscess/
Abstract
Background:Mucoepidermoid carcinoma (MEC) is a rare tumor of the lung that accounts for 0.1–0.2% of all pulmonary tumors. To the best of our knowledge, brain metastasis from lung MEC is rare and magnetic resonance imaging (MRI) findings of this lesion have not been documented.
Case Description:We herein report the case of a 72-year-old male. MRI revealed a left parietal tumor showing ring enhancement with medium gadolinium contrast and an evident high intensity area in the nonenhanced central portion on diffusion-weighted images (DWI) mimicking a brain abscess. Histologically, MEC is composed of a mixture of different cell types including mucin-secreting glandular cells and squamous cells. Accordingly, we suggest that the high DWI signal can be explained by the development of intracellular and intraluminal mucin, which have a high viscosity.
Conclusion:Further accumulation of cases with brain metastasis from MEC is needed to establish the characteristic image findings, which would lead to prompt and adequate treatment.
Keywords: Brain metastasis, brain abscess, diffusion-weighted images, mucoepidermoid carcinoma
INTRODUCTION
Mucoepidermoid carcinoma (MEC) is not common in the lungs, accounting for only 0.1–0.2% of primary lung cancers.[
CASE REPORT
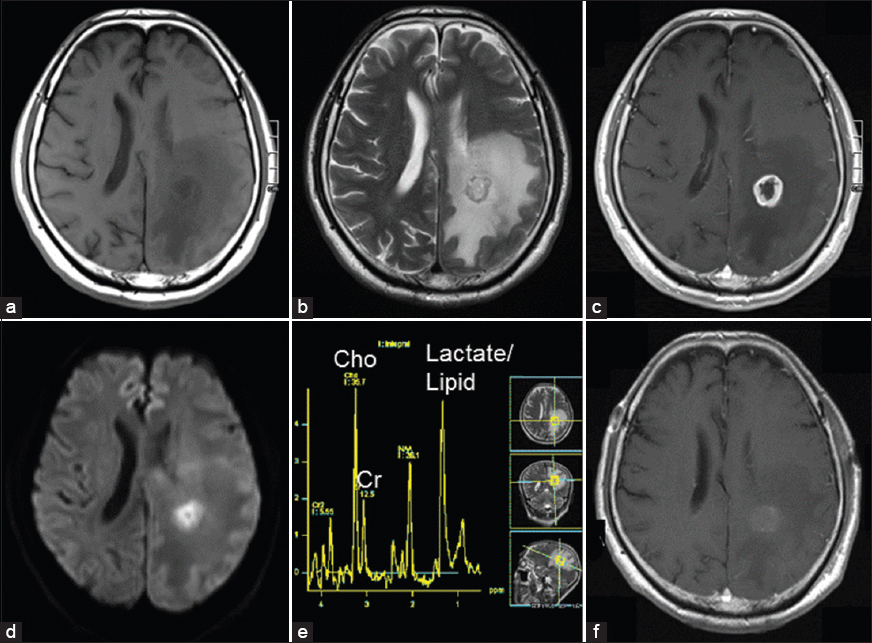
A 72-year-old male presented with numbness and slight motor weakness in the right upper and lower limbs. He also had finger agnosia, acalculia, and agraphia. He had smoked one pack of cigarette a day for 40 years. He did not have fever or leukocytosis (5900/μl), but his C-reactive protein level was slightly elevated (1.25 mg/dl). He was pointed out to have a 3 cm left parietal mass lesion on MRI. The outer part of the tumor showed an iso intensity area on T1-weighted images (T1WI) and T2-weighted images (T2WI), while the central part showed a low intensity area on T1WI and a high intensity area on T2WI [Figure
Figure 1
(a-e) MR images before the surgery demonstrating a tumor in the left parietal lobe. (a) The outer part of the tumor showed iso intensity, and the central part showed a low intensity area on T1-weighted imaging (T1WI). (b) The outer part of the tumor showed iso intensity, and the central part showed a high intensity area on T2-weighted imaging (T2WI). (c) The tumor had ring enhancement with gadolinium contrast medium on T1WI. (d) The central part of the tumor had a markedly high intensity area on diffusion-weighted imaging (DWI) (b = 1000 s/mm2). (e) On proton magnetic resonance spectroscopy, elevated lipid and lactate peaks were recognized. The choline peak was markedly elevated compared to the creatine peak. Cho: Choline. Cr: Creatine. (f) The tumor was confirmed to have been totally removed by postoperative MRI
The tumor was accompanied by wide perifocal edema on T2WI [
The patient underwent the removal surgery under general anesthesia. After left parietal craniotomy, we first made a test puncture into the mass lesion from the cortex of the left superior parietal lobule under ultrasonic guidance. We could not aspirate pus from the lesion, and thus ruled out a brain abscess. The tumor margin was demarcated, and the lesion was removed completely. The tumor was totally removed on postoperative MRI [
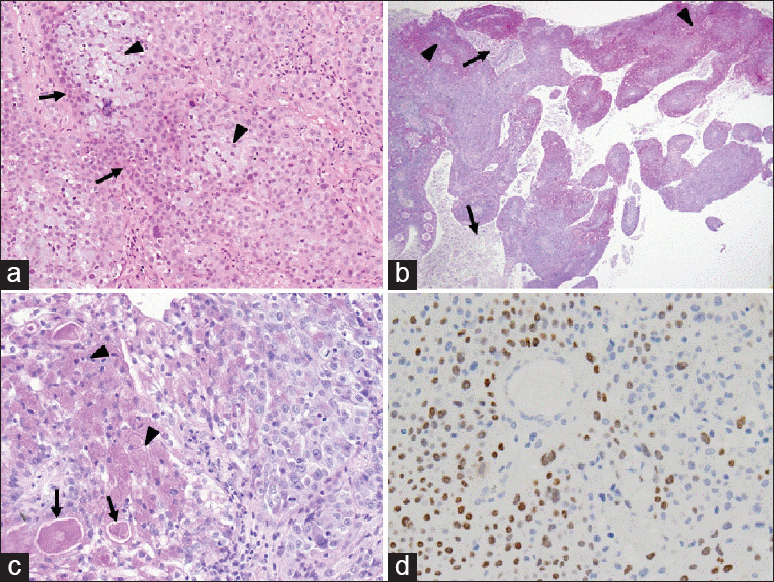
Figure 2
(a) Hematoxylin and eosin staining (×100). The tumor cells were predominantly arranged in sheets and small nests. The solid areas were composed of squamous epithelial (arrows), mucus-producing glandular (arrow heads) and intermediate cells. (b) PAS staining showed that the tumor had both necrotic (arrows) and solid mucin-positive areas (arrow heads) (×40). (c) PAS staining showed strong mucin positivity within the cytoplasm and intraluminal mucus (arrows) (×200). (d) Immunohistochemical staining of p40 showed nuclear positivity for the squamous cell component (×200)
