- Neurosurgical Service, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts, USA
Correspondence Address:
Christoph J. Griessenauer
Neurosurgical Service, Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, Massachusetts, USA
DOI:10.4103/2152-7806.191023
Copyright: © 2016 Surgical Neurology International This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.How to cite this article: Griessenauer CJ, Fusco MR, He L, Chua M, Sieber S, Mazketly AA, Reddy AS, Ogilvy CS, Thomas AJ. Dual diagnostic catheter technique in the endovascular management of anterior communicating artery complex aneurysms. Surg Neurol Int 21-Sep-2016;7:87
How to cite this URL: Griessenauer CJ, Fusco MR, He L, Chua M, Sieber S, Mazketly AA, Reddy AS, Ogilvy CS, Thomas AJ. Dual diagnostic catheter technique in the endovascular management of anterior communicating artery complex aneurysms. Surg Neurol Int 21-Sep-2016;7:87. Available from: http://surgicalneurologyint.com/surgicalint_articles/dual-diagnostic-catheter-technique-endovascular-management-anterior-communicating-artery-complex-aneurysms/
Abstract
Background:The configuration of the anterior communicating artery (AcomA) complex is important in the endovascular treatment of AcomA complex aneurysms. In cases of codominant anterior cerebral arteries (ACA), coil embolization may result in inadvertent occlusion of the contralateral ACA due to poor visualization. A second diagnostic catheter in the contralateral carotid artery may help with visualization of this angiographic blind spot. To our knowledge, the safety and efficacy of this dual diagnostic catheter technique have never been assessed.
Methods:A cohort of consecutive patients that underwent coil embolization of an AcomA complex aneurysm at a major academic institution in the United States between 2007 and 2014 were retrospectively reviewed.
Results:Eighty-two patients who had an AcomA complex aneurysm treated with coil embolization were identified. The dual diagnostic catheter technique was used in 17 (20.7%) patients. Aneurysms treated with the dual diagnostic catheter technique were less frequently ruptured and had less favorable dome-to-neck ratios as well as neck width for primary coil embolization. The rate of codominant ACAs was significantly higher and stent-assisted coil embolization was performed more frequently. The rate of thromboembolic complications, angiographic outcome, and retreatment did not differ between both the groups.
Conclusions:The dual diagnostic catheter technique is a safe and effective method during coil embolization of AcomA complex aneurysms and preferred for aneurysms with codominant ACAs, incorporation of either A1 or A2 segments into the aneurysm, and aneurysms with a wide neck and low dome-to-neck ratios.
Keywords: Aneurysm coiling, anterior communicating artery complex, stent-assisted coiling, subarachnoid hemorrhage
INTRODUCTION
Asymmetry of the circle of Willis is an important factor in the development of intracranial aneurysms and ischemic stroke, and patients with aneurysms are more likely to have asymmetry of the circle.[
PATIENTS AND METHODS
After approval from the Institutional Review Board (IRB) was obtained, a retrospective review of a prospectively maintained database of patients who underwent coil embolization of an AcomA complex aneurysm at a major academic institution in the United States from 2007 to 2014 was performed. The following information was collected: Patient characteristics (patient age, gender, history of subarachnoid hemorrhage), aneurysm characteristics (dome-to-neck ratio, neck width, Aspects ratio, aneurysm direction), ACA characteristics (dominance), treatment characteristics, including degree of obliteration according to the updated Raymond Roy classification,[
Technique
Initial access was obtained through the right common femoral artery and a 6 French (F) sheath was placed. Diagnostic angiography of both common carotid arteries were obtained. When the AcomA complex was codominant, either A1 or A2 segments incorporated into the aneurysm, and the aneurysms had wide neck and low dome-to-neck ratio, the dual diagnostic catheter technique was used. The side for intervention was based on which A1 segment appeared more robust. The contralateral femoral artery was accessed and a 4 F sheath was placed. A diagnostic catheter was placed into the contralateral, non-interventional common carotid artery and was connected to a heparinized-saline flush. Standard guide catheter access, three-dimensional rotational angiography, and aneurysm catheterization were obtained form the side of intervention. Anticoagulation was achieved using intravenous heparin given at the time of guide catheter access with a goal activated clotting time (ACT) of 250. During coil embolization, angiograms were periodically obtained from both the sides to assess the status of the A1 and A2 segment bilaterally. Following the intervention, the catheters were removed and the arteriotomy sites were closed with the vascular closure device.