DISCUSSION
We experienced a rare case of brain metastasis from lung MEC, which was difficult to differentiate from a brain abscess preoperatively, because this tumor showed an evident high intensity area in the central portion on DWI, which was not enhanced with gadolinium contrast medium. MEC is a rare tumor of the lungs arising from bronchial glands.[
The differential diagnosis of metastasis from a brain abscess can be difficult with a conventional MRI study. This is especially true in cases of suspected brain abscess, for which an immediate correct diagnosis is necessary to allow for prompt, adequate treatment, including the drainage of the central contents and administration of antibiotics. In prior reports, DWI and ADC values have been suggested to be useful for the differential diagnosis between abscesses and cystic or necrotic tumors.[
In contrast, Holtas et al. reported a brain metastasis from a lung adenocarcinoma with a central high signal on DWI and a low ADC value.[
In conclusion, brain metastasis from lung MEC is rare, and the MRI findings of these lesions are still unclear. However, our present case indicates that these lesions might show a high intensity area in the central portion on DWI mimicking a brain abscess. Although the incidence is very low, further accumulation of cases with brain metastasis from MEC will be needed to establish the characteristic image findings, which can lead to prompt and adequate treatment.
References
1. Al-Okaili RN, Krejza J, Wang S, Woo JH, Melhem ER. Advanced MR imaging techniques in the diagnosis of intraaxial brain tumors in adults. Radiographics. 2006. 26: S173-89
2. Duygulu G, Ovali GY, Calli C, Kitis O, Yunten N, Akalin T. Intracerebral metastasis showing restricted diffusion: Correlation with histopathologic findings. Eur J Radiol. 2010. 74: 117-20
3. Ebisu T, Tanaka C, Umeda M, Kitamura M, Naruse S, Higuchi T. Discrimination of brain abscess from necrotic or cystic tumors by diffusion-weighted echo planar imaging. Magn Reson Imaging. 1996. 14: 1113-6
4. Fink KR, Fink JR. Imaging of brain metastases. Surg Neurol Int. 2013. 4: S209-19
5. Hartmann M, Jansen O, Heiland S, Sommer C, Munkel K, Sartor K. Restricted diffusion within ring enhancement is not pathognomonic for brain abscess. AJNR Am J Neuroradiol. 2001. 22: 1738-42
6. Hayashida Y, Hirai T, Morishita S, Kitajima M, Murakami R, Korogi Y. Diffusion-weighted imaging of metastatic brain tumors: Comparison with histologic type and tumor cellularity. AJNR Am J Neuroradiol. 2006. 27: 1419-25
7. Holtas S, Geijer B, Stromblad LG, Maly-Sundgren P, Burtscher IM. A ring-enhancing metastasis with central high signal on diffusion-weighted imaging and low apparent diffusion coefficients. Neuroradiology. 2000. 42: 824-7
8. Leonardi HK, Jung-Legg Y, Legg MA, Neptune WB. Tracheobronchial mucoepidermoid carcinoma. Clinicopathological features and results of treatment. J Thorac Cardiovasc Surg. 1978. 76: 431-8
9. Park SH, Chang KH, Song IC, Kim YJ, Kim SH, Han MH. Diffusion-weighted MRI in cystic or necrotic intracranial lesions. Neuroradiology. 2000. 42: 716-21
10. Shen C, Che G. Clinicopathological analysis of pulmonary mucoepidermoid carcinoma. World J Surg Oncol. 2014. 12: 33-
11. Wolf KM, Mehta D, Claypool WD. Mucoepidermoid carcinoma of the lung with intracranial metastases. Chest. 1988. 94: 435-8