Statistical analysis
Statistical analysis was performed using R version 3.1.1 (
RESULTS
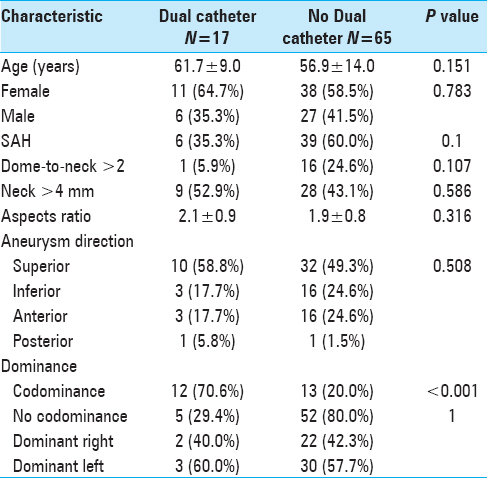
Eighty-two patients who had an AcomA complex aneurysm treated with coil embolization between 2007 and 2014 were identified. The dual diagnostic catheter technique was used in 17 (20.7%) patients [
Patient characteristics
Age (P = 0.151) and gender (P = 0.783) did not differ significantly both the groups. Aneurysms treated with the dual diagnostic catheter technique were less frequently ruptured (35.3% vs. 60%; P = 0.1) [
Aneurysm characteristics
Aneurysms treated with the dual diagnostic catheter technique were more complex and less favorable for primary coiling as indicated by lower dome to neck ratios (dome-to-neck >2; 5.9% vs. 24.6%; P = 0.107) and wider necks (neck >4 mm; 52.9% vs. 43.1%; P = 0.586). Aspects ratio (P = 0.316) and aneurysm direction (P = 0.508) were similar in both the groups [
Anterior cerebral artery characteristics
The dual diagnostic catheter group had a significantly higher rate of codominant ACAs (70.6% vs. 20%; P < 0.001) [
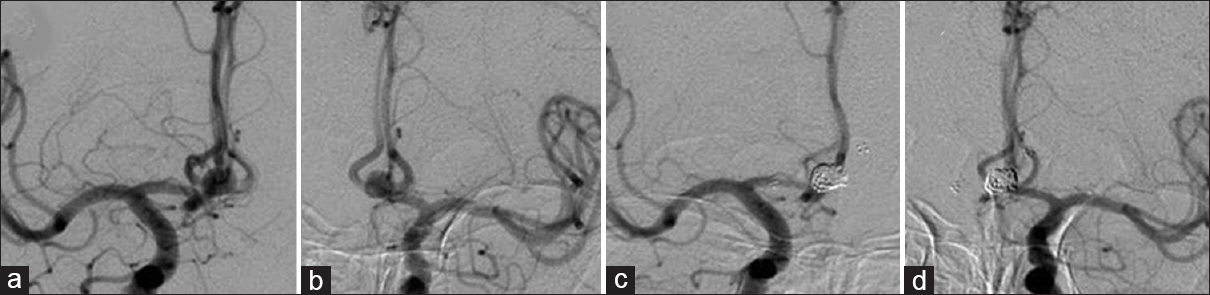
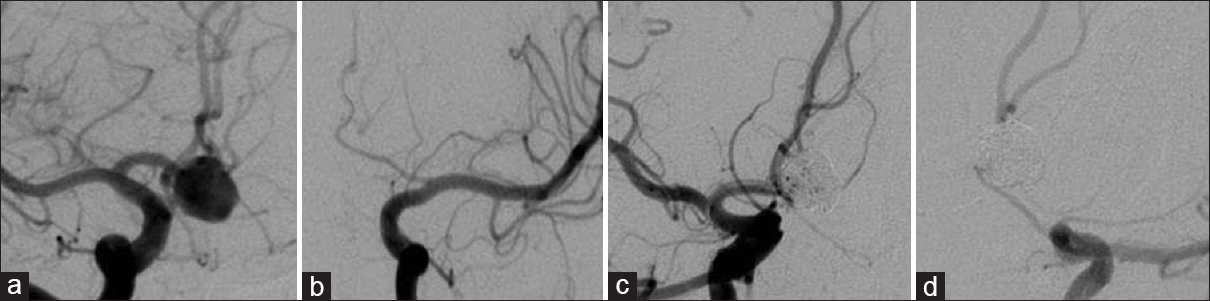
Figure 1
Angiographic evidence of codominant anterior cerebral arteries. Anteroposterior angiograms of right (Panel a) and left-sided (Panel b) injections demonstrate balanced filling of the AcomA complex and aneurysm. The dual diagnostic catheter technique was used. Injections from the side of intervention (right; Panel c) and contralateral side (left; Panel d) during coil embolization show the patency of the AcomA complex
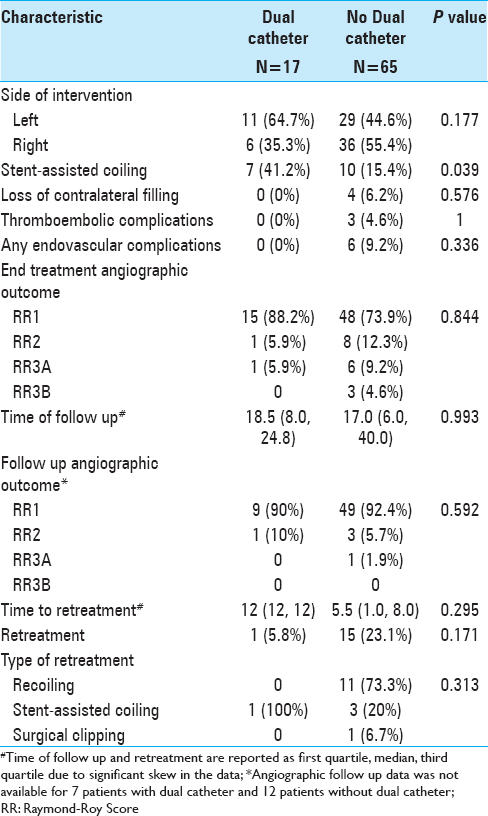
Treatment characteristics, complications, and follow up
Stent-assisted coil embolization was performed more frequently in the dual diagnostic catheter group (41.2 vs. 15.4%; P = 0.039). Loss of contralateral filling across the AcomA was noted in 6.2% of cases where the dual diagnostic catheter technique was not used. The rate of thromboembolic complications was comparable for both groups (4.6% vs. 0%, P = 1) and the dual diagnostic catheter technique was not associated with more frequent femoral artery access site complications. Angiographic outcome at the end of the procedure (P = 0.844), upon follow up (P = 0.592), and retreatment (P = 0.171) were comparable between both groups [
DISCUSSION
The use of a contralateral diagnostic catheter to visualize the angiographic blind spot during coil embolization of aneurysms of certain AcomA complex configurations is not to be confused with the dual microcatheter technique used to treat wide-necked aneurysms.[
The dual diagnostic catheter technique was used in approximately 20% of AcomA complex aneurysms treated in this series. In the majority of cases where the technique was used, the AcomA complex was codominant and the aneurysm had a less favorable dome-to-neck ratio for coil embolization, a wider neck, and a higher rate of stent-assisted coiling. While only the rate of codominant A1s and the use of stent-assisted coiling were statistically different compared to the AcomA complex aneurysm treated without a contralateral diagnostic catheter, the small sample size may have increased the potential for type II error or the inability to detect differences in the other variables. In a minority of cases without codominant ACAs, the dual diagnostic catheter technique was used when the A1/A2 junction was obscured during coil embolization.
Challenges of anterior communicating artery complex aneurysm treatment
AcomA complex aneurysms represent a unique challenge to both microsurgical clipping and endovascular coil embolization due to their complex and highly variable anatomy. Microsurgical clipping can be complicated by perforator injuries, particularly with superiorly or posteriorly projecting aneurysms. In addition, large aneurysms often obscure the visualization of bilateral A1 and A2 segments during clipping.[
Dual diagnostic catheter technique
Unless the A1 of the side of intervention is dominant and provides flow to both A2s, guide catheter angiography may only visualize the ipsilateral A2. To address this angiographic blind spot, a diagnostic catheter in the contralateral, non-interventional common carotid may help with visualization, particularly with codominant A1s, incorporation of the A2 origin in the aneurysm, or working views where the aneurysm overlaps with the contralateral A1/A2 junction. If the contralateral A1/A2 junction is demonstrated reliably using the dual diagnostic catheter technique, and minimal coil prolapse into the AComA complex occurs, one can proceed safely and confidently knowing both A2s are preserved [
Figure 2
A 76-year-old man presenting with subarachnoid hemorrhage from an AcomA complex aneurysm. The dual diagnostic catheter technique was used during balloon-assisted coil embolization. Anteroposterior angiograms of right (Panel a) and left-sided (Panel b) injections demonstrate right dominant filling of the AcomA complex and aneurysm. While the right-sided injection demonstrates filling of the left A2 segment, the A1/A2 junction is invariably obscured by the coil mass. Right-sided injection after conclusion of the aneurysm obscures the AcomA complex and no definitive filling of the left A2 is seen (Panel c). Left-sided injection demonstrates patency of the left A1/A2 junction (Panel d)
There was no added risk with the use of the dual diagnostic catheter technique. No complications occurred in cases where the second catheter was used. With respect to end treatment result, need for retreatment, and long-term outcome, the results with the dual diagnostic catheter technique were comparable to cases where the technique was not used.
Limitations
The main limitation is the inability to perform a genuine head-to-head comparison of both techniques as the dual diagnostic catheter technique is inherently preferred for more complex AcomA complex aneurysms. Aneurysms treated with the dual diagnostic catheter technique in the present study had less favorable dome-to-neck ratio and neck width for primary coil embolization resulting in a higher rate of stent-assisted coiling. Another limitation is the small number of patients because it limits the power of the study.
CONCLUSION
To our knowledge, the safety and efficacy of the dual diagnostic catheter technique have not been previously assessed. We conclude that the technique is safe and effective and preferred for aneurysms with codominant ACAs, incorporation of either A1 or A2 segments into the aneurysm, and aneurysms with a wide neck and low dome-to-neck ratios.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Abla AA, Lawton MT. Anterior cerebral artery bypass for complex aneurysms: An experience with intracranial-intracranial reconstruction and review of bypass options. J Neurosurg. 2014. 120: 1364-77
2. Brisman JL, Song JK, Newell DW. Cerebral aneurysms. N Engl J Med. 2006. 355: 928-39
3. Hendrikse J, van Raamt AF, van der Graaf Y, Mali WP, van der Grond J. Distribution of cerebral blood flow in the circle of Willis. Radiology. 2005. 235: 184-9
4. Hoksbergen AW, Legemate DA, Csiba L, Csáti G, Síró P, Fülesdi B. Absent collateral function of the circle of Willis as risk factor for ischemic stroke. Cerebrovasc Dis Basel Switz. 2003. 16: 191-8
5. Horowitz M, Gupta R, Jovin T. The dual catheter technique for coiling of wide-necked cerebral aneurysms. An under-reported method. Interv Neuroradiol J Peritherapeutic Neuroradiol Surg Proced Relat Neurosci. 2005. 11: 155-60
6. Kwon OK, Kim SH, Kwon BJ, Kang HS, Kim JH, Oh CW. Endovascular treatment of wide-necked aneurysms by using two microcatheters: Techniques and outcomes in 25 patients. AJNR Am J Neuroradiol. 2005. 26: 894-900
7. Mascitelli JR, Moyle H, Oermann EK, Polykarpou MF, Patel AA, Doshi AH. An update to the Raymond-Roy Occlusion Classification of intracranial aneurysms treated with coil embolization. J Neurointerventional Surg. 2015. 7: 496-502
8. Osborn AG.editorsDiagnostic cerebral angiography. Philadelphia: Lippincott Williams and Wilkins; 1999. p.
9. Piotin M, Blanc R. Balloons and stents in the endovascular treatment of cerebral aneurysms: Vascular anatomy remodeled. Front Neurol. 2014. 5: 41-
10. Piotin M, Blanc R, Spelle L, Mounayer C, Piantino R, Schmidt PJ. Stent-assisted coiling of intracranial aneurysms: Clinical and angiographic results in 216 consecutive aneurysms. Stroke J Cereb Circ. 2010. 41: 110-5
11. Raymond J, Roy D. Safety and efficacy of endovascular treatment of acutely ruptured aneurysms. Neurosurgery. 1997. 41: 1235-45
12. Rhoton AL, Saeki N, Perlmutter D, Zeal A. Microsurgical anatomy of common aneurysm sites. Clin Neurosurg. 1979. 26: 248-306
13. Starke RM, Durst CR, Evans A, Ding D, Raper DM, Jensen ME. Endovascular treatment of unruptured wide-necked intracranial aneurysms: Comparison of dual microcatheter technique and stent-assisted coil embolization. J Neurointerventional Surg. 2015. 7: 256-61